Forums › Laser Treatment Tips and Techniques › Hard Tissue Procedures › Pulsed Nd:YAG for Selective Stain & Caries Removal
- This topic is empty.
-
AuthorPosts
-
Robert Gregg DDSSpectatorGreetings All,
I will post the pictures when I get to the office later today, as I had planned to do yesterday. Del and I have a lecture today and I’ll have some time to upload the images.
In the mean time, some may want to see the reaction I got on Dental Town while trying to show and share the technical applications for plused Nd:YAG.
Instead I got grief over the necessity of care–something I never tried to address in the first place.
Thanks to Ron Schalter who made a much appreciated supporting post and made my technical point–it was about what the 1064 laser could and couldn’t do.
And thanks to David Kimmel who hit the nail on the head (borrowing from “Doctor Ed’s” hammer analogy) when he also posted and made a very important point about aggresive carious lesions in the elderly due to medications, dry mouth, poor saliva flow, and the inability to detect carious invasion into dentin using radiographs.
The caries extended 3mm into dentin! Talk about being surprised! I was expecting the stain to blow out and be left with healthy enamel. It started out as a simple case of stain removal–one reason I didn’t charge the patient is because I didn’t prepare her for the fee in advance. Oops. But again, that wasn’t the point I was trying to make….I wasn’t trying to make a statement about these sorts of class I situations. There’s the Congress of Microdentistry, Kim Kutsch, Stu Rosenberg, and others to make that case.
Anyway, thanks or the support, guys, it’s greatly appreciated.
Now I know what Glenn van As means about the hostility to technology and his previous clinical posts on Dental Town!!! Geez, just trying to share technical capabilities and some differnt ways of solving clinical problems and some of those people get TWISTED about it!

http://www.dentaltown.com/idealbb/view.asp?sessionID={DC5AF088-EE75-477D-A1D6-81103B24213A}&topicID=16692″ target=”_blank”>http://www.dentaltown.com/gold….
http
Glenn van AsSpectatorHi Bob………I added a reply in your support……its a shame when information isnt shared with criticism that is constructive instead of destructive.
That is why Rons laser forum prospers……we may not always agree with the treatment or ideas but we have an air here of professionalism and cordiality in the posts.
That is what makes people want to post their cases.
Glenn
Robert GreggParticipantGlenn,
Thanks very, very much. Your comments were AWESOME. Thanks so much for your support. It helped me a GREAT deal!
I have to admit, I was really overwhelmed by the personal nature of the attacks. I understand now what you have been telling me about your previous Dental Town posts! WOW!
I also want to thank Rod Kurthy for being so incredibly supportive of me as well. I’m am really overwhelmed by the kind words and the time Rod and Glenn took out of your Saturday’s and busy schedules to come to the moral and professional support of a friend.
You guys are TOP drawer!!
Glenn, I agree completely with your assessment of the Nd:YAG as a dedicated soft tissue laser with some limited hard tissue uses. Hard tissue removal is one of the ways to try to distinguish Nd:YAG’s performance from a soft tissue only diode that is not free-running (with all of that emission mode’s advantages and capabilities).
Thanks again for all your support, my friends!
(Edited by Robert Gregg at 10:12 pm on May 17, 2003)
Robert GreggParticipantOK Gang,
Here’s the series if you haven’t already seen it. Better images here at Ron’s Forum and a more receptive audience. Sorry about the image sizes Ron–I’m still trying to make adjustments.
Pulsed Nd:YAG lasers are often thought of as ONLY “soft tissue” or periodontal lasers. However, pulsed Nd:YAG lasers have FDA clearance for hard tissue “indications for use”. One FDA clearance is for “enamel caries removal”. That is the removal of organic pigmented debris on and within the pits and fissures of Class I occlusal surfaces. The Nd:YAG 1064 nanometer wavelength is highly absorbed in chromatic pigments whereas this wavelength has very little effect on healthy enamel or water.
The high peak powers that a “free-running” pulsed laser (neodymium or erbium) can generate are powers on the order of 2000 to 3000 watts per pulse for one to two hundred MILLIONTHS of a second (microseconds) allowing the target tissue to reach it’s ablation threshold VERY rapidly resulting in rapid removal of the target substrate/pigment.

Pre-Op photo of the lower right second bicuspid on a 60 year old female with full compliment of teeth. Patient has stain and organic debris on the occlusal surface, as well as in the pits and fissures. To remove this debris with air abrasion, erbium laser or a diamond or fissurotomy bur before determining if there is decay present, could result in prepping a tooth that only has stain. Air slurry polishers might work nicely to remove the organic stain and reveal any remaining decay. However, having a laser that will selectively remove ONLY the organic stain or decay, and NOT any healthy enamel–and do so in microseconds–and before committing the patient and the tooth to a full resoration is a nice application if you indeed have such a device available.

Pulsed Nd:YAG at 100 microseconds (usec) Pulse Duration, at 3.00 watts of “average power”, 300 millijoules per pulse (mj/p), and 10 pulses per second (Hz) gives the operator 3000 watts per pulse. The stain and organic debris on the occlusal surface acts as an “initiator” or an activating pigment. Not unlike water does for erbium lasers. This was very interactive at this stage. No anesthesia was used. No “painting” of the tooth to create laser analgesia was used. No black suma ink “initiator” was used. No simultaneous water or air spray was used to cool the tooth. The patient was comfortable throughout.

Carbon deposits build up, even at short pulse durations, in the absence of water. Plasma and the ejected vaporized organic debris coat the tooth with a grey colored film. Water was sprayed on the tooth and the carbon was easily removed by lasing the discoloration THROUGH the water, obtaining absorption in the carbon, and preventing oxidation. This is a view into the occlusal pits and fissures.
Selective “photothermalysis” (a favorite term of my laser friend Geza) means I was able to remove the organic debris on and around the pits and fissures, but there is clearly more debris and/or decay present.
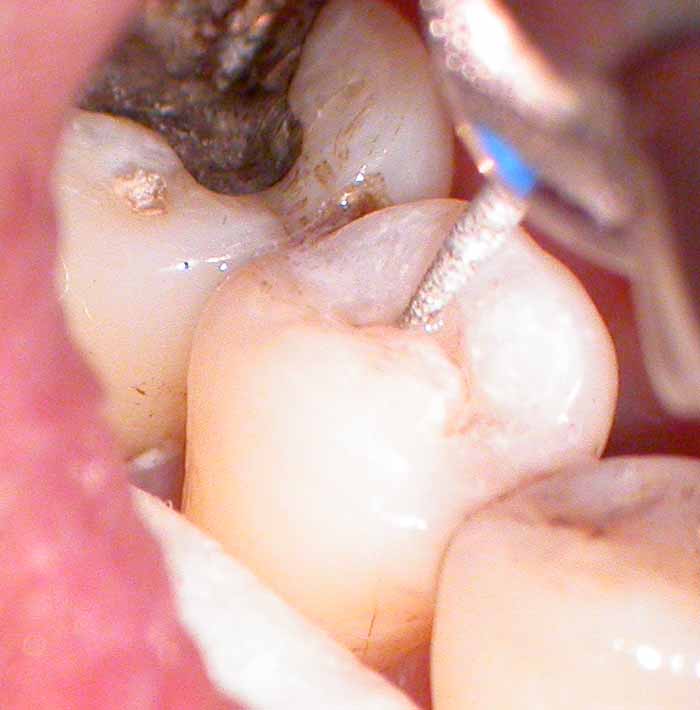
The inverted “V” pattern of decay once it hits dentin makes it necessary to remove enamel. The pulsed Nd:YAG will not do this. It will, however, remove decay and dentin if access is available.
So at this stage, the clinician can choose their own preference in accessing dentin and removing enamel–air abrasion, free-running pulsed erbium lasers, fissurotomy burs, etc.
In this case I used a flame diamond to open up the groove. Again, no anesthesia was used and the patient remained comfortable.

Enamel walls opened up, dentin and decay were accessed and removed with both the effect of the diamond and the use of the pulsed Nd:YAG.
Again, no anesthesia or any other effects were needed to remove decay or diseased dentin in this instance.

Tooth after etching with 37% Bisco phosphoric acid.

Bonding agent placed……..

Flowable composite placed, and polymerized with a pulsed Argon laser.
(One of the few contructive criticizms was about my use of a flowable composite. I agree, it is not the best choice for occlusal surfaces, since it is not highly filled. I simply was NOT planning on doing this for the patient as I thought it would only be a stain removal situation.)
Bob
(Edited by Robert Gregg at 10:31 pm on May 17, 2003)
AnonymousGuestBob, the images here are much clearer than on DT. You can see the ‘hole’ started in the bi.
Just to be sure I understand, is the area circled in black (below) the area of carbonization (gray,dusty appearing)?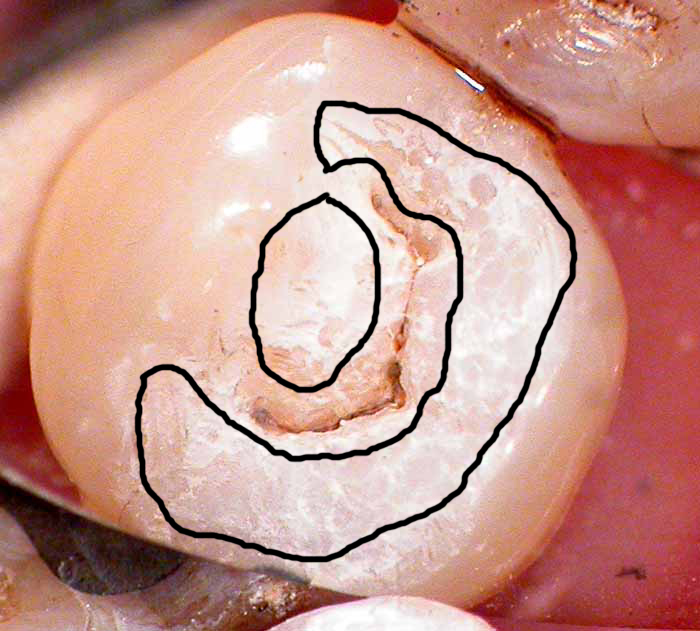
Thanks
BNelsonSpectatorBob
Sorry I missed all the excitement on DT. The negative comments often encountered is one of the reasons I seldom visit it anymore, and would seldom consider posting on it. More power to you. This forum I find much more informative and the caliber of doctors posting much more professional and helpful. Thanks for the great pictures and sharing this case. Isn’t this the exact kind of case that SS White makes fissurotomy burs for, and I have never heard any negative comments in DT about Howard advertising them in the magazine. So what’s with all the crap (excuse the French, Please) with using the laser for the same thing?
Thanks for your usual level of exceptional professionalism and insite in presenting this.
Robert GreggParticipantThanks Bruce for the kind words. Whew! It was not an enjoyable experience.
Ron, that “dusty” area is actually laser etched enamel. It is not the carbonization. I didn’t take a photo of that. It looks awful! This surface appearance is what shows up after the carbon is removed after water is sprayed on the tooth, and then the (black and gray) carbon is vaporized away.
As you might imagine and maybe see, this is a very thin etched layer. It can be polished off with a brownie point. So, that would leave one to conclude that the Nd:YAG laser etch is weaker than Phos Acid etch right? Yep! Fr Nd:YAG etched enamel alone is a weaker etch than P/A. Bond strength studies and practical clinical applications—like bonding brackets—demonstrated that 11 years ago.
So what’s the value of doing it? None, other than it’s the result of getting stain off. Will it accept a P/A etch and bond? Yes, and look how the P/A etch dissolved some of that already etched enamel surface. So it is a reeeally shallow layer of bond that will brux away during chewing…..
Bob
AnonymousGuestCouple more questions if you don’t mind, Bob.
If there were no pigment present (stain) would you still get etch effect? A recent article in ESOLA journal mentions melting of enamel and dentin surfaces by nd:YAG, is this what would happen w/o the presence of the stain?
If there is some melting and recrystallization, is the tissue more resistant to acid?
Thanks,
BenchwmerSpectatorBob,
I got a blurb in May’s DT Magazine on Should I buy a “Water”laser?, opposite the Opus Ad and before the 2 page BioLase center spread.
At least I got top billing.
Jeff
Robert GreggParticipantJeff,
Is that DT mean Dental Town or Dentistry Today??? I’ll check it out. Did you get some ink or face-time??
Ron,
Sorry to take so long to respond. Gettin busy around here!
“If there were no pigment present (stain) would you still get etch effect?”
No. There has to be something organic on or in the enamel for the Nd:YAG to absorb into. Unless it is dentin. Then it looks like this:
[img]https://www.laserdentistryforum.com/attachments/upload/NdYAGetcheddentin.JPG[/img]
A recent article in ESOLA journal mentions melting of enamel and dentin surfaces by nd:YAG, is this what would happen w/o the presence of the stain?”
Which article was that? Fried’s?
I don’t think so, is the answer to the question I think you are asking. Organic material must be present at or pretty darn close to the surface for the Nd:YAG to have an effect. Due to the focal length (spot size) the energy density drops down too much for any absorbtion to occur at the CEJ below that enamel (unless air or a passage way exists).
Did that answer your question?
“If there is some melting and recrystallization, is the tissue more resistant to acid?”
Oh, Yes. How much and how long, etc., I don’t know (or I forgot).
Bob
BenchwmerSpectatorBob,
Picture and info on May issue of Dental Town, page 38.
Today, The Severna Park Voice (5/15/03 issue), local weekly newspaper, had an original article I wrote Advances in Laser Dentistry/Technology w/ photo.
Mentions LPT and Erbium uses.
Jeff
AnonymousGuest“Morphological and Compositional Changes of Human Dentin after er:YAG Laser Irradiation”
Koukichi Matsumoto,Mozammal Hossain,….
Volume 3 Number 1
Spring 2003 page 17 under discussion
-
AuthorPosts
