Forums › Erbium Lasers › General Erbium Discussion › A case of localized bone relief
- This topic is empty.
-
AuthorPosts
-
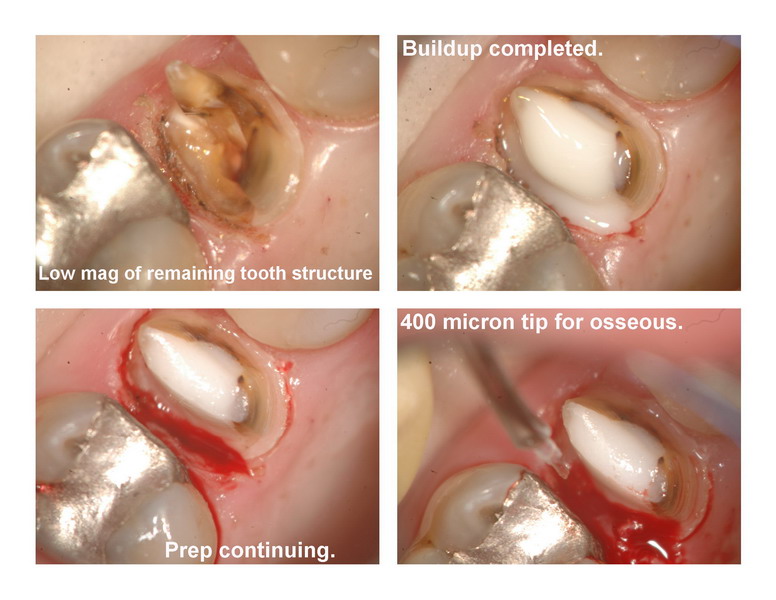
Glenn van AsSpectatorHi there folks: I got into a difficult case here which shows the power of the scope for handling these tough cases and the laser for helping me see what I was doing.
This lady had a crown done by another dentist and told me it never felt right. In addition she always got food caught in the interproximal space.
I opened up the tooth and did the endo and then advised her to redo the crown as well. Lucky for me it was still retreatable. I didnt realize the decay was as big as it was until I looked at the radiograph on my monitor (I took a JPEG of it) and realized how much more I could see at higher sized images (one power of digital radiography).
Anyways, I cut of the crown, cleaned up the margins to see how deep the decay went and then used the diode at 1.0w, CW to tryand do two things.
1. Create visibility of the distal margin because there was alot of blood.
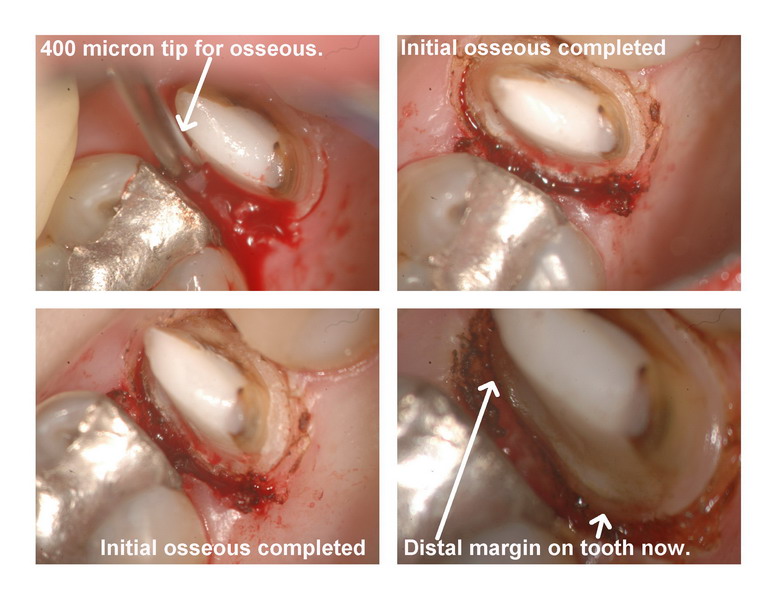
2. Open up the sulcus for the hard tissue laser.I was going to do open flap but looking at the radiograph the mesial root of the molar was in very close proximity to the premolar. By the time I used the diode laser interproximally, I had complete visibility of the site and decided to try it closed flap.
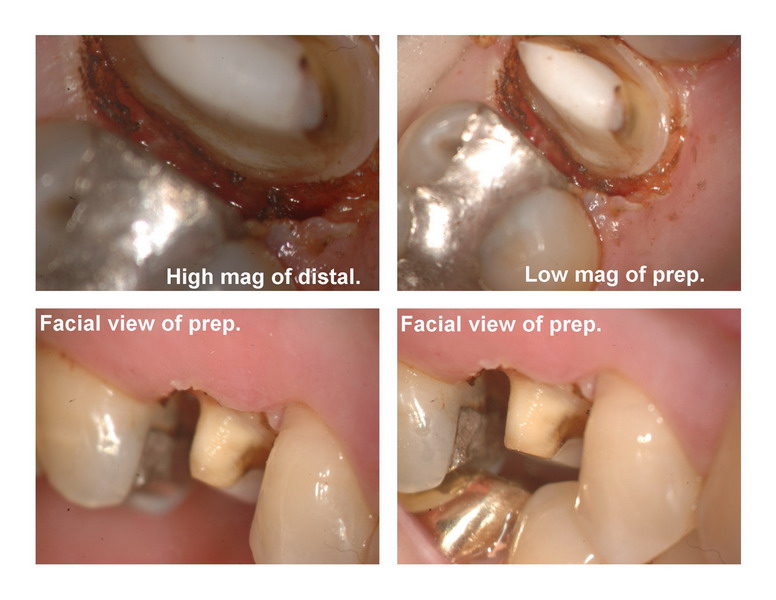
I used a 400 micron tip first and then lowered the settings and used the chisel on its side to go 3 mm down. I tried to angle the tip, and in addition “feel” with a probe and explorer in this case.
I put a post and core in the tooth, and took an impression and put the provisional on. Took a final PA and it will granulate in.
I have seen alot of Dannys great cases with treatment of complex multiple teeth anteriorally but am wondering how the periodontist handle these kinds of cases where it is a localized area, with minimanl distance between roots. Have you any suggestions.
Hope the photographs are ok, off to the inlaws for dinner so no time to lighten up the higher mag ones and my xenon bulb is on its last legs.
Glenn








kellyjblodgettdmdSpectatorGlenn – That’s beautiful! I swear, that’s exactly what I would have done {except the crown would be done already using the CEREC
 } You know, with patients like these, it’s no wonder we’re so busy. Look at all those old restorations!
} You know, with patients like these, it’s no wonder we’re so busy. Look at all those old restorations!My suspicion is that this will heal beautifully. My biggest concern for this patient would be that her caries risk level be thoroughly assessed. From the looks of her gingiva, I would assume that her home care is pretty good. So why the continual caries? Does she have a high level of exposure to fermentable carbs? Where are her levels of Lactobacilli and Strep Mutans? From the looks of the X-rays, she has similar recurrent caries on the distal of #30. Anyway, just some questions I had.
It’s funny looking at these scope pics, Glenn. It’s deja vu, or maybe we’re just on the same wavelength (pun intended!) Fantastic case and documentation. And a great minimally invasive service to your patient.
Kelly
dkimmelSpectatorGlenn,
Man I have been looking at this thread and thinking. I have held off posting but I think you know me well enough now to understand where I am coming from!X-rays be misleading at times.
I have some concerns about the location of the margin and the osseous level on the X-ray. It seems darn close.
jetsfanSpectatorGlen,
As you lowered bone on the distal, did you extend to direct buccal and direct lingual to prevent negative architecture.
Robert.
Glenn on the roadSpectatorOk guys and gals….I am swamped at work and with articles so I havent been able to answer much.
Here goes quickly my replies
Kelly this patient has some issues with some of the previous dentistry that has been done. I am a firm believer by now that no magnification at all (like this docs) can make it very difficult to handle cases like this one. Heck I had a hard time with it. I was surprised that there wasnt more decay under the crown. I dont know what the strep count was but her decay rate isnt huge, just alot of average dentistry done in her mouth. It works well until its a tough case, thats when they have failures.
David: the radiographs are misleading as they dont show the buccal and lingual aspects of the bone. I didnt reduce under the Buc and Lingual papillas so that is why the radiograph looks the same.
The key is to look carefully at the impression of this area….look at the roll on the impression. This tells you how much depth there is below the margin….LOTS.
Robert…..I didnt extend to the buccal and lingual a ton. Lets see where it heals but I can tell you that I now have done this quite a few times with perfect healing and my first case has follow up to around 15 months with no compromise in healing.
Take care
Glenn
lookin4tSpectator“I didnt reduce under the Buc and Lingual papillas so that is why the radiograph looks the same.”
So you created a trench?
Glenn on the roadSpectatorWelcome back hack2, looking4t, etc….did you get a laser or are you just visiting?
Not necessarily a trench. It could be that I flattened the bone interproximally down 2-3 mm but didnt ramp up the palatal or buccal. Just removed 2-3mm in one selective area.
I realize you are not a fan of lasers, and that is fine. I recognize that you are also not an advocate of closed flap crown lengthening, and that is fine. I also recognize that you dont agree with some of the things I do and that is fine.
I also realize that you have alot to offer on perio, biology , healing etc. and that is great
Finally, I realize that you dont have a laser and this is the laser dentistry forum for those that have or are interested in lasers …..that is fine too.
I dont want to get into arguments about things. I have resisted getting into discussions with you about this since our last heated debate on DT. I have also mentioned that I will not get into old debates.
We agree to disagree but it seems that you have decided to revisit and open old wounds. I am not sure as to what your reason for coming here to discuss this again was. In fact the thread seemed to have died down. I am awaiting the postop photos and like always will show the good with the bad.
The tissue like me has healed . The tooth is still present, and I have no intention of debating in private or public any longer your disagreements with my techniques for localized closed flap crown lengthening. I have made large strides towards trying to improve both my surgery and flap work. It is fine to disagree with my techniques and to criticize them and you are entitled to do so, just dont expect me to get into anymore public or private debates about it. I am done discussing things on this topic or lasers with you.
All the best and happy new year to you.
Glenn
lookin4tSpectatorYou have created a crater by what you described, it’s a periodontal defect by definition. You clearly don’t understand what that means or the implications of it long term. Healed gingival tissue and the lack of tooth loss are generally not the best criteria for success either. In addition, with good hygiene, some of this unfavorable architecture can be maintained for what is usually a relatively short period of time. In all honesty, I don’t think you really removed that much bone at all, or at least MUCH less than you think you did and it will likely end up OK. Creating a 2.5-3.0mm crater however is not something a person with a periodontal background could comfortably advocate unless creation of localized mild to moderate periodontal disease was the goal.
If this is closed flap crown lengthening, and in this case, more appropriately called gingival interproximal denudement, you are correct that I disagree with it. The fact that you can’t see why is bewildering.
As far as a heated debate-the only heat came from you, kind of like now. I’ve got other observations regarding that I need not share.
Apparently you will never quite get what negative architecture and crater defects become long term, and don’t care to. There is no right way to create a crater, so modify as you like, it still will be a problem.
In deference to the tone of this board I will also have no further exchange of any kind with you here since it upsets you so much and I have a ton of respect for Ron and what he is trying to do, but I’ve made a little home at DT so if you don’t want to see any comments from me if the mood strikes I guess you don’t have to post there.
As long as you choose to air differences publically as opposed to professionally and in private, you won’t need bother yourself with saying hello in Vegas in February either. I think you are someone trying very hard to do a wrong thing in a right way and it contrary to your statements, the reason it is wrong has nothing to do with the use of a laser.
wilson11Spectatorlookin4t, all hostility between you and Glenn aside, what would you have done in this situation?
AnonymousGuestthis is the song that never ends….

I’ve received a couple PM’s asking if I’d comment on this case (not sure why as there are alot of more talented dentists here than I) but here goes-
1. I don’t think it is a goal of anyone here to create a 2.5-3 mm crater. I think the goal is to develop a way to do this in a less invasive way than flap surgery. Now I know the specialist wll say that is not invasive, but I’d have to guess with the number of times a GP does it, it probably does qualify as invasive. What I find interesting, about what Glenn did, is that ulike what you usually see in these cases- a trough right next to the tooth being prepped- it appears he has tapered the bone away from the tooth in question toward the molar. The xray does make it appear that the bone is relatively close to the margin of the temp on the bicuspid. This brings up a question in my mind- with good hygiene, will the bone remodel to move away from this margin and thereby change the overall architecture to a more positive one in this area?
2. when I look at the preop picture of the tissue on the mesial of the bi, I find it a little surprising that when you consider the margins, the tissue looks the way it does on the mesial. Looking at the xrays I’d have thought the distal tissue would have been more likely to look the way the tissue does on the mesial.
3.everytime time I see this debate I think about how many dentists not using magnification don’t even realize what needs to be done in areas like this, or how many don’t have a clue when it comes to BW. While I’m sure Glenn would agree that ideally a flap gives a much better abiity to see and recontour, i also think this will be ok in the end and will be much better than what the guys get who ignore this or blow away everything in the sulcus with a handpiece.
4. While not the way life should be, many times in my practice I have to deal with the patients overall ability to pay for tx. When you are already talking endo/core / crown and then ask the pt to pay another 跌-600 for the periodontist to crown lengthen, it just puts the cost out of reach of alot of my patients. I then have to decide if I can justify making some improvement using my laser at a minimal fee and thus allow a patient to keep a tooth (although not in an ideal situation) they would have extracted.
I think the contribution of the periodontist here has been good in getting us general dentists to think about BW. I also think that when the periodontist sees a patient of mine, he is really seeing a subset of my general patient population. At least in my area, those that go see the periodontist have a whole different mind set than what my general patient population has. This may color my periodontist perception of what I have to deal with daily as far as patient motivation.
Finally, I hope that February will bring a chance to meet face to face and overcome the limits this forum brings when it comes to understanding the intent of some posts.
I do have to say that in my office gingival healing and lack of tooth loss are pretty good indicators of success
 but I think i understand that there is also more to it than that.
but I think i understand that there is also more to it than that.Gotta go, have a day full of my daughters volleyball tournaments, so have a great civil debate.
I sure hope the ref understands my intent when he hears me yell from the stands 😉
Glenn on the roadSpectatorFirst off Ron thanks for your thoughtful and thorough response. As always you have created a civil and professional post and it keeps in line with the overall scope of the LDF.
I want to lead off by saying that I really appreciate all the efforts of Danny and to a lesser degree Hack in trying to teach us periodontal principles in application to laser technology. I have learned alot from their posts and particularly Dannys great photographed anterior crown lengthening cases and posterior cases of root reshaping.
Second off, I have seen many many anterior cases posted on Dental town which are beautiful from Danny. I have yet to see a single periodontist post a case of interproximal bone relief in posterior teeth. Why is this?
I suspect that not many dentists do refer in these cases although it happens often with posterior crown preps when the interproximal amalgams approach bone. So what are the general dentists doing – are they referring patients. I can tell you the one patient I referred to the periodontist for interproximal bone recontouring ended up with significant sensitivity to cold and also a large posterior triangle without any papilla so that things could be gradualized out. In addition I have 3 patients in my practice who have gone through osseous recontouring in one quadrant and have repeatedly told me that they will not go back for the other 3 quadrants of “non invasive ” periodontal surgery. It is the reality that most patients dont want surgery.Heck I have a huge kidney stone in my right kidney, (perhaps accounting partially for my testiness these days) and I dont want to have surgery on it…..do anything you can to break it up without having surgery. Just the word creates some angst for me. Do Danny and Hack do wonderful surgery ……YES, but patients dont love having to have it done.
WHy is it that the initial dentist just drilled down with a bur, didnt worry about
1. Biologic Width
2. Getting a solid margin on tooth structure.
3. Removing all the decay.I have a feeling that this is the norm. I see it on my endo forum that I belong too, the specialists (endo) were discussing how to restore a tooth which had deep decay subgingival and the consensus was to take a bur and remove bone and tissue.- all done closed flap.
I have yet to see ANY posterior cases posted showing interproximal treatment done, especially with the magnificiation and detail that I am trying to show.
Danny has shown exquisite long term results from his root shaping cases which are unique in their application and best suited for buccal and palatal treatment. I thank him for opening my eyes to another possibility in posterior cases.
I think that sometimes that these difficult cases are a compromise no matter what you do. You can flap and graudualize bone creating iatrogenic root recession and sensitivity on adjacent teeth with a large dark interproximal space. You can in addition extract as many periodontists in my area are doing for ANY questionable teeth and put in the all mighty titanium. I do restore implant abutments in my practice but my first goal is always to try and retain what is there.
Next off it is difficult to determine in this case how much bone was removed because of the angle and the difficulty in showing this and the PA does you no justice because the buccal and lingual papillary bone areas are still at the same heights. The only clue is if you look at the impressions and as stated before you get some idea of the roll of impression material into this area.
In reflecting a flap in this area and removing bone it would be a difficult case because of the root proximity of the mesial root of the molar to the distal of the premolar. Perhaps the best insight I had from someone on DT, was to have considered extrusion which I dont do often simply because of the time necessary to complete the extrusion but it is a viable alternative in this case.
I to be honest had forgotten this case but was surprised that it was brought back up again by Hack2, looking4t etc and I was wondering why after a month he suddenly posts on this again with a short terse reply obviously intended to do nothing but stir the hornets nest, and he is surprised that I stand up for myself, but that is ok.
I post cases here for everyone to learn and do so realizing that not everyone will agree with my treatment, in fact I often learn from the constructive criticism that is levelled at it. Danny has taught me alot.
I also realize that some people have such a built in negativity towards a technology or a treatment that they belittle anything done with it.
I for one am not a big Cerec fan, although I do think that the Cerec 3d is a big improvement over previous versions. I have seen some exquisite crowns done with this technology, but when I looked into it under the scope , the marginal fit of the crowns prepared by the salesman didnt come close to the fit of the crowns made by my lab.(Cerec 3)
Do I go onto the Cerec forum and dish the technology, nah……..not my way.
If someone wants to continually be negative about a technology that is fine but if you do so in a forum where almost all the people own or are interested in laser technology then I figure I have the right to defend myself.
In closing, I never think that my way is the only way to do things. I have repeatedly tried to show an alternative to traditional means of doing certain things in dentistry. Its simply something that is easy for me to show because of the scope and my past experiences from using the technology for the last 5+ years.
That experience has shown me that some things work and some dont and I am always open to new ideas and to showing my successes and failures. No one can accuse me of not trying to educate or teach and in the process I have learned alot about myself, my own dentistry and my ability to withstand criticism.
I hope this clears up some issues and I prefer to move onto other areas of constructive discussion regarding the relative benefits of using lasers in private practice.
Glenn
lookin4tSpectatorReply to Ron:
“The xray does make it appear that the bone is relatively close to the margin of the temp on the bicuspid. This brings up a question in my mind- with good hygiene, will the bone remodel to move away from this margin and thereby change the overall architecture to a more positive one in this area?”
If the bone is close to the margin, it has been documented that you will get slow resorption over time with irritation. That pattern of bone loss will usually be irregular. It also tends to lend itself to periodontal defects. I see them all the time. However, some may stay stable at a deeper than normal probe depth for a VERY long time. Others serve as a niduse for additional periodontal breakdown. In population studies, about 10% of the people NEVER get periodontal disease, around 10% get severe, and the rest are in between. In 10% of the people you will always be OK, in 10% you will never be OK, and the rest will be in between when this is done. Does that make sense?
In this case, with the denudement of the gingival tissue, you will get some resorption of bone as a result of that that will make the difference in bony height less of a step. However, on the mesial-palatal of the molar, you will have a step, that may lend itself to mild periodontal involvement.
Overall, I’m not sure biologic width was established, as described it will lend itself to mild periodontal involvement that may or not be stable over time.
See you in Vegas Ron.
lookin4tSpectatorGeez, Glenn, don’t mention me and I’ll abide by what you ask:
“First off Ron thanks for your thoughtful and thorough response. As always you have created a civil and professional post and it keeps in line with the overall scope of the LDF. “
I think you need to take a good hard look at the rest of what you wrote here and see if it’s consistent with the first paragraph. It doesn’t bother me at all, but it’s two faces of one argument with what follows IMO.
“I want to lead off by saying that I really appreciate all the efforts of Danny and to a lesser degree Hack in trying to teach us periodontal principles in application to laser technology. I have learned alot from their posts and particularly Dannys great photographed anterior crown lengthening cases and posterior cases of root reshaping. “
I spent a considerable amount of time showing you how to make a vertical, not splitting papillas, bringing the data you asked for. Perhaps your anger has clouded what used to be a good relationship..at least as I perceived it. I had recommended people to see you speak….and would likely still do so as you and Mark Colonna are the only two speakers I’ve seen on erbiums in restorative dentistry that have good info to share even if I don’t agree with all of it (yeah, I’ve heard you speak Glenn). Sorry it’s come to this Glenn.
“Second off, I have seen many many anterior cases posted on Dental town which are beautiful from Danny. I have yet to see a single periodontist post a case of interproximal bone relief in posterior teeth. Why is this?
I suspect that not many dentists do refer in these cases although it happens often with posterior crown preps when the interproximal amalgams approach bone. So what are the general dentists doing – are they referring patients. I can tell you the one patient I referred to the periodontist for interproximal bone recontouring ended up with significant sensitivity to cold and also a large posterior triangle without any papilla so that things could be gradualized out. In addition I have 3 patients in my practice who have gone through osseous recontouring in one quadrant and have repeatedly told me that they will not go back for the other 3 quadrants of “non invasive ” periodontal surgery. It is the reality that most patients dont want surgery.”Ummm…maybe we don’t take pictures of that because it is routine and not exciting in any way, shape or form. We also don’t have as many to shoot as violation of biologic width is rampant and not often referred. If you like I could dig those photos up, but then you would have to have a dialogue with me, and that seems to incense you (even a small simple, sentence). It would also require a bit of my time, and apparently, I haven’t been that useful to you or anyone else and my time is valuable to me. The reason is not patient comfort as much as you would like to believe. Perhaps your bias is leading you to an incorrect conclusion. I would agree that most people don’t want surgery…I’d also tell you I’ve worked on several that had no trouble coming back for more later after they realized how easy it was. Of course, throwing in osseous surgery is not apples to apples is it? A straight forward single tooth crown lengthening on that tooth equals no need for vicodin, and probably no advil in that part of the mouth. I also have no idea how your guys are doing osseous. If they are in the grand school of ultimate positive architecture….it ain’t easy on the patients. There are other modes of treatment to consider as opposed to one size fits all therapy. Could you maybe stick to crown lengthening as that was the discussion topic?
“Heck I have a huge kidney stone in my right kidney, (perhaps accounting partially for my testiness these days) and I dont want to have surgery on it…..do anything you can to break it up without having surgery. Just the word creates some angst for me. Do Danny and Hack do wonderful surgery ……YES, but patients dont love having to have it done. “
In a comparison of post-op photos, crown lengthening in my hands seems to heal faster than in yours. Have you seen any of mine or Danny’s patients that you can make that statement from? Are you sure your patients “love” interproximal denudement as done here. Bob Gregg suggested my patients may like me and don’t always give me the straight scoop, I imagine that applies regardless of the tool. As always individual mileage on a procedure varies from one to the next. I just happened to go to a New Year’s party that featured two of my crown lengthening patients that went on and on without solicitation of how it didn’t hurt at all. I’m sure I can find some that say the opposite however. In any event, the pissing contest here is pointless..two opinions, both will be right at one point or another. I place a bit higher value elsewhere.
“WHy is it that the initial dentist just drilled down with a bur, didnt worry about
1. Biologic Width
2. Getting a solid margin on tooth structure.
3. Removing all the decay.I have a feeling that this is the norm. I see it on my endo forum that I belong too, the specialists (endo) were discussing how to restore a tooth which had deep decay subgingival and the consensus was to take a bur and remove bone and tissue.- all done closed flap. “
That was one in the mid-80s..you’re doing it with a laser now, but it looks much nicer to the tissue with the laser than the bur. Perhaps Canada doesn’t reflect my area. There is also a difference with new tech on hemostasis, ability to get impression, etc.
“I have yet to see ANY posterior cases posted showing interproximal treatment done, especially with the magnificiation and detail that I am trying to show.”
I’m not sure what you’re trying to prove here besides your value as a result of your effort. Was that the point?
“I think that sometimes that these difficult cases are a compromise no matter what you do. You can flap and graudualize bone creating iatrogenic root recession and sensitivity on adjacent teeth with a large dark interproximal space. You can in addition extract as many periodontists in my area are doing for ANY questionable teeth and put in the all mighty titanium. I do restore implant abutments in my practice but my first goal is always to try and retain what is there.”
This is not a difficult case though is it? I would agree minimize the compromise can be a good catch phrase. If it’s the mesial of a first premolar and it’s deep, the titanium isn’t always a bad idea. Why criticize one technology while using another? Are they both not viable? Saving teeth with a compromise versus extracting is always an interesting debate-taken on a case by case basis. I can’t see this one as an extraction, nor did I call for it.
“Next off it is difficult to determine in this case how much bone was removed because of the angle and the difficulty in showing this and the PA does you no justice because the buccal and lingual papillary bone areas are still at the same heights. The only clue is if you look at the impressions and as stated before you get some idea of the roll of impression material into this area.”
PAs aren’t appropriate to look at here, the BWs are..as I pointed out at DT. You are 100% correct.
“In reflecting a flap in this area and removing bone it would be a difficult case because of the root proximity of the mesial root of the molar to the distal of the premolar. Perhaps the best insight I had from someone on DT, was to have considered extrusion which I dont do often simply because of the time necessary to complete the extrusion but it is a viable alternative in this case. “
Looking at the BW, the roots aren’t that close are they? In a tight space, you can use a beavertail ultrasonic to remove bone, a sugarman file, etc. You can also smooth up the root when you get done if you abuse anything if you have a flap. In this case, a flap is more likely to have more bone coverage with tissue at the finish if that matters….and given what some people do with straight line incisions..it doesn’t matter that much I guess.
“I to be honest had forgotten this case but was surprised that it was brought back up again by Hack2, looking4t etc and I was wondering why after a month he suddenly posts on this again with a short terse reply obviously intended to do nothing but stir the hornets nest, and he is surprised that I stand up for myself, but that is ok.”
There was nothing terse, just short. I’ve also made no secret here of my ID at DT..and many here know me by name or even personally. I waited a month to respond to anything you posted in deference to what appeared to be unjustified anger that lead you into a post that you did that was clearly ONLY meant as a personal attack. Perhaps you’re forgetting your conduct and in context, I can’t see where your anger is justified. I think a short reply to stimulate discussion can be more effective than a long one. Hardly anyone outside of you or Ron will read this whole thing. That post was meant to stimulate thought as to what you’re doing with the architecture and what that can mean. I will readily concede in some cases, a small compromise is acceptable-I do it myself. I wouldn’t view a 3mm crater as a small one though. In this case, it is unlikely to be where you think it is IMO.
“I post cases here for everyone to learn and do so realizing that not everyone will agree with my treatment, in fact I often learn from the constructive criticism that is levelled at it. Danny has taught me alot.”
And you went after him pretty good for quite awhile and said he wasn’t being constructive, just abusive. I think there’s a lesson in there somewhere. By exclusion, you are suggesting I post to cause trouble, not to learn. That is complete BS and inconsistent with my actions.
“I also realize that some people have such a built in negativity towards a technology or a treatment that they belittle anything done with it.”
That is inaccurate, unfair, and in a vein that can’t be supported by my actions. Belittling something would mean attacking it for the purpose of attacking it…to wit, with no basis in fact. I have yet to see where your concern is when you look at trench formation, crater formation,and negative architecture. I see criticism of conventional crown lengthening, but when done conventionally with a laser it seems to take on a new meaning to you. Perhaps you are as biased against older methodologies as you think I am against new ones. I guess I should throw out my implants, PRP, fibrin glue, digital X-rays, stacks of journals, T1 line to connect the offices, paperless office, etc. just to prove you correct.
“Do I go onto the Cerec forum and dish the technology, nah……..not my way.”
I have not dished the technology in this thread-the application of it requires deeper thinking IMO. It was said without heat or any hint of a personal attack…that came in your reply. Apparently a more lengthy reply would have assuaged your hurt feelings, but I honestly didn’t see it as rude. Given that perception is reality, the only thing I can offer is my apology that it was not meant taht way. I wanted to know what you thought you did. I am of the opinion you removed much less bone than you thought, a vertical BW would be useful post-operatively, and that in some cases, as I have said now TWICE, minimizing the compromise is something that is perfectly fine. In addition, I could link to the old thread on closed versus open and see if the numbers are the same now. It apparently isnt’ just me. Are you going to respond to them the same way? Are they “dishing” new technology when they say it?
“If someone wants to continually be negative about a technology that is fine but if you do so in a forum where almost all the people own or are interested in laser technology then I figure I have the right to defend myself.”
If someone tells me they won’t be responding to me, then respond in a self-styled personal attack after commenting how nice things have been set-up here, I will likely choose to respond. As pointed out, it was not the technology, but the application of it. Erbiums are fine and may be better for some things. People are interested in lasers here..all the more reason to consider from a different view what is being done. If everyone is thinking the same, then someone isn’t thinking. In this case, IMO, you removed much less bone than you estimated, are little close on biologic widht, but will likely end up OK due to the fact that there hasn’t been as much compromise as you estimated (third time).
Now, I sent a private message to you last night…if you want to continue this, you can continue it in private, or by yourself, I’ve said all I will say and refused to get sucked in by you calling me out again. If you genuinely want a respone, you let me know…otherwise I will show you, Ron, and the message board as set up my respect by not posting to you. You have more to contribute on erbiums than I have to contribute on general biology. When I have a professional difference of opinion on something that doesn’t make the other guy a bad person or even a bad dentist for that matter. Bad ethics make a bad dentist-every time IMO. The rest is person by person…just like they view me. Apparently, it isn’t quite the same for you-it’s more personal. It is not a weakness, just a difference in how we think that I will try to be cognizant of if we have any future interactions. I will endeavor per your request to avoid them.
(Edited by lookin4t at 3:22 pm on Jan. 8, 2005)
ASISpectatorHi All,
It’s been a while since I have visited the forum. It’s good to see the new members that have joined. It’s good to see that Glenn continues to be so prolific in his documentation and sharing of cases.
As in the past, sometimes when a difference in opinion exits, it tends to undermine the whole purpose of the forum which is sharing the case and learning from one another.
I feel the case was handled very well and Glenn certainly provided his reasoning in doing it closed flap. To really be certain of course and satisfy all queries, flapping after the osseous relief would be the way to go. But that would delay the impression for a number of weeks which may or may not be the choice decided by Glenn and his patient.
Glenn, thank you for sharing.
Ron, thank you for your eloquent words.
Andrew
-
AuthorPosts
