Forums › Erbium Lasers › General Erbium Discussion › Closed crown lengthening, a biologic understanding
- This topic is empty.
-
AuthorPosts
-
Glenn van AsSpectatorBill: I have a case now which was my first case in the office that I did osseous surgery on. In that case I literally ablated the tissue and bone between the papillae of the maxillary lateral and canine so that I could get the margins placed on solid tooth.
I am embarrassed that I did the case that way , but its done.
I saw him last week and it was one year or so after this was done and the crowns looked great (remarkable but true).
I will phone him and get him back for some photos for you.
I am glad that you come here to learn. I dont mind constructive criticism, as you have levelled at me before at DT. I showed the case which has healed fine.
It is there for you to see.
In addition Danny asked me privately to comment on the osseous cases.
First off, most of them are not cases that I would have done in my office at present as the bone was too much for me to take off with the laser.
2nd off, I will tell you that the tips of the DeLight laser can be either 400 , 600 micron, and the chisel tip which I have shown is much much bigger than that and the footprint of this gives you a nice cut on bone.
I have shied away from closed crown lengthening because of what Danny and others have said for all but very simple cases.
In closing, I will say that osseous with the laser for bone removal in an open flap environment shouldnt even be discussed as a viable alternative to traditional methods……..IT IS …..PERIOD.
There are some advantages in my opinion to the laser…..
1. Non contact, quieter in the DeLight case than a turbine.
2. Water spray has much less splatter than with a handpiece.
3. It is slower than a bur but you can be very precise in your bone removal , flaking of bone that covers a follicle predictablely without risk of damage to the follicle or tooth underneath.Some can claim th at periotomes and other assorted chisels can do the same thing (these are the same people who have never even used the laser!!), and that is fine.
All I am saying is that the laser does work on bone, safely and precisely and if you use it open flap there is no reason it cannot be used as an adjunct to traditional methods and in some instances I suspect it will become the treatment of choice.
I will try to post some of my follow up cases and their healing, one of the difficulties for me is that I have two scopes in my treatment areas and none in my hygiene areas yet (but it is coming) so its not as easy for me to take the pictures postoperatively with the same magnification as in my operatories.
Take care……….
Glenn
Dan MelkerSpectatorGlenn,
Thank you for your answer. As you know I have no problem with the use of the laser on bone. My only problem is being able to see the bone and root so the proper contouring takes place..
The second case shown does not have excessive bone. The key to the picture is that when one crosses the line angles correcting osseous defects or crown lengthening they can only trough the bone when doing closed flap CL.
The pictures allow us to now see what the underlying tissue looks like both bone and root surface.
The 4 th case shows the root surface and all the problems associated with the furcation. Again visabilty is critical to correct all the problems on the root.
I LOVE lasers when used within realm of BIOLOGY!
Thanks,
Danny(Edited by Dan Melker at 10:58 am on June 14, 2004)
N8RVSpectatorI wanted to jump in here for a couple of reasons. One, because, like Bill, I stepped on some toes when I first posted and can feel his pain.
Also, because I think I represent an entire segment of dentists out there who can easily fall into Bill’s category of “morons”. I know I’ve placed my share of restorations that have violated biologic width principles and some have come back to haunt me. Most haven’t. We’ve all seen what I call “amazing dentistry” — the crowns that fit like socks on a rooster but have no perio or decay. Fortunately, some peoples’ systems can tolerate some incredible insults. Most can’t.
Twenty-plus years ago in dental school, the term “biologic width” wasn’t discussed at any great length. I can’t even recall its being mentioned, and I don’t think that’s because I slept through the lecture.
Consequently, many of us start our careers with only the rudiments from school and are thrown into the profession with little knowledge of how to perform complicated dentistry successfully.
Maybe I’m deluding myself, but I think I represent an entire segment of garden variety dentists who do generally nice work on a regular basis. We’re not into gnathology, TMD treatments or perio surgery. Total occlusal reconstruction we simply don’t do. But we do very nice restorations and do them every day. We don’t contribute articles to journals or travel to seminars to teach others.
We coach little league or soccer, teach Sunday School and read novels for relaxation rather than JADA. Our patients generally like us and trust us to take care of them as we would our own families. We’re reluctant to buy the latest and greatest gizmos and use our patients as guinea pigs.
We start our practices, raise our families and struggle to squeeze mandatory CE into our schedules. In the blink of an eye, two decades have passed and we’re still drillin’, fillin’ and billin’. It works. It pays the bills. It gives me time to raise my family and have hobbies, which is why I chose the profession in the first place.
I admit that with some shame, because I thought I’d always be on the cutting edge of dentistry and would never allow myself to turn into one of those “old coots” who still practices how he was taught eons ago.
>sigh<
Anyway, I’m playing catch-up big time. Now that my kids are gone, it’s time to learn new techniques and new treatment modalities. The concept of biologic width and how to fine tune what I already do right is a great adjunct to my personal “continuing education”.
As was mentioned, in the real world, patients will often accept a crown, hesitate if it involves RCT as well and will probably opt for extraction if you mention the cost of crown lengthening.
I, for one, was anxious to start closed crown lengthening procedures with the information garnered from the laser sales pitches. After digesting the great posts here from Glenn, Danny, Ron and others, I’ve come to the conclusion that I need to seriously consider open procedures rather than closed.
I have a LOT of work ahead of me. Not unlike dental school, it’s a do-it-yourself project. I don’t even know where to incise for such a procedure; I’m sure even that has changed over the years. But I’ll learn. I’ll ask questions, try some things and, like others before me, fail occasionally. But I’ll succeed more often than fail, and my patients will be be beneficiaries of my technical improvements, even though they’ll probably be unaware.
I’m a good dentist — not great, just good. And that’s OK. I may even be a moron, and I won’t argue that. Heck, it’s much better than some other things I’ve been called. However, sometimes we morons do things because we haven’t taken the time to learn how to do things better than we were taught.
Bill, here’s a challenge for you: Take a moron to lunch. If you see somebody continually abusing biologic principles, maybe a friendly conversation would open his eyes to a concept that he never learned. Just a thought…
— Don
Dan MelkerSpectatorDon,
I have started posting Biologic cases so wee all can see what is really there. This is a great forum if we all have the same concept-Understand Biology and use the tools within its scope!
Laser or Handpiece-follow Biologic principles
Thanks
Danny
N8RVSpectatorYes, Danny, you’ve made a believer of me. Before your challenge to closed CL, I thought it was just an easy procedure that could be whipped off just prior to completing a post & core and crown prep — and sometimes can, but not without completely visualizing the width of bone available and the resulting contour of bone after the procedure. Without your input, I’d have tripped along merrily, probably making circumferential ruts in bone around every CL tooth.
I’ve seen you go from being somewhat adversarial toward lasers for CL to being accepting — so long as biologic principles are followed. I commend you for being open to new paradigms of treatment ( I just HAD to use that word!)
I’m looking forward to learning more from all of you.
(I also apologize for the length of my last post. I had no idea I was so long-winded! Oops.)
— Don
dkimmelSpectatorDanny, Lets get through a couple things first.
1. As opened cases all four of your cases could be done with a laser. It’s just a differnt tool and if you follow the same technique the end results would be the same.
2.Of the four cases you posted only one would have been done as a closed procdure by most laser dentist. That is case #2. The other cases are far too difficult and I can say I have never seen somone try to do these types of cases as a closed procedure. Now I will give you that it is far easier to tell that these cases are to difficult to do closed as we are seeing them opened. Though as you become more aware of what the under lining bone looks like you can tell predict its appearence without flapping the area.
The majority of laser cases are of two types.
1. Is an isolated area of BLW invasion. Like the DO alloy that is sitting on the bone or a fractured premolar where the lingual is ok but the facial is at the creatl bone.
2. The anterior GV or anterior osseous recontour. Sort of like you case #2. But more like your favorite Biolase ad.
That out of the way lets go to Case #2-bone touching cej related to APE.
The second case shown does not have excessive bone. The key to the picture is that when one crosses the line angles correcting osseous defects or crown lengthening they can only trough the bone when doing closed flap CL.When you place the laser tip within the sulcus you don’t just move it within the confines sulcus. You work it under the tissue as in a blunt disection. Once you have a release you start to remove the osseous structure. Unless you have a very thick bone on the buccal or lingual it is not difficult. You just need to comfirm this with a periodontal probe. The probe will quickly tell you if you have troughed the area. It is agreed troughing is not good. The interproximall areas are the tough part. The case you picked is real tough because of the shape of the mesial and distal tooth structure. Using tthe periodontal probe would quickly tell you there is a problem. In this case you would place the tip of the laser only the long axis of the tooth at the distal line angle. Because of the acuteness of this angle you would have to work the laser toward the distal bringing it up so as not to flatten out the interproximal bone. You would need to continue this until the proper osseous reduction occured and it felt smoot to the perioprobe. You would need to do this on the distal lingual. Then repeat as needed on the mesial. Cake walk!
David
.
Dan MelkerSpectatordAVE IS SETTING ME UP. No one, not even me is that good. Dave you are in a critical esthetic zone wanting to be perfect. No one no one, yes I am repeating myself is that good. Periodontal pockets are nothing more than discrepancies between bone and soft tissue!. If you are off just alittle in your Closed CL procedure-guess what-possible creation of periodontal pocket.
Take a look at the bone in case #2. The bone has a great deal of irregularities in thickness in a buccal lingual direction. No one no one is that good.
I am trying to get across a point- do it right if you are going to do something. Do not do what is easy or in the eyes of some less painful. Do a procedure that is the best that can be done!
If you want to do CL- learn how to do a perfect flap with perfect suturing tech as quickly as possible to decrease discomfort for the patient. Then do all the osseous you want with a LASER. Just see what you are doing.
There is a big misconception about discomfort and Perio surgery. Do a proper flap-with the proper blood supply as atraumatically as possible, quickly so the tissue does not dry out etc. and the patients discomfort is far less!
Enough said. As you have helped this board so much doing a closed flap procedure then opening it up do another one like case #2 where you feel it is indicated and I will open it up for you and take pictures of what uyou did free of charge!
Danny
dkimmelSpectatorNow who is being set up??
You have just said:
If you want to do CL- learn how to do a perfect flap with perfect suturing tech as quickly as possible to decrease discomfort for the patient. Then do all the osseous you want with a LASER. Just see what you are doing.
There is a big misconception about discomfort and Perio surgery. Do a proper flap-with the proper blood supply as atraumatically as possible, quickly so the tissue does not dry out etc. and the patients discomfort is far less!So start typing. I’ll be easy on you. Tell me about how to do a perfect flap on case #2!!!! That is sticking to sound biology
Got you!!
David
kellyjblodgettdmdSpectatorI’m looking forward to the response. Could you add some pictures or diagrams to illustrate your flap design in such a case? Thanks, Dan.
Kelly
Dan MelkerSpectatorKelly,
I usually design my flaps so I can always suture to periosteum. When one sutures to periosteum the flap can be placed any where the surgeon wants. This is extremely critical because it means that no connective tissue has to be removed to prevent the flap being to high on the tooth. That is the major reason for GV.’s. The problem with GV.’s is they remove good connective tissue.
In the above cases I start with a full thickness flap to get over the exostosis and split the tissue. If you look to see where the flap is sutured, it is in the mucosa where I picked up periosteum. Notice the flap lays just over the bone and will not move. I have not packed a case with perio pack in 20 yrs.
I do not remove connective when I do flaps and therefore always have an abundance of connective tissue.
Thanks,
Danny
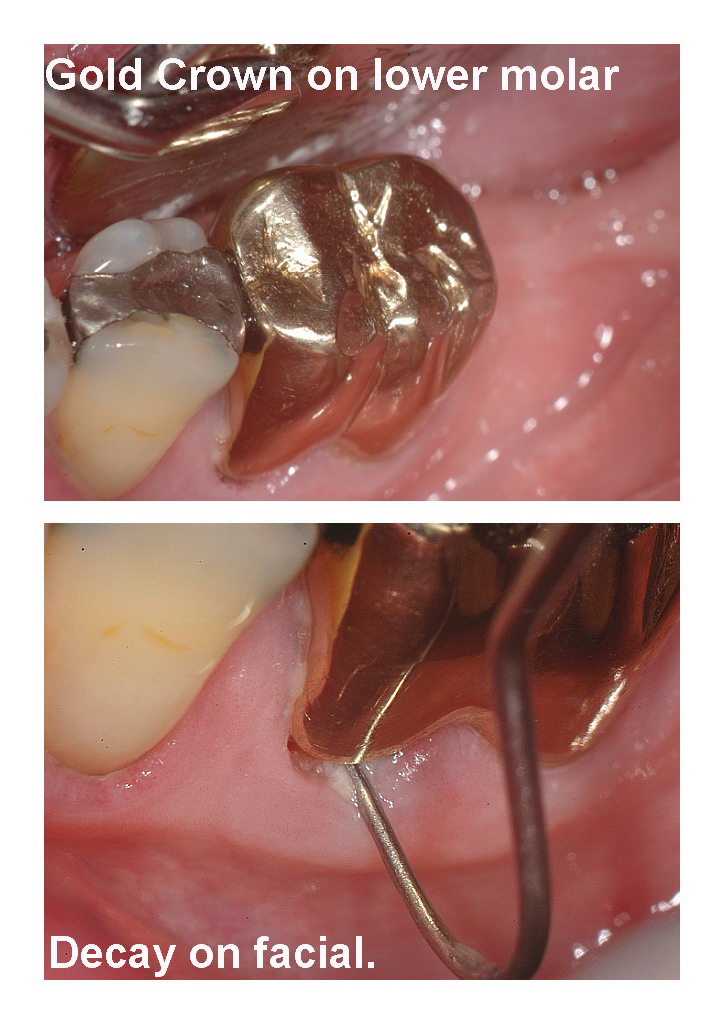
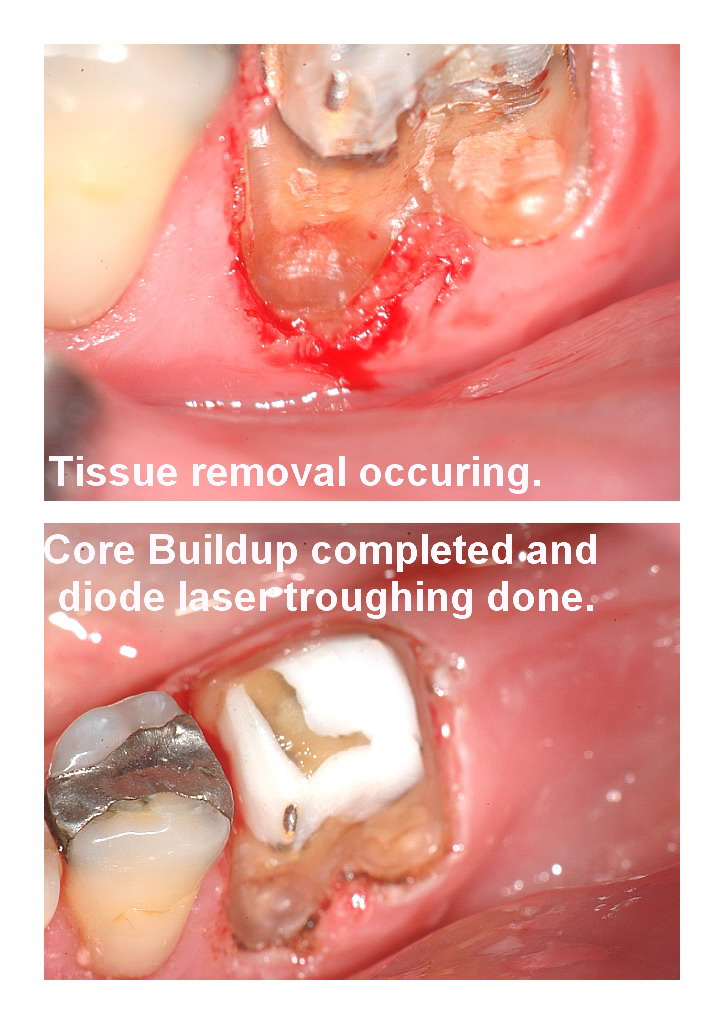
Glenn van AsSpectatorHere is a case I did today. It was done Closed flap CL.
THere was decay under the gold crown which needed removal and there was alot of decay under the buccal. I used the erbium for soft tissue and bone (1mm or so) and ran out of time before I could get the impression.
I will follow the case up.
I like the clarity of these pics shot with the new camera setup and with a little time I figure the pics of mine will be improved.
Hope you like it and I didnt get a chance to take a pic of the provisional crown in place.
Take care and cya in a week when I am back from Salt Lake City………cya
Glenn





lookin4tSpectatorGlenn,
Do you have 2mm or more of keratinized/attached tissue on the mesial root? Hard to tell real well, but that is one limitation of doing CL without a flap.
A furcation area is one area I really would prefer it to be an open technique.
Can you explain to a non-laser user what the main advantage of a closed technique in this situation?
(Edited by lookin4t at 12:46 am on June 28, 2004)
Glenn van AsSpectatorHi Hack…….thanks for your interest in the case. You know what these are the tough cases when they occur because honestly you know there is decay under the crown but really you have no idea how extensive it is.
I was faced with a tough decision………flap the case and perhaps run the risk of opening up the furcation on a patient who has previously gotten decay under a gold margin and doesnt have the best OH
I could have done Dannys Root reshaping but the decay was quite deep into the tooth so that again presents problems because there is pulpal blushing as it is due to the proximity of the decay.
I chose to place a temporary after really removing tissue and a very little amount of bone strictly on the MB of the tooth.
It wasnt interproximal and I used a curette afterwards to try and smooth out any ledges.
I will follow this case so that you may see how the healing occurs. I have done this 5 times on cases just like this.
One hasnt healed (temp crown broke off in addition and tooth was extracted).
Other 4 have healed…….
Hack, you are always courteous to me. If you had a GP who referred to you, would you ask him to place a temp in this case and refer to you for osseous , how would you handle this case.
I will show you the results as they come in.
Glenn
lookin4tSpectatorI would ask them to remove the decay as best they can, temporize it….and I would get anything left behind and add to the temp. Yeah, I still remember how

I’m more comfy flapping it near a furcation to see what I have to work with.
drcamSpectatorAnyone able to direct me to Danny’s pictures for his case presentation???
TIA Cam
-
AuthorPosts
