Forums › Erbium Lasers › General Erbium Discussion › When are two lasers needed
- This topic is empty.
-
AuthorPosts
-
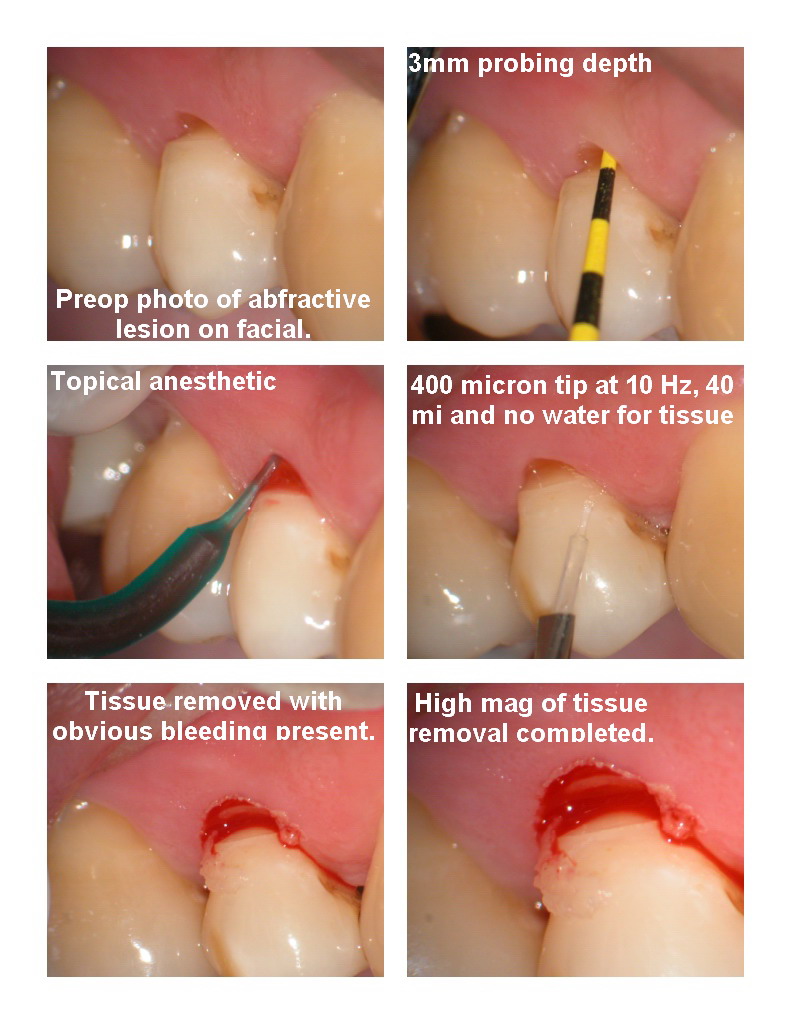
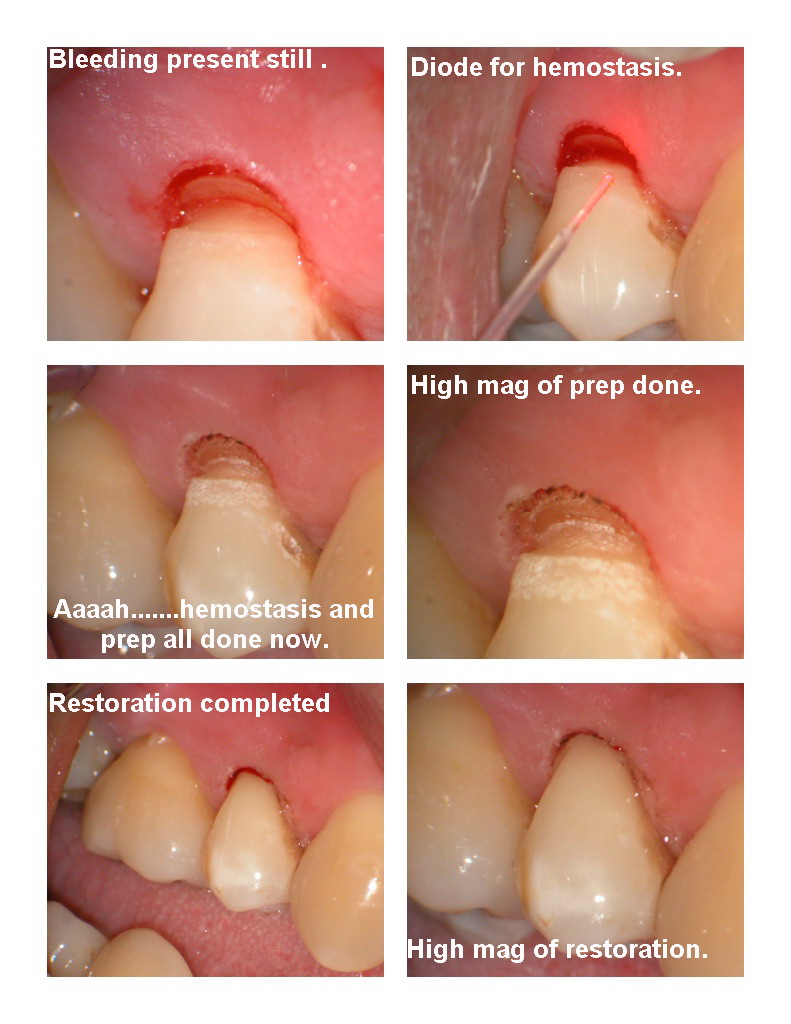
Glenn van AsSpectatorSometime even with a best guess you find a patient who bleeds more even in supposedly healthy tissue. I did this case all without anesthetic which can be tough with the hotter diode laser but we managed.
The abfractive lesion as noted preoperatively was subgingival so we tried to remove some soft tissue with the erbium laser at 10Hz, 4omj and air only as the patient was quite nervous. Got it done but there was a ton of bleeding present so we decided to get the diode out.
15Hz and 800 milliwatts in contact and we were able to get it to stop. I tried in uninitiated fashion first , not alot of luck so initiated the tip and then managed to get coagulation.
The topical is Ultracare in Ultradent syringe and the final restoration was Point 4 opaque which I like for the Class Vs as it is opaque , doesnt run and works for me quite well.
Hope you like it………
Glenn
SwpmnSpectatorNice case and your findings concur with those of my own. The erbium lasers will remove the soft tissue efficiently but not provide very good hemostasis. If you have a diode laser it will control the hemorrhage and this can be done without local anesthetic when a low energy setting such as the one reported is selected.
Al
Glenn van AsSpectatorCome on Allen……..give me heck for something. I hate when I post here and only 1 person has something constructive to say and on DT, I get 25 responses in a day of all sorts of discussion!!
I am glad that you are finding that both lasers bleed around the same amount. I remember reps in the early days saying how much more bleeding one laser versus the other there was.
Glad I wasnt the only one questioning that from the photos I saw of very good cases done (smile lift cases) on DT.
Made me think…..hmmmm……my laser bleeds like the others.
Its great when the BS about one laser being faster , cutting better than the other give way to rationale discussions of how any Erbium laser can be used.
Its a huge positive step forward that this forum has maintained and why I really enjoy all the stuff that I have learned.
If I hadnt been part of this forum, so many things like small spoons from Mark, different topicals, how to open up an occlusal, different mechanisms of anesthetizing a tooth, etc all have helped me become a better laser dentist.
Great stuff.
Glenn
dkimmelSpectatorGlen , I did not say this before: Nice finish line. You cannot see the junction of the composite and the enamel.
David
Glenn van AsSpectatorThanks , if you are talking about the one on the gingival its because there is a big huge hunk of material under the tissue As for the incisal one……..I didnt do anthing to special except use a fairly low setting. I find that doing this reduces the ablated material and the depth of the ablation which for me helps hide the finish line.
Thanks
Glenn
Robert Gregg DDSSpectatorHey Glenn–
I’ll give you some grief later when I can post some pictures from the office.
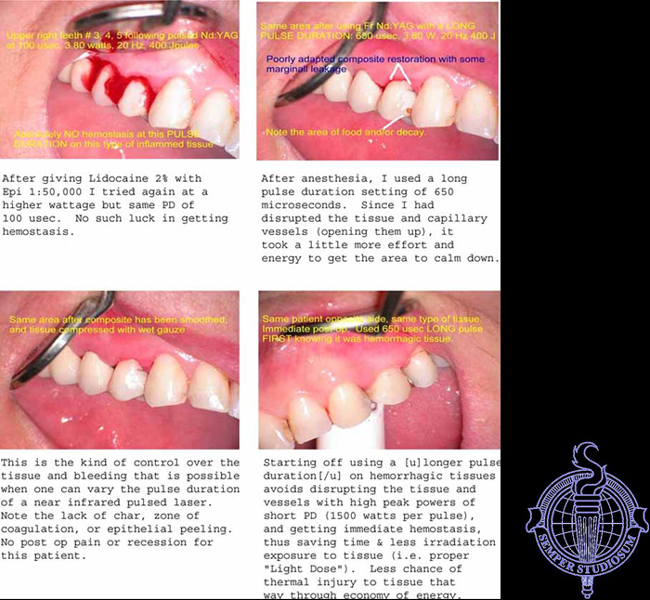
It isn’t just differences in laser wavelengths, but differences in a devices pulse duration that requires one to “shift device gears”.
If I use a short pulse duration such as 100 usec with arguably the best hemostasis laser wavelength around (the FRP Nd:YAG), I will STILL get hemorrhage like you got here.
By changing the pulse duration I can extend the zone of thermal penetration, absorbance, and “stasis” by the necessary amount to create a zone of irradiation and zone of thermal stasis that poaches the large diameter capillaries that caused the surprise.
For example (and in a manner of thinking only)
100 usec /= 100 microns zone of stasis
150 usec /= 150 microns zone of stasis
250 usec /= 250 microns zone of stasis
350 usec /= 350 microns zone of stasis
450 usec /= 450 microns zone of stasis
550 usec /= 550 microns zone of stasis
650 usec /= 650 microns zone of stasisSo a laser’s temporal emission mode (time) can then be thought of as correspondingly dimensional as well. assuming it has some tissue penetrating qualities such as near IR wavelengths do.
Pictures to follow……….
Bob
Robert Gregg DDSSpectatorOk, So I might have titled this sequence, “When two pulse durations are needed”.
Glenn van AsSpectatorHi Bob: Mark reported your post to me as an administrator, because he said your response was to intelligent for us mere mortals.
I think that your post is excellent and something that is not covered in most laser articles. How pulse duration affects hemostasis or the zone of coagulation. Once you explained it, of course it makes sens. Now I wonder how the longer pulse duration affects sensitivity. Is it worse with the 650 usec pulse than the shorter 100 usec.
Next off , I would have anticipated alot of bleeding in your case because the tissue looks inflamed so it doesnt surprise me that it bled alot.
Do you think that the tissue in my case looked inflamed beforehand. I didnt anticipate bleeding at all.
Thanks for your interesting post and email me privately because I do have to do some juggling to go to your meeting and then to a lecture in Bahamas.
Lee-Ann will not be coming to Huntington beach as she will be going straigth to Bahamas and I will join her after my lecture.
Just email me and I will iron out the details.
Take care and cya
Glenn
Lee AllenSpectatorBob,
I love this kind of explaination since it clears the air more that antecdotal reasonign that I parse together from experience and the forums.
I feel very limited in my ability to use the information since the waterlase has very limited adjustments. But the understanding of the effect of variations is still helpful. Puts treatment expectations in perspective.
Thanks.
Robert Gregg DDSSpectatorQUOTEQuote: from Glenn van As on 9:51 pm on Dec. 22, 2003
Hi Bob: Mark reported your post to me as an administrator, because he said your response was to intelligent for us mere mortals.I think that your post is excellent and something that is not covered in most laser articles. How pulse duration affects hemostasis or the zone of coagulation. Once you explained it, of course it makes sens. Now I wonder how the longer pulse duration affects sensitivity. Is it worse with the 650 usec pulse than the shorter 100 usec.
Next off , I would have anticipated alot of bleeding in your case because the tissue looks inflamed so it doesnt surprise me that it bled alot.
Do you think that the tissue in my case looked inflamed beforehand. I didnt anticipate bleeding at all.
Thanks for your interesting post and email me privately because I do have to do some juggling to go to your meeting and then to a lecture in Bahamas.
Lee-Ann will not be coming to Huntington beach as she will be going straigth to Bahamas and I will join her after my lecture.
Just email me and I will iron out the details.
Take care and cya
Glenn
Thanks Glenn,
Did you mean “Mark” or “Mike” from DT. Ouch!
Hey, I really appreciate your kind words here, privately, and on DT where I took a pounding for trying to help that guy, Mike, and others understand why we might use a laser in such a fashion as you did. Wow!
It was nice thinking on your part, in solving your immediate clinical challenge.
Not only did your patient’s tissue NOT look inflamed, it didn’t BOP either! So, no way I would expect your patient to have bleeding. Having said that, I might think about it now, as the etiology for that abfraction might be occlusal trauma to the buccal, which might suggest some “hidden” perio disease. We do see that in our LPT cases.
As to PD and sensitivity, I have not seen any differences in the effects on sensitivity. We typically use and recommend short PD. Why? What are your thoughts? More sensitivity might be possible?
Perhaps if one were to spend too much time at long pulse, might lead to more sensitivity? Haven’t seen it. The interesting thing about longer PD’s is that you actually end up using LESS total Joules (watts per second), because it is more efficient in getting to the treatment objective (hemostasis in this case), so often a lot less exposure to tissue than with a short PD (100 or 150 usec).
Sorry I won’t get to meet Lee-Ann for a while yet. I’ll let everyone know. We are looking forward to your presentation. Final programs announcements will go out at the end of the month. You are in distinguished company on the program. (That means I’m not on it!).
Merry Christmas and Happy Holidays!
Bob
Robert Gregg DDSSpectatorQUOTEQuote: from Lee Allen on 5:38 pm on Dec. 23, 2003
Bob,I love this kind of explaination since it clears the air more that antecdotal reasonign that I parse together from experience and the forums.
I feel very limited in my ability to use the information since the waterlase has very limited adjustments. But the understanding of the effect of variations is still helpful. Puts treatment expectations in perspective.
Thanks.
Lee–
Thanks for the kind remarks.
I’m glad I am making sense to a few people. I’ve known this stuff conceptually for a long time, but it has been a challenge to share the significance of varying the pulse duration of ANY free-running pulsed laser like the Waterlase, DELight, or the PerioLase with others, especially those that have been using lasers for a while (nobody here), that think they know all they need to know about laser parameters.
I predict other manufacturers will pick up on it. I know they will, since the market tends to follow those things that are being used succcesfully AND those things customers keep asking about!
Have a great holiday Lee! See you in PS for dinner at Hooters it sounds like………..
Bob
Lee AllenSpectatorBob,
Thanks for the PS invite. Hooters, huh? Never been there before. Only for night owls?
Lee
N8RVSpectatorGlenn —
I know this is a rather old post, but it brings up a question. Why would you restore this abfraction lesion in the first place?
Like everybody else, I see these all the time. Usually, they’re clean, hard and noncarious. And unless the patient complains of roughness or food impaction, they are totally asymptomatic and, in my mind, require no treatment.
That said, I’m open for education here. My eyes have been opened recently to a LOT of new treatments (compliments of my laser purchases!) but what’s the rationale for fixing these lesions when there’s no perio involvement and they’re asymptomatic?
(and you were complaining that nobody challenged your posts … HA!)
Thanks,
Don
Glenn van AsSpectatorHi Don……….what I had to do was look back at the case to see what I had put up……funny how my old mind is starting to lose it.
I dont like these notched abfractive lesions. These are often from occlusion and I have to adjust the occlusion.I am not sure it the periodontists would prefer to do the graft on these ones. I know the flat ones they like to do.
This was probably sensitive but to be honest with you I cant remember anymore but when I see a V type abfractive lesion which I suspect is from attrition, I am more apt to restore it like I did.
Here is one I did today that some periodontists I am sure would do a graft on but the patient was sensitive and wanted a resin in this case.
WHat say ye and oh ya ……..look at the spoon .
The enamel settings were 30 Hz and 70 mj but I used a 400 micron tip and that will give you a little bit of a deep bevel so look at all the loose enamel.
The color was a little off but it was ok and the patient loved the lack of anesthetic.
Soft tissue 20 hz and 30 mj without water and some air (gentle water spray from 3 way syringe)
Hard tissue 30 hz and 50 mj for dentin.
Enamel border 30hz and 70 mj.Flowable was point 4 opaque shade from Kerr.
Glenn

kellyjblodgettdmdSpectatorDon – I think that you have a great question here: Should we be restoring these lesions? Why or why not?
Check this link to read an interesting article which discusses the stress distribution at the cervical area of a tooth. It emphasizes that the deeper the cervical lesion gets, the faster it progresses. I found it helpful.
http://parkell.com/cervicallesion.html
Obviously, there is a slant here towards Parkell products, but I still appreciate the science.
Kelly
-
AuthorPosts
