Forums › Laser Treatment Tips and Techniques › Hard Tissue Procedures › Lasers for extractions
- This topic is empty.
-
AuthorPosts
-
Glenn van AsSpectatorHi folks: its been painfully quiet in here for a while. Here is a case I did a couple of weeks ago and thought it might be interesting.
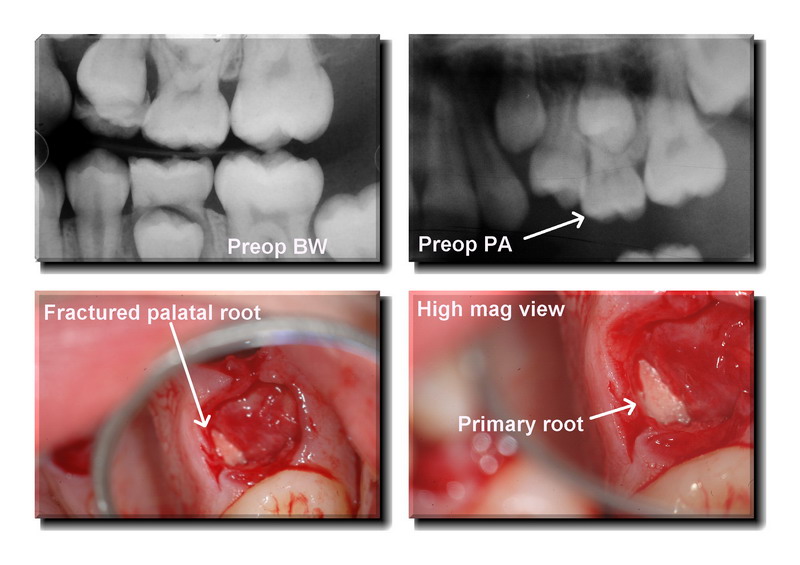
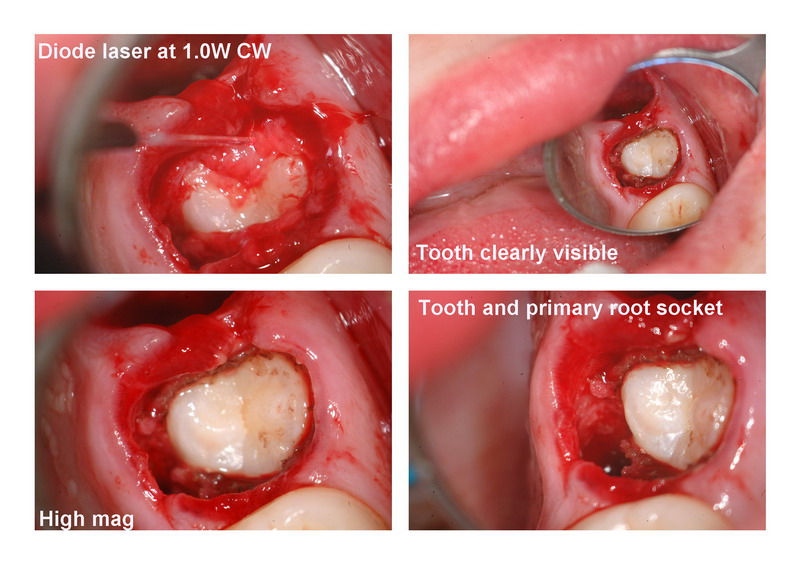
This is a yong 13 year old female with alot of crowding. Treatment included extraction of all permanent 1st premolars and the primary tooth on the upper left at the same time.
I have posted some preop radiographs and then when I extracted the primary molar I heard the tell tale “CLICK” which occurs at the same time as the crown is removed. It is typically followed by some short four letter words uttered quietly or thought loudly.
In this case given the orthodontics are being done the primary root had to be visualized (its great to have a scope), and then removed.
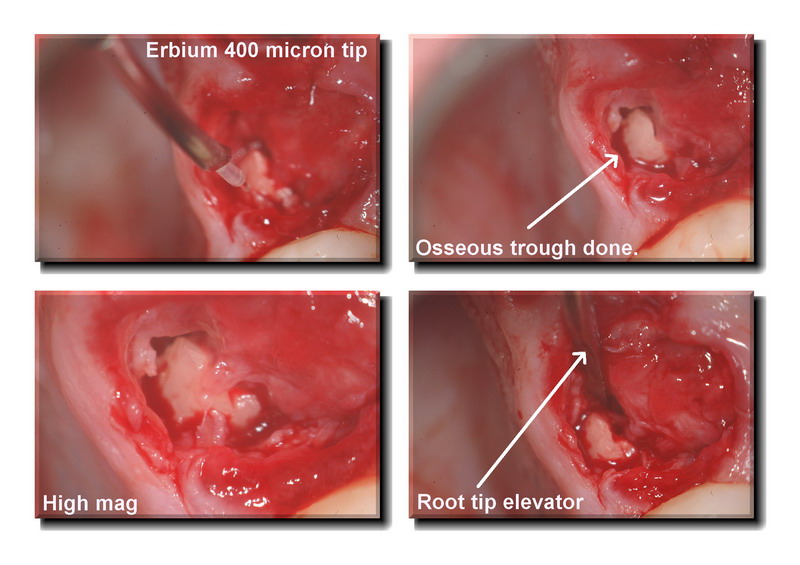
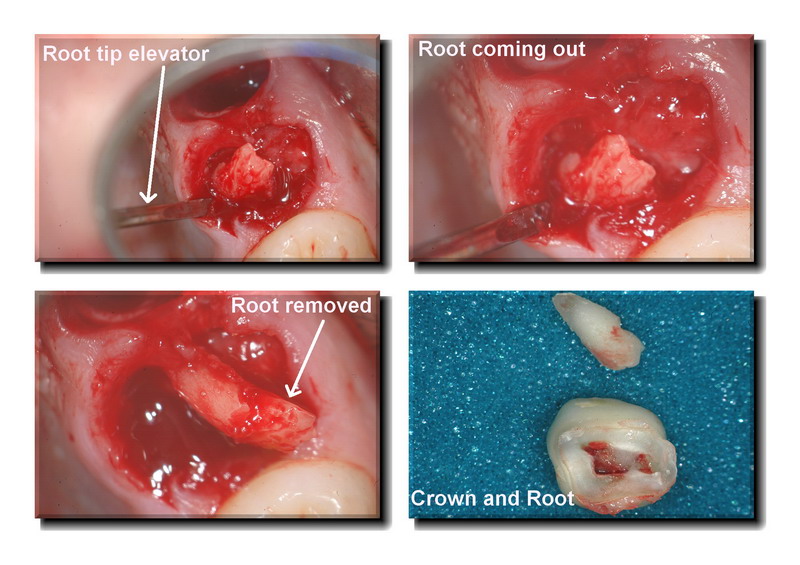
The erbium laser was chosen to create the osseous laser trough around the root so that a root tip elevator can be inserted and the root removed. Settings were water on, 40Hz and 110 mj or so. Not much air at all.
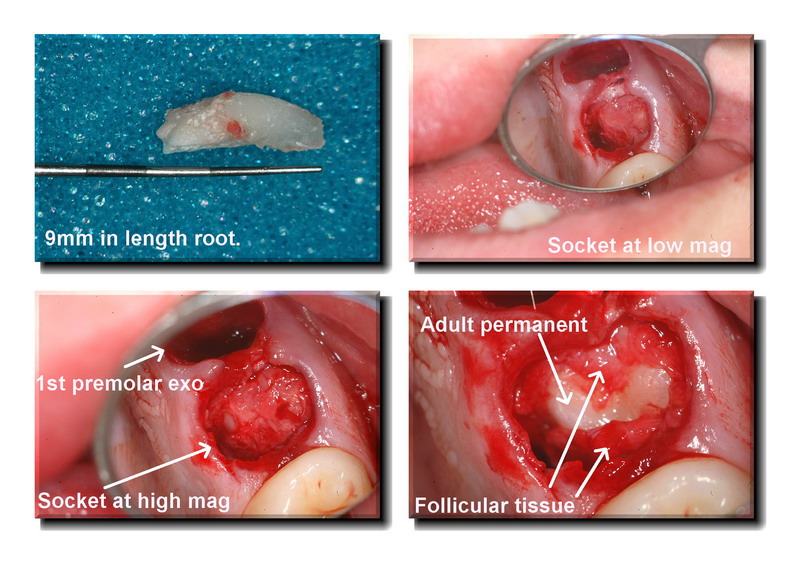
I then removed the 9mm root and decided to help the tooth along a little by using the diode to remove the overlying tissue (follicular tissue) and allow this tooth to come in faster and I used the diode to remove the tissue. Settings were 1.0w CW. Light air and water stream. The diode was used in contact as was the erbium.
I like the diode for coagulation in these cases as well. Maybe not quite as nice as Dr. Bobs NdYAG (cant speak from experience though) but it works.
Hope it creates some discussion, we cant have figured it all out in under 3 years can we??
Glenn

BenchwmerSpectatorHey Glenn,
Nice results, photos and documentation.
With a 550-650usec Nd:YAG pulse width, you could of created hemostatis by setting stable clots in your extraction sites and where the root tip was removed.
Great for third molars and patients on thinning meds.
I had a 50 year old patient leave the practice to save money with a dentist participating in his PPO a couple years ago. I’ve always treated him without taking him off his Coumiden. No problems with hemostatis after surgery and extraction. A couple months ago his new providers took him off his meds prior to a surgical procedure. he died three days later. Maybe it was his time, but his wife is back as a patient and blames his dental care as his cause of death.
I’m glad I never had to take him or my other patients off their meds.
When do you want that Nd:YAG shipped?
Jeff
SwpmnSpectatorNice case Glenn. The erbiums work well for this type of conservative extraction assistance. Sometimes these seemingly simple deciduous tooth extractions can be a real PIA can’t they?

Great job on placing tip and trough on the palatal side and not adjacent to the adult premolar. If we place the erbium tip on the side adjacent to the premolar we could have easily nicked up the adult tooth.
Glenn van AsSpectatorWow Jeff, what a story that is, makes you think about taking them off the coumadin.
I also want to say thanks to Allen, he is one of the brightest laser minds I know and he always takes the time to look in detail at the cases and notice things like the area I took the bone in this case. I didnt even mention it but Allen reads my mind alot of times……scary actually!!
It always feels like home here on LDF because Ron has created an atmosphere of togetherness despite differences in wavelengths or brands.
Its a testament to him and his vision.
Glenn
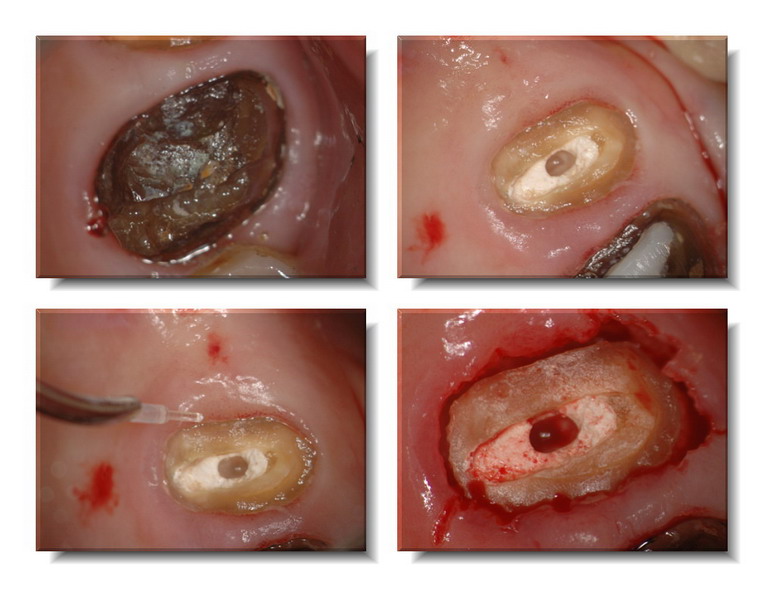
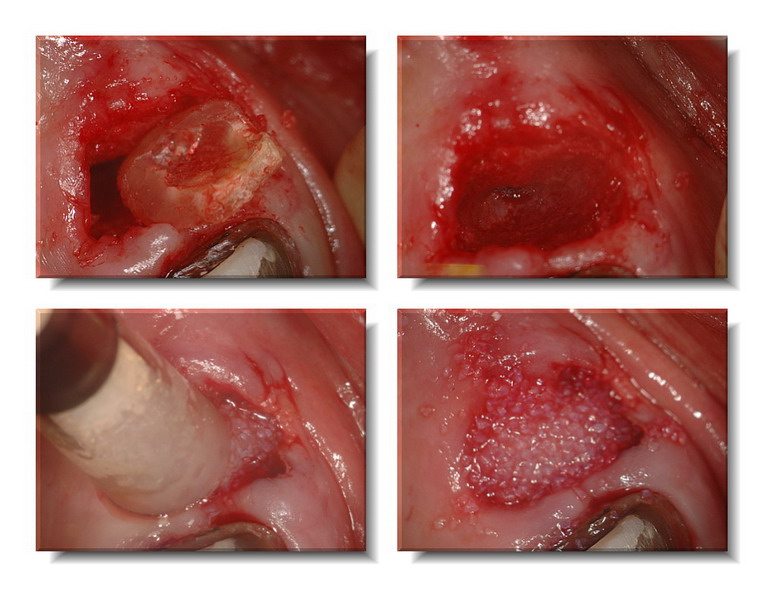
drkddsSpectatorSeeing a few of Glenn’s laser-assisted extraction cases inspired me to try one myself. This patient is my assistant’s husband. He was in the military and this tooth was neglected following a RCT. He came in with gross decay on the distal and an abscess on the distal root. The re-treat was completed and this tooth fractured about 6 weeks following the re-treat.

(Pic 1) I initially went in to explore the fracture. I was fairly certain it was hopeless, and it was, as it turned out. The tooth was fractured along the buccal aspect of both buccal orifices from mesial to distal. I decided to extract this tooth surgically exclusively using the DELight for access and bone removal.

Pic 2
After anesthesia, I used the DELight (45Hz, 55mJ +H2O, no air) to sever the gingival attachment. The buccal section was removed with tissue forceps. I gave in and removed the remaining Cavit temporary with the handpiece.

Pic 3
So I could have access to the pulpal floor I used the laser to remove the palatal axial wall of enamel (by angling the laser to cut palatal to buccal @ the CEJ) (20Hz, 400mJ) After removing the palatal wall I gained easy access to the pulpal floor. I sectioned the pulpal floor from mesial to distal and between the buccal roots. (20Hz, 400mJ). When I was able to visualize bleeding in the section I knew I was through the floor.

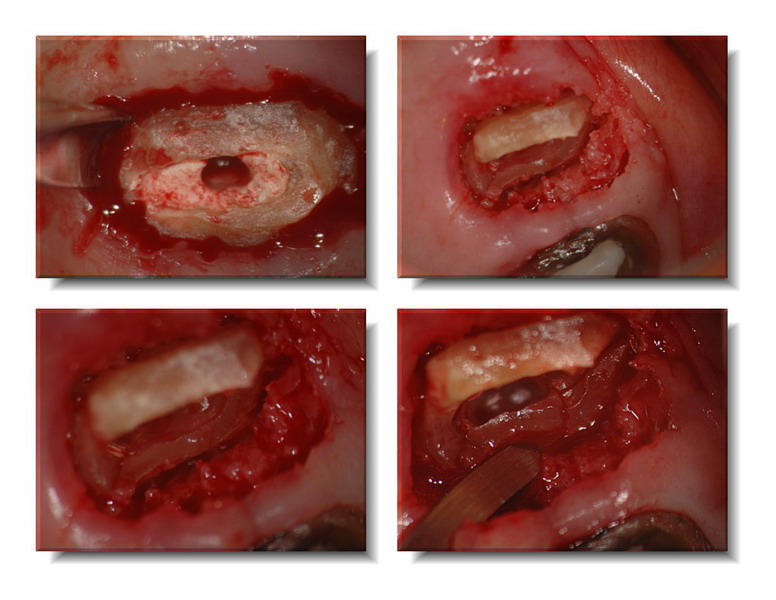
Pic 5
A straight elevator was used to luxate the buccal roots. They all but jumped out. Very little force was used due to the perfect purchase I had between the roots. I then used the laser to sever the palatal gingival attachment and removed bone around the palatal root (20Hz, 200mJ). Now I had a solid purchase on the palatal and buccal aspect of the palatal root, so I used the Rongeurs to twist the palatal root out, again, with minimal exertion.


I am very pleased with the result of this treatment. It went better than I could’ve hoped. There was very little bleeding (notice the pics) and minimal tissue damage or bony expansion. I was prepared to lay a flap, section with the HP and suture it closed. What a difference! The total treatment time after anesthesia time was 45 minutes, including pics. Neat use for the laser!! Thanks so much to all on the forum who posted cases like this. I would never have thought to use my laser like this. What a great service for the patient. Comments are appreciated, good or bad!!
(Edited by drkdds at 9:05 pm on Feb. 21, 2006)
(Edited by drkdds at 9:17 pm on Feb. 21, 2006)
Glenn van AsSpectatorAWESOME DOUG ….absolutely AWESOME
Its nice to see that what you did today I did the same but for a much easier premolar that was part of a bridge. If I have time I will post the case tonight.
What a great job you did…..look at the cut in the furca of the bone….
By the way , I used the same settings with the 400 micron tip myself today.
Kudos to you…great case, photos and documentation
CLAP CLAP CLAP
Glenn
drkddsSpectatorThanks, Glenn. Coming from you that means ALOT!
By the way, I used a 600nm 80 degree tip to cut the palatal axial wall. I then switched to a 400nm 80 degree tip for the sub-gingival and pulpal floor sectioning. Getting the correct angulaton to access the mesial portion of the tooth was a challenge. I found myself thinking about the 90 degree handpiece and chisel tip, but I just didn’t want to get up out of my chair. My 400nm tip did get beat up a bit, though.
I look forward, as always, to seeing your case, Glenn.
Are you, or is anyone here, going to the Townie Gathering Las Vegas in March?
(Edited by drkdds at 9:10 pm on Feb. 21, 2006)
brucesownSpectatorIntresting thread. I’ve started to use my DELight for troughing out those hopelessly broken down bicuspids. The one concern I have is that I occasionally have trouble getting the trough deep enough to get below the decayed part of the tooth and get purchase on something solid. Any suggestions? Is there a tip that has more of the fiber sticking out beyond the cannula? On the whole I enjoy using the laser as it usually avoids the necessity of raising a flap. You can do the same thing with a highspeed and no flap, but the collateral damage is hopelessly messy.
Just a note on coumadin. It is perfectly accetable ( from OMFS literature) to take out one or two teeth from someone on coumadin using local measures for hemostasis. The risk from having the patient off their meds is too high in most cases to justify the small amount of blood loss that is avoided by stopping the meds. Remember that it takes several days for the effects of coumadin to disappear and an equal time for it to reassert itself once it is recommenced. By all means check with the patient’s MD to see what their INR is. If you are concerned, let the surgeons have the case. Just like golf, one little stroke can ruin your whole day.
Cheers from Vancouver Island.
AnonymousGuestNice job, Doug. I’ve noticed a lack of bleeding with these also. Sometimes I wonder if there is enough.Make sure to post follow-ups if possible.
Bruce, those coumadin pts are nicely handled with a ndyag that has the ability to use a long pulse duration(Periolase).The ability to create a thermal clot really makes treating them a lot less stressful.
Glenn van AsSpectatorHi Doug……..its been too long for me since I have posted here. I saw Rons sig and felt guilty…..darn it all.
Its 2 am and I am in Vegas starting a lecture tomorrow and I cant sleep.
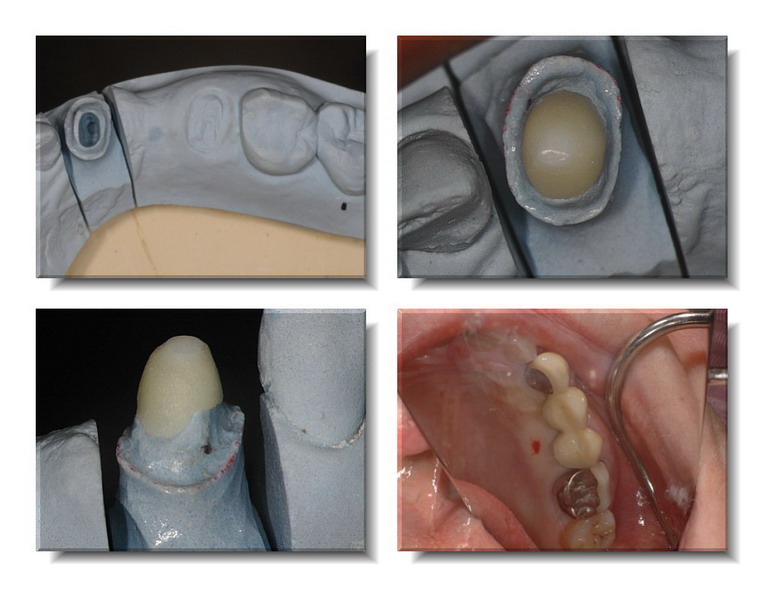
Here is that case I did the other day.
The original bridge from the premolar (2nd ) to the canine fractured and the patient doesnt want implants. I tried to salvage the canine, doing an endo on a completed calcified tooth, some crown lengthening and then it came in like this. I took and impression for a Procera Zirconium post that I cemented with Resin (after using the ErYAG laser to remove the smear layer).
The crown on the first molar was removed (yikes) and then the 2nd premolar was extracted ala Dougs case. I used a 4oo micron tip at 25 Hz and 200 mj with H20 to create a small trough……..crack , crack , crack. A little more troughing and presto mundo, out comes the root.
Placed in some Osseograf and put a piece of gauze over the osseograf til I took the temp and relined it. Didnt want all the extraction preservation material going all over the place. Will leave the temp in for 3 months and then will do an ovate pontic on both teeth that are missing.
The temp bridge is in place……..hope its interesting.
Glenn and PS its too late and to tiring for text , so just follow along….
Boy some of the socket photos through the scope showed RIGHT down to the bottom of the socket….talk about no bleeding!!…what a cool shot. Put that in at the end for you.
glenn



Glenn van AsSpectatorPs and here is a photo of the exo socket, sooooo coool to see to the bottom of the socket without any blood….
Glenn
[img]https://www.laserdentistryforum.com/attachments/upload/DSC_0007_resize.JPG[/img]
AnonymousGuestGlenn, if the guilt gets you posting this kind of stuff…I hope you stay feeling guilty. 😉
It seems like I’ve heard some debate lately about amount of bleeding and grafting. Did you stimulate a little more bleeding before placing the graft? If you hadn’t grafted would you have tried to get a little more bleeding so there would be a ‘full’ clot and good matrix for healing?
Thanks for posting.
Glenn van AsSpectatorHi there, great question Ron, there still was enough bleeding I think for the graft but that is a very good point. Look at the graft material it was pretty soaked . I didnt stimulate bleeding but I am pretty quick with the trigger finger as well on the camera (I know how to ge these types of photos ……..suction ……suction …….ok quick……….CLICK!!)
As for the other aspect, yes I thinkk that the Nd YAG induced clot is probably the way to go, I just find that the relining of the bridge causes all sorts of bleeding etc. I dont know how firm the clot is from the NdYAG and whether it will resists the pressure from the relined bridge pontic resting on it as the material sets.
This will.
Hope that answers it……..gotta run.
Tom Haney is here in 30 mins.
Glenn
PS I have more stuff I have been saving and will try to post as I get time.
Glenn
dkimmelSpectatorDoug nice case and gald to see you posting…
Glenn — sweet.
Ron are you using the Nd:Yag in cases like this to form the clot over the graft? Seems like it would be a great way to go instead of the barrier.. I ‘ve thought about doing this a couple of times but the op is getting smaller everyday and I get lazy sometimes in bringing the Periolase into the op. That and I like to put the pontic 2-3 mm into the extration site. Without out the barrier , I’ve be afraid of disruption of the clot and graft particals going everywhere during the cementation process. Then having to go back and laser again. Not a real big deal but a time management issue..
Robert Gregg DDSSpectatorNice cases Doug and Glenn!
What I have been doing lately is using the FRP Nd:YAG (Periolase) with long pulse to lase the extraction site, place Bio-Oss to all but the coronal 1/3, allowing the thixotrophic clotting blood to squeeze around the graft material, then lase to create a barrier clot.
I will try to locate and post a case. Seems to be working well, according to Del who placed implants into these areas recently.
Bob
-
AuthorPosts
