Forums › Other Topics › Consultation › Consult?
- This topic is empty.
-
AuthorPosts
-
AnonymousGuestHi All,
Can all you great dentists give me a little feedback on the following?
About a year ago my chiropractor starts coming to me . Has a history of long time ortho (last 5 years although all hardware off when I see him the 1st time), uncontrolled diabetes and no previous periodontal care- just ‘routine cleanings’.
Referred to periodontist and ortodontist. Ortho and perio come up with a plan to extrude upper anteriors to ‘grow bone’ and the extract and place bridge or implants. Perio also wants to do osseous surgery 4,12, 14. Ortho also wants to realign upper anteriors to get rid of traumatic occlusion- this would be the 3rd go around for braces. Patient alarmed at the บ,000 cost without my restorative plan and no certain outcome ( has 2 daughters in college so $ a concern).I told patient not to do any surgery w/o getting diabetes under control.
Patient went to endocrinologist and is now controlled (1 year later) and would like alternatives to previous treatment plans.
Charting 02/04/03
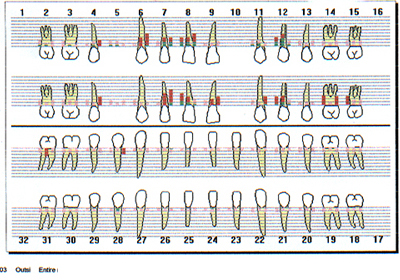
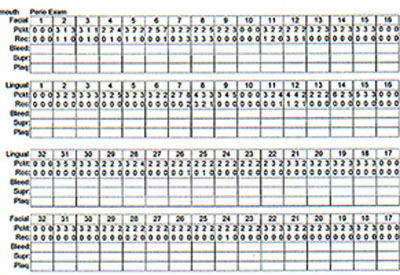

[img]https://www.laserdentistryforum.com/attachments/upload/rccuspidu.JPG[/img]
[img]https://www.laserdentistryforum.com/attachments/upload/rcltbw.JPG[/img]
[img]https://www.laserdentistryforum.com/attachments/upload/rcrtbw.JPG[/img]
[img]https://www.laserdentistryforum.com/attachments/upload/rcrtbw2.JPG[/img]
[img]https://www.laserdentistryforum.com/attachments/upload/rcmaxant.JPG[/img]
I’m reasonably sure we can get the 4’s , 5’s and 6’s back to where they belong w/ scaling & rootplaning and the diode laser.
What would you do with 6-12 and 14’s bone loss?
Restorative options?Thanks for any insite you might have,
Robert Gregg DDSSpectatorHi Ron,
Do you REALLY want to know what I would do??:biggrin:
Seriously, what does the patient want to do? What does he want to invest in time and treatment effort and cost?
My orientation would be to try and save each and every tooth by doing endo, LANAP perio, occlusal adjustment, splint therapy and then seeing how he heals…….for the next 2 years! Yes, even the lateral and #14. Touch up as required any perio pockets that partially heal.
But I think you’ll need a variable pulsed Nd:YAG for those deep pockets and considering his diabetic tissues! :cheesy: Much better control over tissue response of the variety of tissue challenges in variable pocket depth and disease overlap.
I wouldn’t subject him to any more ortho though.
Bob
AnonymousGuestJust an update.
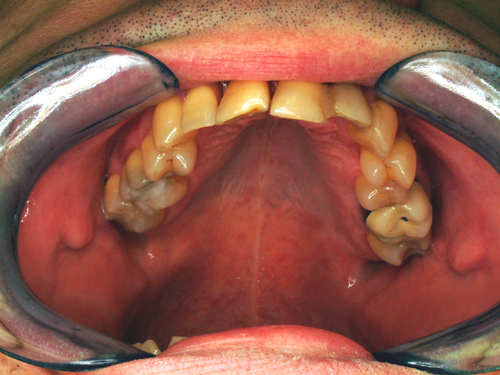
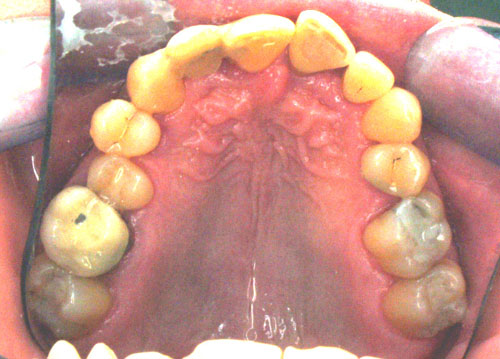
Patient finally decided to try and save teeth but would not see periodontist for surgery or ortho for extrusions . Patient also wouldn’t wear braces for the 3rd time. 14 probed 10+ mm.
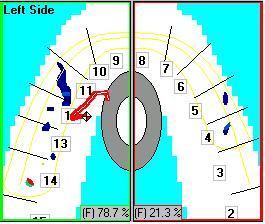
1 week post op LPT of left side TX. Time for some occlusal adjustment. Found it very interesting the correlation between which teeth were in hyperocclusion and where the bone loss was most severe.
[img]https://www.laserdentistryforum.com/attachments/upload/Image010.JPG[/img]
TEK Scan movie before adjustment
TEK Scan w/ adjustment. Further adjustment was done right side after this movie.
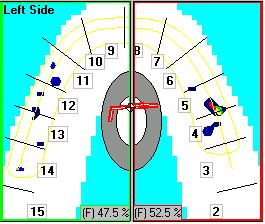
After adjustment patient sat up and said “WOW, that’s the first time I’ve been able to bite on both sides since I got braces off”.
Made my day!
We’ll see if we can get some new attachment and bone back.
Robert Gregg DDSSpectatorRon,
Excellent case presentation and initial results. Based on the history, I would fully expect regeneration/new attachment.
Remember, “The depth of the bone defect is directly proportional to the amount of occlusal trauma”.
and, “If there is a bone defect, there is a traumatic force that directly correlates to that defect–and it is proportional to the amount and severity of the defect–so the clinican must find the trauma as it is often masked by mobility.”
The use of the Tek Scan is an excellent way to find the hidden trauma! Since I updated my software from 2.0 to 4.0, I am using it much more these days.
Great stuff Ron!
Bob
AnonymousGuestMoved here from Off Topic.
drnewittSpectatorBob , how did you go about finding the hidden trauma before you got your hands on the Tek Scan? Did you do full cast articulation?
Robert Gregg DDSSpectatorQUOTEQuote: from drnewitt on 5:25 pm on June 4, 2004
Bob , how did you go about finding the hidden trauma before you got your hands on the Tek Scan? Did you do full cast articulation?Paul–
1. The defects revealed by the x-rays indicates there is OT–every single time.
2. Depth of the defect is proportionate to the amount and severity of OT–every single time.
3. Laser ANAP protocol has a means by which to help assess the direction of tooth deflection into the defect.
4. Green articulating wax for the 3-D visualization of the impact. Often better than Tek-Scan.
Casr models don’t reveal very much info.
Bob
lookin4tSpectatorbob,
I had one case today and 2 other cases in the last 4 months with furcal bone loss that had nothing to do with trauma. When you say every time do you allow for exceptions?
You see, these cases were sporting cemento-enamel projections. They were the only areas in the jaw with periodontal disease.
I think occlusion can be important, but it isn’t in play every single time. Would you agree given the examples I stated?
The reason I ask is I sat through a Bill Dickerson lecture. The highlights included him attributing 80% of endo to malocclusion/trauma and stating that 100% of exostoses and tori are related to occlusion. The latter statement is not reflected in the lit. It seems that some people are predisposed to bone formation genetically be it from normal or abnormal forces. Bone can either do nothing, resorb, or increase formation as a general rule. Some of these people will get exostoses in the presence or absence of occlusal trauma or malocclusion or whatever he was saying. In short, for a guy that likes to be on the edge, get in your face a bit, and criticize CR from a scientific standpoint, he somehow expects you to swallow it all without question.
And you’re no Bill Dickerson Senator…I hope

Robert Gregg DDSSpectatorHack,
Yes we allow for exceptions. I had a furca case last week with an enamel projection–and took some photos of it.
But there is a much stronger correlation of pocket depth to OT than I ever appreciated until about 8 years ago. So while OT may not be in play “every single time”, for training and for practical reasons that what we harp on.
When a doctor says that his/her results are not as dramatic as what Del and I show, I know it is one of two things (or both):
1. Not enough laser energy is being used.
2. The OT is not being appreciated and adjusted.It is just that simple.
Our dental school training and the literature (as you point out) do not support this association. But after too many failures over too many years of not looking 4 it , and now that I am, I cannot get over how often OT is involved in some way with inflammatory PD and to the extent that it is involved once identified.
It’s like the MB2 canal in an upper molar root canal. People didn’t start having MB2 canals until I was out of school for 10 years. There was an “instance evolutionary leap in human being” from 3 to 4 canals in upper 1st molars! And then they started presenting in my office (right after it was widely published) and I started looking for them. Then I started seeing them in the majority of my RCT upper 1st molars.
So just just like for MB2 canals, OT must be ruled out as a causative etiology first and not just looked at in retrospect when the pocket persists or breaks down–or the RCT fails.
When we first discussed this with Prof Yukna prior to starting the human histo, we had to hold our breath. Then he said that while the literature doesn’t support it, from his clinical experience he gets better results when he does it.
Recently, and at the last Bootcamp training couse where Yukna participated (what a great weekend that was) Ray said that the pendulum for doing OA for grafts and PD is swinging back towards doing it.
Good question.
Bob
lookin4tSpectatorbob, didya get my email Re:October?
I’ll need some travel info.
Thanks for the review. Occlusion seems to shift in and out of focus every 15 or 20 years….one thing is for certain with GTR, it’s harder to grow it around a moving target, adjusting the occlusion is one way to address it.
I love the old school wax by the way.
Can you post a pic or describe what appliance you use as I thought you discussed a splint of some kind?
Robert Gregg DDSSpectatorQUOTEQuote: from lookin4t on 1:41 am on July 30, 2004
bob, didya get my email Re:October?I’ll need some travel info.
Thanks for the review. Occlusion seems to shift in and out of focus every 15 or 20 years….one thing is for certain with GTR, it’s harder to grow it around a moving target, adjusting the occlusion is one way to address it.
I love the old school wax by the way.
Can you post a pic or describe what appliance you use as I thought you discussed a splint of some kind?
Got your email. I think that’s fine. I forwarded the date on to Dr. McCarthy for FYI and processing. He said it is a go. But give him a call at 888-49-LASER to remind him.
We use all sorts of non-fixed and fixed stabilization:
1. Lower Panke occlusal guard with anterior ramp.
2. Ribbond
3. Composite interproximally on loose anteriors
4. Wire splinting on some casesSee you in October………Bob
-
AuthorPosts
