Forums › Erbium Lasers › General Erbium Discussion › er,cr:YSGG
- This topic is empty.
-
AuthorPosts
-
AnonymousGuestHi all,
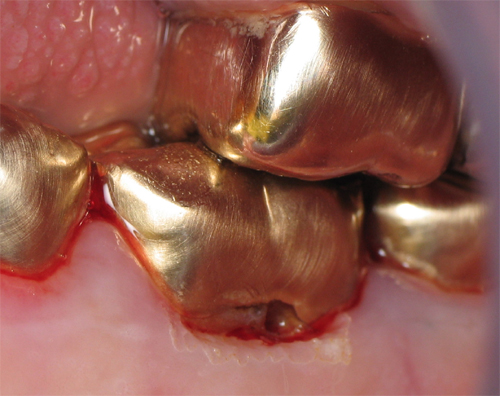
Today had a middle aged gentleman w cervical decay buccal and subgingival to crown on #19. Patient didn’t want new crown at this time after explaining to him that the depth of the decay may lead to endo.preop

Decay/ beginning gingival recontour/removal
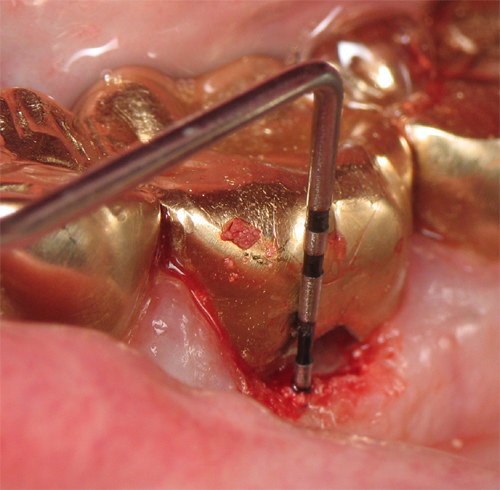
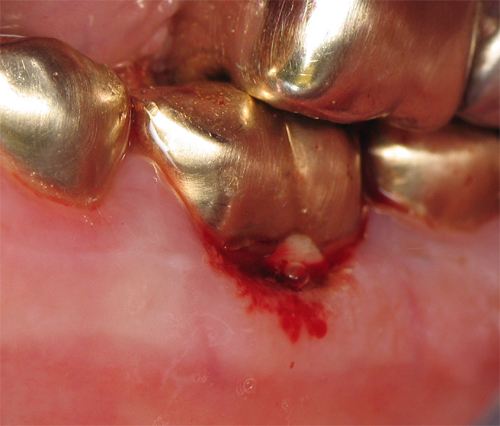
More recontouring of gingiva

Probe
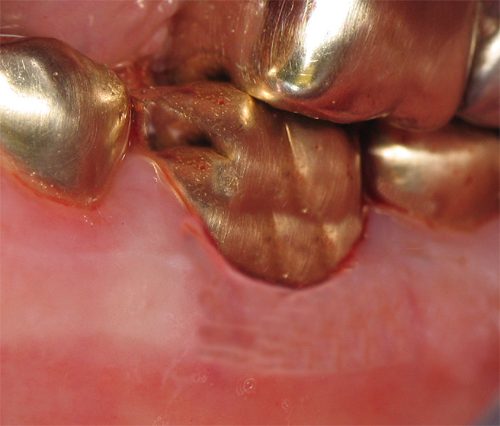
Post op
EMLA (no local anesthetic),4mm tip er,cr:YSGG
gingival recontouring/removal .75w 11/7
Caries removal – 1.25W 60/30 , spoons
Bone Removal 1.0w 40/30 (yes I did it closed because it was minor)
Near exposure lined w/ ‘aussie wonder mix’
Restored w/ Fugi IX
Probably would have got a nicer recontour w/ the nd:YAG but it was in the next room setup for the next patient.
Hopefully we’ve avoided endo and I’ll remember to take a picture at recall
SwpmnSpectatorInteresting case and demonstration using an erbium laser around what is obviously a high noble metal. Did you observe any “sparking” or “flashback” if you inadvertedly irradiated the gold crown? Due to our elderly patient pool in Florida, we have done many similar cases using both the Er,Cr:YSGG and the Er:YAG wavelengths. I observe similar results trying to obtaining a clean recontour and also difficulty controlling hemorrhage with the erbiums.
What is the advantage of Fuji 9? Is it primarily adhesion, fluoride release and use of a no-Hg restorative? I’m still kind of from the old f*rt school on these Class V repair jobs and this is our primary use of dental amalgam. Is Fuji 9 triturated and injected into the defect or do you hand mix and pack? Then you allow the material to set and contour with bur?
Regarding your mention of the free-running, variable-pulsed digital Nd:YAG. Are you finding in cases such as this you would be able to recontour the gingiva and obtain hemostasis without the use of local anesthetic? I have a handful of early cases where we’ve done this with our 810nm diode and am interested in comparisons and observations from others.
Al
AnonymousGuestQuote: from Swpmn on 7:29 pm on Oct. 8, 2003 Did you observe any “sparking” or “flashback” if you inadvertedly irradiated the gold crown?
No flash or spark but I was being extra careful
What is the advantage of Fuji 9? Is it primarily adhesion, fluoride release and use of a no-Hg restorative? Is Fuji 9 triturated and injected into the defect or do you hand mix and pack? Then you allow the material to set and contour with bur?
Al, this stuff is great. Tirturated and then injected. About 3 minute total set. Can be finished w/ bur under water spray but usually after about 2 minutes set time you can ‘carve ‘ it w/ your explorer to remove any extra. I love the fluoride release and adhesion. I’m not an anti amalgam guy , I just am real pleased w/ this in areas where hygiene is less than ideal (as you could see above). I am also doing more and more of Graeme’s co-cure sandwich technique w/ the Fugi IX in the box and then overlayed Fugi LC and composite. Starting to see these come back at 1 year in high caries rate individuals and there is no new decay in these areas (thanks Graeme!) I also like GC Ketac Silver as a temp material for fractured cusps. More times than not it stays until the patient comes back for the crown prep and you have fluoride release in the mean time.
Regarding your mention of the free-running, variable-pulsed digital Nd:YAG. Are you finding in cases such as this you would be able to recontour the gingiva and obtain hemostasis without the use of local anesthetic?
Al
Yes, by widening the pulse width I see to get better hemostasis than I did with the diode.Now if you have any tips for keeping saliva bubbles out of the pictures….
ASISpectatorHi Ron,
Yeah, that Fuji IX has great fluoride release. You can be certain as the bubble shows in your photo….
Grin.
Andrew
AnonymousGuestWhat bubble?

😉
2thlaserSpectatorGee, I thought I saw a bubble!! Hmmm…….
Ron, great stuff, and excellent use of GI. I use the co cure technique as well, with wonderful results. Have you seen Doug Youngs, stuff on Carries Risk Assesment, and the protocols involved with these high risk, no hygiene type of patients?
Mark
Tom HaneySpectatorAl,
Regarding your questions about seeing any sparking or flash with the erbiums: We have tested the DELight at highest average powers on both gold and porcelain crowns. I have never seen any effect yet. If there is no absorption in the material, there is no effect. I don’t know about all of the metals, but I would be interested to hear if anyone has seen any sparking or flashing with anything else.
Tom Haney
VP Hoya ConBio
AnonymousGuestQUOTEQuote: from 2thlaser on 12:21 am on Oct. 9, 2003
Have you seen Doug Youngs, stuff on Carries Risk Assesment, and the protocols involved with these high risk, no hygiene type of patients?
MarkMark, I heard Doug a few years back as well as someone else whose name escapes me now , a few years before that. Based on Doug’s and this other guys info we developed a ‘Caries Reduction Protocol ‘ for high caries rate individuals. It basically involves taking away the bacterias hiding places (sealants, oral hygiene instruction, GI restorations or combo restorations) , decreasing the amount of bacteria (chlorhexidine rinse at home after restorations done, now soon as we can get some betadine- which seems everyone has backordered we’ll do inoffice rinse q3mths, and reminerilization (Act fluoride and gum w/ recaldent). The people we get to do it (follow thru) really see a decrease in caries rate. We also occasionally use the Ivoclar kit for salivary flow and bacteria counts.
Thanks for the nice comments although I did expect some comments on the Cubs?
2thlaserSpectatorHOLY COW!!….BTW, make sure you also substitute xylitol based gums. The Trident White with Recaldent is ok, but not xylitol based. Xylitol should be the first ingredient…I found it so far at Starbucks….Trident Original has xylitol, but also sorbitol.
Mark
ericbornsteinSpectatorRon:
Very nice stuff.
Huge service to patient, as you do not need to uncouple the entire area and start from scratch with your technique.
Eric Bornstein DMD
AnonymousGuestQUOTEQuote: from 2thlaser on 9:39 am on Oct. 9, 2003
HOLY COW!!….BTW, make sure you also substitute xylitol based gums. The Trident White with Recaldent is ok, but not xylitol based. Xylitol should be the first ingredient…I found it so far at Starbucks….Trident Original has xylitol, but also sorbitol.
MarkMark, we’ve also found it in Xylifresh gum (most often at health food stores) and at one time Extra Bubble Gum and Cinammon flavor had xylitol. We have trended to the recaldent just because its so much easier to find in this area. We also recommend the oral B 3DExcel toothbrush (adult) or some of the spin brushes for kids.
Here’s the actual form we give patients to put on their refrigerator-
CARIES (DECAY) REDUCTION PROTOCOL
In past years, dentists have concentrated their treatment on restoring decayed teeth. This treatment usually consisted of repairing teeth with silver or white materials. Preventive care consisted of the toothbrush, floss, professional cleaning, and fluoride.
Recent advancement has allowed researchers to determine that decay is actually an infection caused by the bacteria Strep. Mutans. This bacteria uses carbohydrates (sugars) to produce acid. The acid in turn works on the tooth surface to leach out the minerals, causing the tooth to soften and produce a cavity (hole) in the tooth.
Since we now know that decay is caused by an infection common sense tells us our focus should turn to eliminating the infection rather than filling holes. Using the following in addition to professional cleaning, fluoride, and routine home care can do this.
1. Bacteriologic Testing – Similar to what your physician does when he tests you for strep throat. A sample of bacteria is taken from the tongue and incubated and then analyzed for the amount of decay causing bacteria.
2. Sealants – The bacteria that cause the dental decay infection colonized (chose to live in) the deep grooves on posterior teeth. By “sealing” off these areas we take away one area that the bacteria can live and produce its acid.
3 .Restoration of previously decayed teeth. Again eliminating a living area for the bacteria.
4 .Prescription Mouth Rinse – Peridex or Perioguard mouth rinse may be prescribed to be used to help reduce the amount of bacteria present.
5. Home Fluoride Rinse – to be used before bedtime to help remineralize teeth and make them more resistant to decay. (Act Fluoride Rinse)
6. Gum – Xylifresh or Recaldent gum contains a chemical that affects the decay causing bacteria to be unable to produce as much acid.
One final factor is very important in preventing decay and that is eating patterns. As one eats, the decay causing bacteria are supplied with a source of energy to produce acid that stays in the mouth for approximately twenty minutes and begins to leach minerals out of teeth. Your saliva then comes along and dilutes the acid and begins to remineralize the teeth. Now if food and drink are being supplied to the bacteria continually (not just at mealtime) the saliva never gets a chance to remineralize the teeth and the decay process accelerates. This leads us to recommend limiting eating to mealtime so that teeth are not continually bathed in acid.
Based on our findings we recommend the following for _______________________________________.
1. Brushing ___________ times per day.
2. Flossing ___________ times per day.
3. Sealants on tooth#______________.
4. Restoration of tooth#____________.
5. Act Fluoride rinse morning and nighttime (Nothing by mouth for 30 min after)
6. Iodine rinse in office at 3 month interval.
7. Bacteriological Testing at __________ month intervals to assure reduction of decay causing bacteria.
8. Gum – Chewing Recaldent Gum ________times per day. (Trident Kids with Recaldent and or Xylitol containing gum).
Midwest Center for Laser Dentistry, P.L.L.C.
Ronald W. Schalter, D.D.S.
808 N. Maple Grove Avenue, Hudson, MI 49247
517-448-7130
<a href="http://www.laserdentist4u.comYou’re” target=”_blank”>http://www.laserdentist4u.com[/color]
You’re free to use this unless you’re in Hillsdale, Lenawee County Michigan, or Fulton County Ohio otherwise you have to make up your own version 😉
Glenn van AsSpectatorRon , absolutely outstanding and thanks as I have copied it for my office.
Great stuff and I mean that………wonderful post.
Glenn
-
AuthorPosts
