Forums › Erbium Lasers › General Erbium Discussion › A place for laser Tx?
- This topic is empty.
-
AuthorPosts
-
AnonymousGuestHi All,
I thought I’d get some opinions on whether a laser should be involved in this case, and if so, how?. Those of you who have seen this case privately please refrain from posting until others who don’t routinely post have had a chance.
Background- 44YOWM presented w/ fractured tooth/post number 10. Pt refused implant, bridge, or CL w/ periodontist.

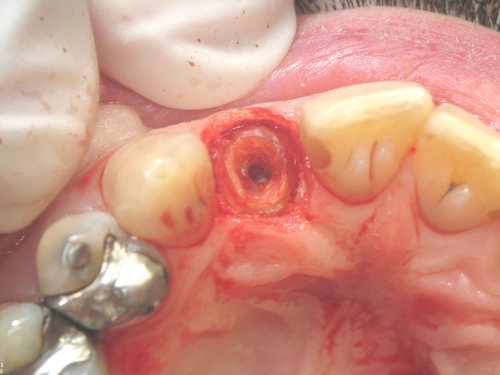
Old post crown removed-

Occlusal View-

Perio probe 1mm sulcus-

Xray after retreatment from endodontist (endodontist 1st Tx didn’t heal)

Lets start a discussion on how you would tackle this since the patient wants to keep the tooth.
Crown lengthening- closed or open?
Laser/no laser?
If laser, settings?
Type of post?
Cement/Bonding agents?
Type of crown?I look forward to your opinions and don’t worry about your comments as this case has been called a bunch of negative things from those who have seen it privately.
After some discussion, I’ll post details on Tx.
lookin4tSpectatorGeez, I dunno, do you use it during extraction and implant placement?
drkddsSpectatorHi Ron.
I’ve yet to come up with a way to use my laser to make a flipper, but I’m tryin!
I’m going to assume the endo has been re-tx’ed.
I don’t do crown lengthening in my office, but he’d better have a low lip line!
I would prepare a post space a minimally as possible while achieving significant canal wall engagement. I prefer stainless steel posts and Panavia for their cementation.
I build up with Tenure + CorePaste.
I’d probably go with a cerec In-Lab crown for this case. I LOVE their margins, I think they look nice and don’t require a ton of reduction – and you can use a chamfer.
I’d also invest a tremendous amount of time discussing the guarded prognosis of this tooth. You can’t polish a turd, ya know. This tooth is a turd!
dkimmelSpectatorOH !
David

whitertthSpectatorQuite honestly, with the isze of the area and the potential crown to root ratio following crown lengthening and the total costs involved I would always exo this and do an in implant…I just dont see reason today with the predictability of implants to mess arond with a tooth like this..maybe I am a tad aggressive but long term I think thats a better option…
N8RVSpectatorOK, Ron, I’ll play …
First, it sounds exactly like the majority of MY patients! “Can’t you just glue it back in?” (followed by all the usual reasons why they can’t afford anything else right now, of course.
Given that extraction/implant tx is out of the question, along with seeing a periodontist for CL, I’d probably have a LONG discussion with the patient about how guarded the prognosis is for this tooth no matter HOW it’s treated. Assuming he says, “No, I want YOU to save my tooth,” I’d propose the following and will expect to get flamed for it …
1) Closed CL. I know, I know … really bad idea. However, from the info given, the patient doesn’t want to either endure or pay for a flapped, surgical procedure. Fine, the prognosis is guarded anyhow, so whip out the laser and do your best to remove some bone, clean up the tissue and get some tooth on which to hang a margin.
2) Make a conservative post space for a cast post & core-crown combo
3) Take impression
4) Temporize
[Really Big Disclaimer: I’ve never done closed CL with the laser. Heck, I’ve never done CL of any kind, so this idea is probably so much blather, so take it for what it is.]
However, I DO know patients of this mindset, and they just aren’t into fancy, comprehensive treatment plans. The will, however, love you and pay you a reasonable fee to figure out how to save this tooth, if only for a short time.
Seems like a good opportunity to do a closed CL, save the patient some time and money … but NEVER take pictures of the procedure and post them on anywhere online! 🙂
— Don
AnonymousGuestQUOTEQuote: from N8RV on 3:28 pm on Aug. 24, 2004
OK, Ron, I’ll play …Seems like a good opportunity to do a closed CL, save the patient some time and money … but NEVER take pictures of the procedure and post them on anywhere online! 🙂
— Don
Don, glad you’re playing along!
Well almost never post pictures… :shocked: I’ll take a chance this time because I’m off to San Antonio for the Southern Laser Conference for a few days. You guys can pick it apart while I’m gone. To be honest, the whole purpose of this post was to see if we could get some new people comfortable with posting and I see myneighbor Doug in Grandville joined us as well as another Midwesterner-Don
First off, let me say that I’m definitely not advocating this treatment as something that should be done routinely. The prognosis is guarded long term but given the limitations I had, the outcome appears reasonable so far. IMO, Access and visibility were very important as well as the ability to currette and reshape the bone.
Begin Troughing/lengthening 1.0W 50/50 up and down motion not touching bone- er,cr:YSGG


CL and cast post prep complete. bone was smoothed w/ curette (tooth prepped with highspeed)-
Temp in place, intentionally short(opposing cuspid and lateral hit almost end to end w/ old crown.

Palatal view 8 weeks

Buccal view 8 weeks (little bleeding from food impaction on mesial)

Temporary Removed /Cast post-core cemented. I was able to get about 2.5 – 3 mm ferrule

Crown Seat 2-3 weeks later

Palatal View at seat

Seat x-ray- (apology to the periodontists- my assistant should have lined this up a little better so you could see the bone better)

Andrew SatlinSpectatorHi Ron,
We all agree on what this patient really needs and we have all had to accomadate patients who want to dictate treatment.
For the discussion I thought I would add the option of ortho extrusion.
If the root length is good and the taper is not extreme extrusion is a great way to get crown length in the esthetic areas. Minimal resection is necessary and preservation of the papillae is easier.
I have never done closed C/L but this looks like cases that have been posted and restored using this method.
The prognosis is poor regardless so I would say least amount of time and money needed is best in this case.
See ya,
Andy
drkddsSpectatorHi Ron.
CL isn’t a procedure I’m ready to do in my office. With my laser or with a blade! So I have a hard time even coming up with questions for you. I haven’t done a crown lengthening since I mauled a hog’s jaw in 1997 in my AEGD. I figure Dan Melkers will be by any time to let me know the things I don’t even know I don’t know. (that’s a good thing…:)
I do have a question for you, though – I’ll phrase it in the form of a laser forum question.
Why did you (laser) decide to (laser) use a cast post and (laser) core (laser) versus a prefabricated (laser) post and (laser) core?

Thanks for the welcome, btw, neighbor!
AnonymousGuestQUOTEQuote: from drkdds on 10:35 pm on Aug. 25, 2004I do have a question for you, though – I’ll phrase it in the form of a laser forum question.
Why did you (laser) decide to (laser) use a cast post and (laser) core (laser) versus a prefabricated (laser) post and (laser) core?

Doug,
In my hands I’ve always had more patients with preformed posts with core buildups fracture or fail than I have had fracture cast posts and cores (or the root). This patient presented with a preformed post and core buildup that had failed so I decided to go a different route.Thanks for the question.
I’m probably asking for it here, but, I find it interesting that my periodontist friends can agree on the risk involved in doing this case and the potential for failure but there have been no comments from them on the tissue response. Well perio guys, leaving the risk factors out and the method in which this was done, is the tissue response what you’d like to see? If it’s not, I’d like to learn what else I should expect out of something like this.
Again, I’m not advocating this as a routine procedure for anybody.
kellyjblodgettdmdSpectatorOh my goodness, Doug! I’ve just stopped laughing about your “polishing a turd” analogy. By the way, I’m stealing that one. Hilarious!
Ron – It’s very hard to argue with the tissue response. Perhaps the body know’s more about how to heal than we sometimes give it credit.
Kelly
mickey franklSpectatorHi Ron
I would do the same as you did.
It would be interesting to know what you charged for all these procedures compared to what you would charge for an extraction and an implant.
Thanks for posting this case.
Mickey
drkddsSpectatorFinal result looks really nice, Ron. Tissue response looks better than I would have thought. Good job!
Samuel MossSpectatorRon,
I’ve done a few of these, however with prefab stainless steel and fiber posts. Your patient’s tissue response, by the way, looks “marvelous.” It seems that upper bicuspids and upper laterals seem not to last very long in that 1) the poor crown to root ratios–especially those roots that were already short in the 1st place and 2) the dark forces of occlusion that broke the camel’s back originally seem to find their way back–even when “taken out of occlusion.” So, trying to ensure , especially in the anterior region, the ever important ferrule and thus making a borderline C/R ratio tooth, I end up seeing more than a few coming back with fractured roots. Even though we’ve had a documented discussion about the poor prognosis and consent signed, there is definitely dissappointment on both sides as now that investment is down the toilet and something more expensive must be in the works.
Now I go into the risks, prognosis, etc, and do not many of these any more. I even suggest that they get a 2nd opinion or an opinion they want. I’d rather they get disappointed with someone else down the line than me and I sleep a little better.
Great photography, by the way.
Mossman
AnonymousGuestQUOTEQuote: from mickey frankl on 2:31 am on Aug. 27, 2004
Hi RonIt would be interesting to know what you charged for all these procedures compared to what you would charge for an extraction and an implant.
Mickey
In discussing this with the patient I said that I would not charge for the CL. Patient paid endondontist and for post/core/crown(Insurance covered 80%). I also assured the patient that should this fail in under 5 years that I would credit what he paid toward any restoration that would need to be placed on an implant.
I have a periodontist or OS place implants so I can’t comment on the cost comparison except to say an implant and crown usually works out pretty close to a 3 unit bridge. -
AuthorPosts
