Forums › Laser Treatment Tips and Techniques › Hard Tissue Procedures › 2 laser case
- This topic is empty.
-
AuthorPosts
-
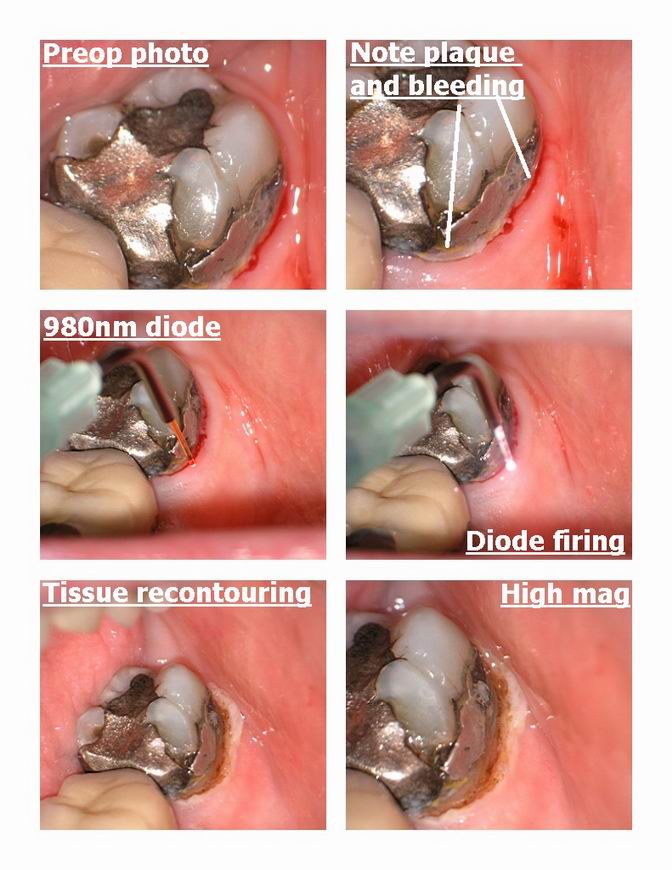
Glenn van AsSpectatorHi folks: second last case before I go on holidays.
I did this with anesthetic as a buildup prior to a crown being down.
I removed the tissue on the buccal with a diode because there was plaque and inflammation and the eribum often will increase the bleeding in a case like this.
Diode set at 2 w .02 on and off.
Nice result I think and it allowed me to get the clamp on without inflammation and seepage.
Removed the amalgam and then used the laser to remove the smear layer and in addition to sterilize the prep. Nice etching……..this laser of course was the erbium yag hard tissue laser , unfortunately no hk here but I still managed to get a half decent result , amazing huh.
The tooth is slated for a crown but still wanted to show you the result.
Cya
Glenn


vinceSpectatorNice case Glen.
With the 980, did you use water to cool also?
Later, Vince
Glenn van AsSpectatorThanks Vince…….yes I did use the water, and thanks for the kind words.
glenn
SwpmnSpectatorWill that 980 ablate “optically”, in other words, out of contact as the company claims? Are you contacting the tissue in these photos?
Great composite!!!!! You might just watch it, that thing will probably last for years.
Al
Glenn van AsSpectatorHi Alan…….great question about the optically cutting. I think what they mean is that this laser because it can be flooded on the tip with water and still cut , is not as thermal in its cutting etiology as other diodes.
I know you can flood it with water and have it cut.
I know it is slower to do this than a thermal cut.
I know that the healing is pretty darn good.
As for the rest, I havent played with it enough to really give you a firm idea.
By the way great questions, thanks for the kind words about the composite and just to advise the people here that I will be on vacation for the next week and maybe two, so I wont be around much.
I will return in September though.
Cya
Glenn
marc andre gagnonSpectatorIn this case I think that Glenn is using a 810um diode with is a laser that work like a hot knife.In a case like that ,he only can work without water and with anesthesic.If you want to work without anesthesic you can use a 980um laser from biolitec.It’s the only wavelenght that stop bleading without contact.I can do a case like that with my 980um biolitec with water and no anesthesic.we do case like that with no anesthesic .We use topical anesthesic in some case when the patient doesn’t feel well with the dental clamps.
We can see in this case a beautifull work and terrific photos .
Thanks Glenn for subject.
SwpmnSpectatorMarc:
One of Glenn’s photos is labeled “980nm diode” plus he uses the same 810nm DioDent I do and the tip in these photos sure doesn’t look like mine.
Thanks for the input on the Biolitec.
Al
vinceSpectatorHi Allen,
I use the 980, and it does coagulate optically, with lots of water, out of contact. No charring whatsover. The patients also appear very comfortable without LA for minor plasties, crown troughing….
Cheers, Vince
SwpmnSpectatorThanks Vince!!!!
Al
Robert Gregg DDSSpectatorHi All,
Glenn, beautiful case and use of different laser devices.
I think the CW/gated pulsed 980 may be the best near-infrared diode wavelength and the Biolitec very well the best of all the existing diode devices.
Having said that, I have some commentary about this discussion.
Pardon me, if you will, but my goal–as a clinician and a manufacturer–is to see that physics, devices and laser tissue interactions are accurately represented–no matter what laser wavelength or certain manufacturers claim in their marketing attempts to make their device seem unique.
A few comments:
1. Sure 980nm coagulates “optically”–I’m unaware of a near-infrared thermal laser that doesn’t?:confused:
2. I must respectfully disagree with Andre. 980 is not the only wavelength that can stop bleeding without contact. Pulsed Nd:YAG as well as pulsed Holmium:YAG and CO2 will do so as well.
In fact, when the pulse duration is very short in pulsed Nd:YAGs (100-150usec and very high peak powers) the way in which one achieves hemostasis is to defocus (reduce the cutting effect of peak powers) and “warm” the blood to create thermolytic hemostasis. This gets harder to do when the blood flow exceeds the ability to coagulate the surface blood. That’s where extending the pulse duration (pulse time) while keeping pulse energy intensity with full energy as called for–hence the warming time in tissue–allows hemostasis even in the deepest recesses of pockets, where “de-focusing” with CW diodes will not work due to surrounding tissue dissipating the ever “extinguishing” energy.
The “High Fluence” technique with water lavage helps to address this energy extinction with CW diodes, but is not possible deep in closed pockets.
3. Be very careful when using water to “cool” tissue at high fluences with ANY near-infrared wavelength “true” pulsed, gated or CW. 980nm is completely transparent to and in water. The infrared pouring into tissue is the same infrared energy passing through clouds on a sun-less summer day–you can still get a sunburn (UV light notwithstanding).
Water cools the glass fiber and reduces the hot glass effect, but doesn’t cool the soft tissue in the irradiated volume. That’s why is cuts slower, but warms more. But remember the caution learned a long time ago, “Low-Low is a No-No”. Low powers, low pulse repetition rates, cause tissue warming and tissue death with less cutting.
With all near-infrared wavelengths (810-1500nm), the clinician must be very careful not to warm the surrounding connective tissues that do not absorb near-infrared energy very well–except to warm to the point of irreversible thermal necrosis!
The water spray, since it excludes oxygen needed to carbonize the surface of the tissue, gives the impression of less thermal insult, when in fact the reverse is true. That’s why you get the “coagulation”! As long as it is the blood absorbing the “warmimg”–no problem with underlying CT. But when water spray is used to blow off the blood, CT is exposed to warming.
Now it takes a little while for the CT to warm up to the point of coagulation necrosis–but it will occur if too much time is spent on one area, especially where the tissue is thin……..
Ask me how I know…….4 years after I started using lasers, and thinking I was pretty sure of myself, it happened to me on 2 centrals, and a couple of posterior molars. Not fun, not good. The tissue regenerates eventually (remarkably) in most cases, but not before a lot of ugly tissue sloughing and 2 weeks of very, very painful burn recovery.
4. Take a very close look at the 3rd and 4th photos that Glenn posted. Take note of the 4th photo labeled “Diode firing”. Notice how the fiber is intensely bluish-white in its appearance, but not so much the tissue in comparison. Now look at photo #3, labelled “980nm diode”. The fiber has its characteristic brown/amber appearance when there is no near-infrared energy coursing through it. Glenn’s 3-Chip camera on his microscope is able to detect near-infrared, and it shows up as bluish-white in photos.
It should cause all to take pause and consider why so much laser energy is “leaking” (hemorrhaging?) out of the side of the fiber. So what is the actual therapeutic energy delivered to tissue? Is a Molectron PM600 power meter being used to measure the actual power at the fiber tip
 Is this why “High Fluence” is needed in some situations? (I’m not crticizing Glenn, this case, or anyone’s clinical technique here). But think about it……
Is this why “High Fluence” is needed in some situations? (I’m not crticizing Glenn, this case, or anyone’s clinical technique here). But think about it……Del and I have tried to raise this issue of “lossey” (as it is known to the fiber optic engineers) with the manufacturers of these fibers, but we have been repeatedly dismissed. Lossey can be corrected by increasing the number of polyimide resin “coats” on the exterior of the fiber, but the current manufacturers don’t do it except as a “special order” and a “special” additional cost. Another case of engineers and manufacturers refusing to listen to their customers and clinicians. They tell us we are the only ones that ever mention it. Maybe we have the technology and experience to detect it! Like Glenn’s technology and photo shows…..
I will try to post a picture of a fiber we now use, with a high intensity pulsed near-infrared emitting and irradiating tissue to see what the fiber looks like compared to the tissue.
Thanks to anyone who followed that essay to the end!
And thanks again to Glenn for you excellent case presentation and ecellent use of these lasers in this case.
Bob.
P.S. Knowing that Glenn uses an argon laser to RAPID cure his composite, I noticed the absolute absence of any “white line” around his composite………very cool.
(Edited by Robert Gregg DDS at 12:58 pm on Sep. 5, 2003)
Robert Gregg DDSSpectatorOk, here are some photos I took today with the Global microscope and the 3-chip camera with near-infrared sensitivity.
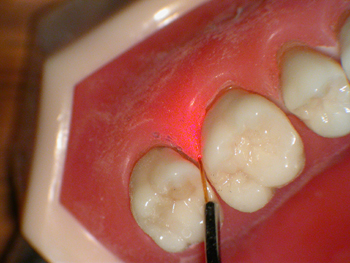
Figure 1. Shows the brightness (intensity) of the 1 MilliWatt HeNe beam 650nm visible light. Detectable by human eyes and the camera used here. No appearance of red photons exiting the fiber from the sides

Figure 2. With the microscope light turned off, this photo shows the brightness (intensity) of the 1 MilliWatt HeNe beam 650nm visible light into tissue–“Forward Penetration”. Detectable by human eyes and the camera used here. No appearance of red photons exiting the fiber from the sides. Notice scattering, reflection, and transmission of the red photons into typodont “tissues”.

Figure 3. With the microscope light turned ON, this photo shows the brightness (intensity) of the Fr pulsed Nd:YAG at the fiber TIP. NOT detectable by human eyes but by the camera used here. No appearance of near-infrared photons exiting the fiber from the sides.
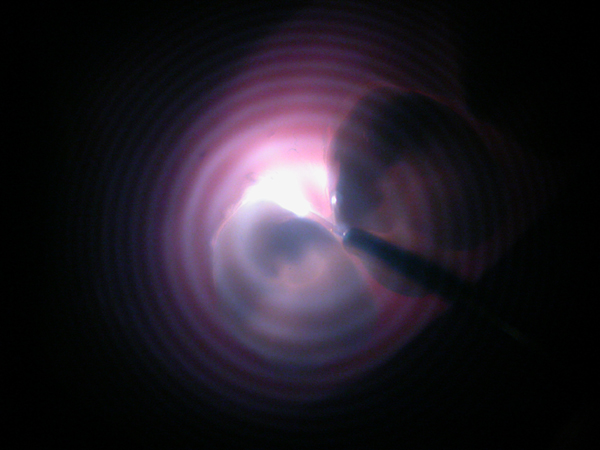
Figure 4. With the microscope light turned OFF, this photo shows the brightness (intensity) of the Fr pulsed Nd:YAG at the fiber TIP and into “tissue”. NOT detectable by human eyes but by the camera used here. No appearance of near-infrared photons exiting the fiber from the sides.
Kinda cool……..
That’s what I mean about intensity of a working beam delivered into tissue at depth w/o loosing its intensity (brightness) from the sides of the fiber or the sides of the tissue next to where you want to irradiate.
The pulsed near-infrared Neodymium YAG is easily 4 time brighter and more intense than the red HeNe beam. No “lossey” in this fiber.
Because these lasers are pulsed in the microseconds, they have peak powers on the order of 2000 watts per pulse, but ON for only 1/500th or so of the “duty cycle”….. versus always ON with a low powered CW or gated diode that never achieves much forward intensity (penetration).
That’s why there are no diode erbiums–only free-running (microsecond) pulsed erbiums. It’s the physics.
But that photonic performace doesn’t come on the cheap. The “engines” needed to deliver these peak powers are more costly than the arrays for CW diodes. If you want maximum control over tissue interactions (cutting tooth structure or coagulating soft tissue in deep bleeders), you have to “pay for what you want to get”.
Have a great weekend everyone!
Bob
(Edited by Robert Gregg DDS at 6:02 pm on Sep. 5, 2003)
vinceSpectatorGreat stuff Dr. Gregg! Really excellent photographic explanations.
Regards
Glenn van AsSpectatorBob: I gotta tell you that I read every word of your post. I spent all day lecturing about lasers today, hard soft , diodes, ndyags erbium yags and of course the er cr YsGG as well.
I think I know a little but posts like yours always humble me. I will admit that when I had the Laser turned on with my blue lossy light I dont remember if I was just holding the laser steady for the pic or actually cutting.
I really learned alot from your post and will reread it.
What a phenomenal teaching tool your posts were. Absolutely fantastic.
I know that you feel so passionate about the Nd Yag and you should after all the work Del and you put into it.
I want to congratulate you for all the efforts you put into educating us, and the posts here today were 2nd to none. They may have been the best posts I have read on lasers in a long long time.
Thanks again, that was an excellent demonstration.
All the best,
and WOW is all I can say.
Humbly yours,
Glenn
Robert Gregg DDSSpectatorGlenn–Thanks so much for your kind and gracious words.
No need to feel humbled, I hope you know that wasn’t my intent.
We all here, including me, are regularly humbled by your clinical, laser, microscopic, and laser prowess!
I hope it was clear my posts were not directed at your excellent clinical skills and results, nor your superb use and control of all of your laser devices, as I have the utmost respect for you in all those ways and many more.
I hope it was also clear that I was focusing on two really unique photos (that you so excellently took), and just a very subtle observation about how near-infrared (N-IR) transmits through fibers given different Temporal Emission Modes (TEM) and different quartz fiber-optics that many assume are all the same in their effects and results.
It was such a unique opportunity to demonstrate with photos what Del and I try to explain in words, but often come up short in getting our point accross about beam intensity at the fiber tip and keeping that intensity at depth in a pocket or after submersion of the tip in tissue.
It’s the same for pulsed FR Erbium lasers, as it is for pulsed FR Neodymium lasers like our PerioLase. They “renew” their intensity with each and every new pulse that is generated in the laser head and transmitted down and out the fiber tip. “True” pulsed (free-running) lasers are not dependent on the fiber tip itself interacting with the tissue. Just the photons or the acoustical-mechanical, or plasma generated as a result of high intensity peak powers.
.
We’re passionate about our laser, sure. But that wasn’t the point. We are just as passionate (deeply intense?;) ) about educating others about the manner in which ALL lasers actually interact with tissue. With everyone (clinicians, engineers, manufacturers) hopefully having a better understanding of what is actually taking place, we can better advance the device and peripheral technology that manufacturers might develop and use better device and peripheral configurations in the future for all laser types–as we have done with the multi-variable pulsed, digital pulsed Nd:YAG that we designed.As for my other comments about water cooling tissue with N-IR, I just don’t want anyone to make false clinical assumptions based on clinicians repeating marketing claims that end up causing unnecessary patient pain and injury.
I’m not saying any particular laser device is “bad”, not at all! But different device configurations have different performance characteristics, and the clinician ought to have an accurate understanding of how their device is actually interacting with tissue. Whether hard tissue thermal and photoacoustical ablation of enamel with Mid-IR Erbiums (including YSGG), or thermal photocoagulation of soft tissue with pulsed or CW N-IR lasers, let’s speak knowledgeably and accurately about the actual mechanisms. It’s our patients and my colleagues I am ultimately concerned about, not the stock performance of a publically traded company.
Just as an aside, Del and I have worked extremely hard to keep our company a private “boutique” company that focuses on laser science, clinical results, our dentist customers and their patients. We’ve turned down several offers to “go public”, or some such scheme and make a lot of money. We aren’t rich, and sometimes we struggle, but we do have the freedom to slow-grow our company based on sound science and solid technology. And we’re free of the pressure from “outside” investors who want a quick ROI or “liquidity event” or an “exit horizon” shorter than it takes to prove the science and before the science has really matured.
As we know, some laser companies and some laser clinicians don’t care how it works, just as long as it works and sales continue based on some un-proven theory of how it works……..Not a way to get mainstream dentists to buy, or expand the market very much.
But I’ve been around for over 13 years using all sorts of lasers from all sorts of companies–and witnessed a dozen laser manufacturers and their laser devices come and go. That doesn’t instill confidence in the dental profession at-large. But I’ll still be a laser clinician after some of the companies here today have gone and other companies have replaced them. Maybe Millennium will stick around a while longer than most. Longevity, not “flash-in-the-pan” is our goal. So I get real tired of “outsiders”, with the help of a few of our professional own, doing you-know-what where I make my living and call Home–the profession of dentistry–and leaving it to me and my laser colleagues to clean up the mess after they have made their money and gone on to something else to profit from!!
Sorry for the rant, but Geeeeezz……..
So, many thanks, Glenn for graciously allowing me to intrude on your clinical post and share some photo-dynamics of laser “TEM’s” and fiber optic coatings….and a few rants!
All the best,
Bob
ASISpectatorHi Bob & Glenn,
Bob, your sincere enthusiam on laser dentistry comes through crystal clear. You are a credit to dentistry and a treasury of laser physics and education.
The very same can easily be said about you, Glenn. Your documentation of clinical procedures are setting a whole new standard.
Thank you so much for sharing.
Andrew
-
AuthorPosts
