Forums › Erbium Lasers › General Erbium Discussion › How would you do this osseous case
- This topic is empty.
-
AuthorPosts
-
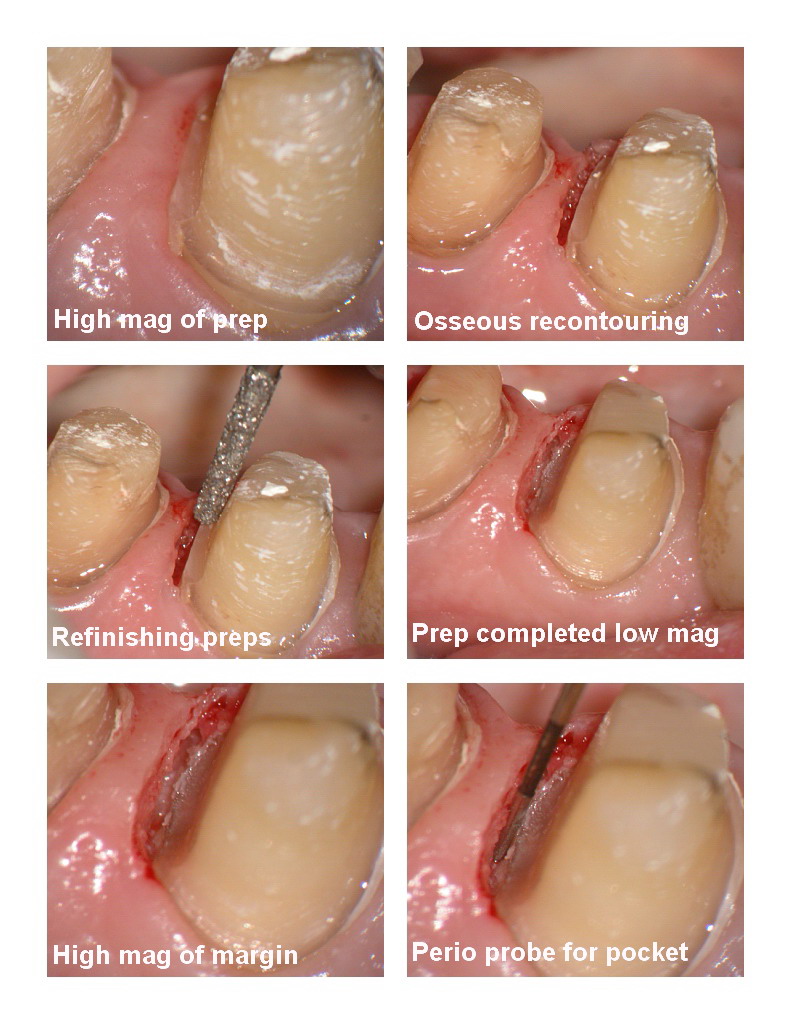
Glenn van AsSpectatorHi folks: I had this case to do today for my associate and I am still struggling with closed versus open flapped osseous recontouring.
I think that the pics are pretty good in this case to show you what I did but by no means is this the only way.
I have recently ordered some small instruments from Hartzell to try to do some mini flaps with osseous with the laser and then use the tiny sutures.
In this case this patient has recently undergone some changes in medication and has had alot of decay.
My associate did the endos on both lower premolars and then did some post and cores. (No PA of this) . He then quickly roughly prepped both teeth and placed provisionals on both. He then asked me to do some limited crown troughing to expose more tooth structure on the distal of both teeth.
I started with the 400 micron tip with water but not alot of air at 30 Hz and 130 mj with anesthetic. After treating the first premolar distal, I then switched to 30 Hz and 70 mj without water or air with a 600 micron tip to widen up the trough and get a little lateral displacement of the tissue.
After I had completed the osseous, I took the diamond bur back in there and got down to solid tooth structure because initially the preps were on composite resin.
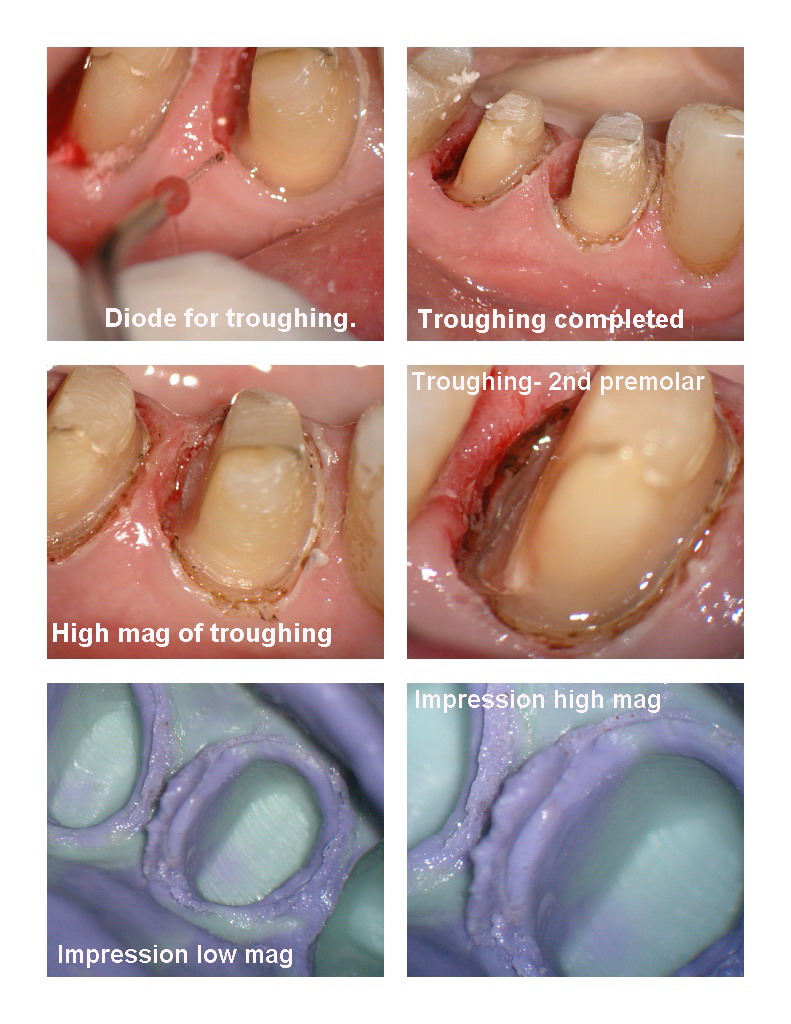
I then brought over an 810 diode to trough the tissue for the impressions and tissue control.
I had trouble getting the impressions (5mm below the tissue), until I used a putty/wash combination technique to force the light body down deep. I did use expasyl to widen the distals on both teeth prior to the putty/wash.
Now my question, I have showed you how I handled this case……..what would you do.
1. With respect to raising a full flap.
2. Sutures where and what type for open flap.
3. Would you use a diode for troughing.Would you have extracted both these teeth and placed implants??
Thanks guys……..I dont see alot of people posting open flap cases, but wish I would see some to help me learn how better to do these.
Glenn

vinceSpectatorHi Glen,
Great case. Nicely presented (as per usual).
Implants would not be a bad proposition for this patient due to the amount of caries they present with (mesial of 1.7, mesial of 4.6, distal of 4.4 and 4.5) and resultant compromised crown-root ratios of the premolars (especially 4.5). But if the patient wishes to keep the teeth I would have handled it the same as you did up until having established crown margins on sound tooth structure.
At that point I would have raised a FTF from the mesial of 4.3 to the distal of 4.6, on the lingual and buccal. Followed by osseous reduction in the interproximal areas between the PMs and the second PM and the 4.6 with blending to the buccal and lingual to re-establish biologic width and positive architecture. (Osseous would have been done with the Erbium.) Sutures would be gut (4.0). I would have then re-temped for 4-6 weeks for initial healing to take place then impress for the final crowns (diode to trough).
My two cents. Nice case.Take care.
SwpmnSpectatorGlenn:
In the preliminary case studies on closed crown lengthening(which I’ve only started this year) mine are done somewhat differently. I’m completely removing the interproximal gingiva with the Er:YAG. This allows me better visualization of osseous structures so that I can properly reduce the interproximal height and attempt to blend the osseous reduction facially/lingually and mesio-distally.
The interproximal gingiva on my cases is healing via secondary intention as I’m not reflecting a flap or placing sutures. Often I use the 810 nm diode laser at 3.0-4.0 Watts, non-initiated tip, defocused(out of contact) to affect a coagulum interproximally. So far we are seeing amazing regeneration at 1 week and patients are reporting no to minimal discomfort. I’ve shied away from taking the impression at same appointment we now schedule impression 4 weeks out and the diode laser is used for margin exposure.
The debate continues as to whether closed crown lengthening is a viable treatment alternative. On one hand by not reflecting a flap we may have less recession and root sensitivity on adjacent teeth. On the other hand with the closed procedure we may fail to properly reduce/blend osseous structures and may create an osseous defect. Prior to incorporating lasers into my practice, I have performed a similar closed technique using electrosurge and diamond burs and had some good results even taking impression same day and even in semi-esthetic areas such as teeth numbers 5 and 12.
Guess time will tell but I think in certain cases the closed closed osseous crown lengthening technique is a useful alternative.
Al
vinceSpectatorHi Al,
Very interesting way of doing this!
What parameters are you using with the Er:YAG to remove the interproximal gingiva, and from which direction to find this denudation to be most efficient (ie. from occlusal or from buccal/gingival)? Are you prescribing analgesics/rinses? Are you placing perio-pack?…
I would love to see some clinical pictures/ radiographs. Thanks for sharing this protocol.Regards,
Vince
ASISpectatorHi Glenn,
Nice handling of a difficult situation.
A flap would certainly allow better access to make sure a positive osseous architecture is created from the erbium reduction. Did you get a chance for a post-op PA?
Having a 5mm depth from crest of gingival tissue apically is rather difficult to maintain even after healing, not to mention the impression step as you had brought up. Perhaps more troughing might be needed to lower the tissue height. If not then, at least at the seating appointment as needed.
Root decay is a major problem. Will custom fluoride trays for home therapy be recommended?
Andrew
Glenn van AsSpectatorAlright you guys……..sheesh here are the answers…….
Vince you have an interesting idea about the FTF and how you would have waited for the healing and done it with traditional means. I would love for people to post a case that they have done this way using the laser. I have yet to see a single case posted this way and would love to do one side of the mouth this way and the other side of the mouth with closed flap and watch over the next few years the healing……now wouldnt that be cool.
Allen, I too have ablated the gingiva and let it heal by secondary intention on the first one I did. It healed very quickly (within 6 days) and was very non sensitive for the patient and now a year later is still holding on. I do agree with you in that it does seem to work but is a little barbaric for the periodontists. I agree that time will tell whether the closed flap is useful and whether there are long term sequelae that make its use not the front line treatment in cases like this.
Hi Vince, to remove the interproximal tissue I used first a 400 micron tip with water at 30 Hz and 140 mj or so….and it works quick and then I actually went to a 600 micron tip afterwards without water to ablate some tissue away to widen the tissue laterally. I used Expasyl as well to displace the tissue. I tired to create a 3mm pocket in that area.
I gave the patient Chlorhexidine rinse ( I did this Friday) and Advil or Toradol. NO pacs at all. Just recemented the relined temps.
Hi Andrew……no I didnt take a postop Pa but will this week to see how it looks. The expasyl helped with the impression but it took a putty and wash impression to get the margin. I can shave the tissue down if it doesnt work but implants seem to have a steepness to their exposure from the hex. The key is trying to get on solid tooth and then to create enough of a trough to get the impression of the area. It was tricky that is for sure.
Patient is on Fluoride trays now……bad decay. Mouth is dry from all meds……
Take care and talk to you this week.
Glenn
SwpmnSpectatorQUOTEAl
Very interesting way of doing this!
What parameters are you using with the Er:YAG to remove the interproximal gingiva, and from which direction to find this denudation to be most efficient (ie. from occlusal or from buccal/gingival)? Are you prescribing analgesics/rinses? Are you placing perio-pack?…
I would love to see some clinical pictures/ radiographs. Thanks for sharing this protocol.Regards,
VinceVince:
This is not my technique I learned it from Dr. van As and others plus it’s just a laser modification of an old technique that was performed with electrosurge and diamond burs.
Generally speaking I use 30 Hz 160 mJoules 600 micron tip and copious distilled water irrigation on bone. You can shut off the water to remove the interproximal gingiva but I would probably do that at a lower mJoule setting. I personally like to remove the tissue from an occlusal orientation but you can turn the tip perpendicular if necessary to reduce height or thin facial/lingual tissue.
I don’t use perio packs, some patients are on stannous fluoride and some patients are given twelve Vicodin ES. Some of the patients that we gave Vicodin reported using one or two. In other cases, over the counter ibuprofen or nothing has been taken.
I posted a similar case with photos some time ago in the hard tissue section:
http://www.rwebstudio.com/cgi-bin/ikonboard//topic.cgi?forum=25&topic=107
Al
dkimmelSpectatorGlenn ,
I really am getting sick of your microscope!
Looking at the pictures, I can see the bone between the margin and the trough. Doing the closed procedure with 4.5x loops , I can not see the bone without making a large trough. In most cases I end up doing as Allen does an just remove the tissue.
I am not getting a scope, I am not getting a scope. At least that is what my wife tells me!
DAvid -
AuthorPosts
