Forums › Laser Resources › Laser Physics Related Literature › Hydrokinetics Article
- This topic is empty.
-
AuthorPosts
-
ericbornsteinSpectatorRay:
Let me re-state this again.
1) Newton’s third law of Motion:
Newton states that whenever one object exerts a force on a second object, the second object exerts an equal and opposite force on the first. In other words, to every action there is always opposed an equal reaction.
If you were to push on your computer screen with your fingers, the computer screen is also pushing on you. That is why your fingers will bend.
Neither force exists without the other, and forces come in pairs. The action and reaction pair of forces makes up one interaction between two things.
Now, If I were to ask Mike Tyson to punch a piece of tissue paper that I put in front of him, Tyson,s fist (reguardless of how pissed off he was) could only exert as much force on the tissue paper, as the tissue paper could exert on him.
Even if I were to buy the arguement (which I do not) that the spray nozzle was sophisticated enough to produce certain shapes and/or opacities of water droplets to cause “ignition” of the water in “certain areas of the droplets” upon the incidence of erbium energy, where in the world is the necessary remaining water mass, to produce a force large enough to propell the remaining water, at a direct vector velocity to actually cut something as hard as enamel.
Come on Ray, you sound like a guy that understands rudimentary physics. Newton would need a Valium to buy this argument.
Second:
As to your Relativity point. What is the point? Again, as I previously stated.
If incident erbium energy (infrared light) strikes a water droplet in front of the beam, and the reaction (vaporization, hydokinetics, whatever) begins; long before even 1% of the reaction causing the hydrokinetics takes place, the rest of the erbium photons that did not interact with the water must have already hit the tooth and begun the thermal-mechanical ablative reaction that we all know. To state any different logic than this (because remember light travels at 300,000 kilometers/sec) is to say that the hydrokinetics is faster than the speed of light.
Every study and crater photomicrograph I have ever seen (with all erbium lasers) clearly shows thermal-mechanical ablation of dental enamel. It is crystal clear that the Er:YSGG photons that successfully make it through the aerated water spray in front of them, strike the enamel target and start the thermal-mechanical ablation WAY WAY WAY before any “Hydrokinetic” effect could ever take place, BECAUSE of the speed of light.
Again from the web site.
How does Waterlase™ work?
•Waterlase™ uses a cool-water spray to cut teeth without generating heat. Conventional drills and lasers can overheat teeth during procedures, inducing discomfort and irreversibly damaging the soft tissue or pulp underneath.
•The Waterlase™ system uses laser-energized water to cut teeth.
•The Waterlase™ emits a laser beam that energizes a highly precise spray of air and water.
Water droplets absorb the laser energy and become laser-energized water particles that, when directed at the tooth, rapidly remove enamel, dentin and decay/caries.
Let me now write out a Valium Rx for Einstein.
Eric Bornstein DMD
Robert Gregg DDSSpectatorEric,
Excellent explainations concerning the physics in simple terms for us to understand.
I think part of the question is why the company feels it is so important that energized-water be the mechanism that they defend it so strongly in the absence of credible science or logic–and now in the presence of credible research and references that disprove it???
Eric, you posted some of the unproven energized-water claims from the company website. Here is a jpeg photo of an animation that the company had on their site at one time. It portrays the concept that they are trying to get everyone to accept. One wonders why it was removed when the website claims are the same.
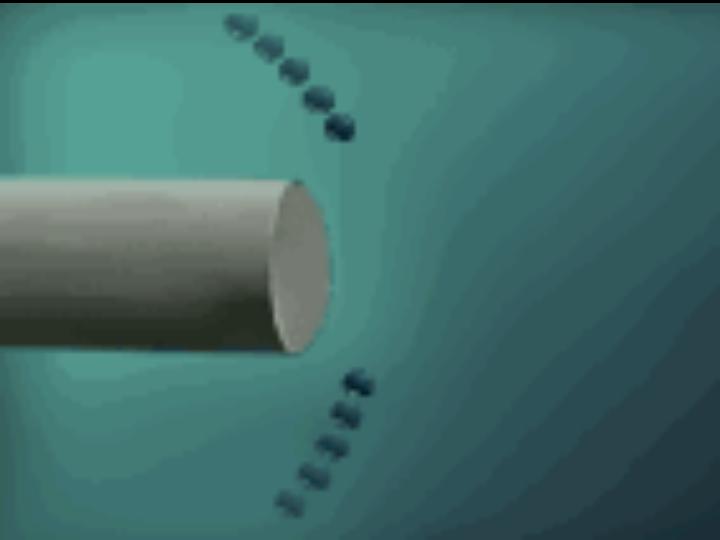
What this animation shows is the water droplets (above and below) coming into the path of the Er, Cr: YSGG photons coming down the fiber. The photons are completely absorbed into the water droplets and the droplets accelerated to the speed of light (apparently) towards the target tissue.
The company and their representatives are extremely defensive when these sorts of questions are raised.
Why?
I’m sure it’s because they are ultimately insecure about their claims and don’t want new prospects to hear a contradictory opinion. If it isn’t water doing the cutting, then it is photons. If it’s photons, then the prospects have other laser devices to take a look at. If it isn’t energized-water, then those new 1-800-DENTIST ads thye plan to run in California to the public (now on their website) aren’t accurate.
Bob
ericbornsteinSpectatorBob:
Once again, another voice of educated reason on the dental laser thread. I also have this animation stored in my computer. Photon torpedoes and warp factor 5 anyone?
Thanks,
Eric Bornstein DMD
lagunabbSpectatorDr Bornstein
looks like we are talking past each other again and I am sure we would both be taking remedial physics classes and go through Feyman notes if we had to take a test.
(1) Newton’s law only apply to bodies with mass. It appears to me you are raising issues about water-laser interaction. If you make the assumption that the water droplet explodes from the center of the mass (the droplet’s mass), then you would be right in questioning whether there will remain anything usable afterwards. That’s a big assumption. To answer that, you have to estimate how far the photons have to penetrate a water droplet before it explodes. It would depend on droplet size or if we are dealing with a film, film thickness. If rapid water vaporization happens close to the surface of the droplet (given a big enough size), as I think it does, then there would be enough mass left over to form a high velocity shock.
(2) I don’t believe anyone disputes that photons do get through the mist or films since the amount of water contained in the space in front of the laser has to be volumetrically small compared to air volume even at the highest water setting. The question is whether those photons are useful for vaporization ablation, Fried’s latest results says not even close to the ablation you can get with interaction water film+laser (at settings close to actual clinical practice).
(3) Based upon postings in DT, you appear to discredit all studies published (refereed or not) when a Biolase researcher is involved or if a study supports Biolase clinical claims (Biolase supported or not) such as the two Japanese bovine bone experiments that Ron Schalter posted. I am starting to go through some of those papers in their entirety. Since the argument in favor of “ablation mechanism has to be enamel vaporization” and one of the effects has to be tooth heating (second law), then the following experimental study (under the auspices of Biolase) has to be flawed. Please read the article and educate us as to why in your view, it is flawed:
http://www.etechadvisors.com/PDF/Pupal_temp_YSGG.PDF
username = dentaltown
password = member(I am trying to limit access to people involved in the science discussion because of copyright)
(Edited by lagunabb at 8:36 am on Sep. 18, 2003)
lagunabbSpectatorBob,
I remember seeing that animation on the Biolase web site. They must have taken it off because of the anti-HK controversy. Looks like they really dumbed it down to get an idea across. I agree the animation is vastly lacking in science but then it is probably better than showing maxwell’s equation from the marketing perspective.
AnonymousGuestQUOTEQuote: from Robert Gregg DDS on 10:34 am on Sep. 18, 2003
If it isn’t energized-water, then those new 1-800-DENTIST ads thye plan to run in California to the public (now on their website) aren’t accurate.Bob
Gee,
I wonder if 1800dentist will refer to my office since I have a Waterlase but don’t pay for their services? and why would a dentist need 1800dentist if they have a Waterlase?Maybe 1800dentist/Biolase should change the video to say they’ll give a referral to a 1800dentist that has a Waterlase instead of a Waterlase dentist.
p.s. at least the consumer online contact form says ‘free referral to a qualified Waterlase/1-800-DENTIST’
lagunabbSpectatorBob,
when and where did Biolase ever make or made the claim below?
“The photons are completely absorbed into the water droplets and the droplets accelerated to the speed of light (apparently) towards the target tissue.”
It’s one of those statements that make me question your knowledge of physics and/or your credibilty.
(Edited by lagunabb at 9:49 am on Sep. 18, 2003)
ericbornsteinSpectatorRay:
Let us take your points one at a time:
You posted:
(1) Newton’s law only apply to bodies with mass. It appears to me you are raising issues about water-laser interaction. If you make the assumption that the water droplet explodes from the center of the mass (the droplet’s mass), then you would be right in questioning whether there will remain anything usable afterwards. That’s a big assumption. To answer that, you have to estimate how far the photons have to penetrate a water droplet before it explodes. It would depend on droplet size or if we are dealing with a film, film thickness. If rapid water vaporization happens close to the surface of the droplet (given a big enough size), as I think it does, then there would be enough mass left over to form a high velocity shock.
Response:
If we use Hale and Querry’s water absorption coefficient data, and perform the simple calculation of (1/absorption coefficient) to get the absorption length, (1) this data reveals that the optical penetration depth in water of the Er,Cr:YSGG laser is about 2um. This optical penetration depth of 2um is a 40% increase over the optical penetration depth of the Er:YAG beam per pulse, which Niemz (2) calculated at .8um. This means, that with an Er,Cr:YSGG laser, you are much more likely to explode the water droplet FROM THE CENTER OF THE MASS instead of close to the surface “front surface” of the water droplet. If we are dealing with a 1 micron water film, then you are already into the dental enamel. ANY WAY YOU SPIN THIS, there are credible issues to be answered, not just my opinion.
1 Hale, G.M., Querry, M.R. (1973): Optical constants of water in the 200-nm to 200- um wavelength region. Appl. Opt. 12, 555-563
2.Niemz, M: Laser-Tissue Interactions. Fundamentals and Applications, Berlin, Springer, pp45-80, 2002
You posted:
(2) I don’t believe anyone disputes that photons do get through the mist or films since the amount of water contained in the space in front of the laser has to be volumetrically small compared to air volume even at the highest water setting. The question is whether those photons are useful for vaporization ablation, Fried’s latest results says not even close to the ablation you can get with interaction water film+laser (at settings close to actual clinical practice).
Response:
In Erbium laser ablation of hard dental tissue, the operator is constantly attempting to keep the Ablation Front of the laser tissue interaction ahead of the Thermal Front of the laser tissue interaction. An operator must always keep in mind that with 200-400 microsecond pulse widths (all conventional Erbium dental lasers), he/she is dealing with a thermally driven mechanical (vaporization) ablation effect. Not a true photoablation or “shock wave” reaction. The heat and thermodynamics of the reaction is the most important issue. With these pulse widths, the water acts as a heat sink to keep the ablation front ahed of the thermal front. I refer you again to previous logic on the DT board.
When the Erbium water interaction is explained on a molecular level, the obvious disparity in thermal clinical data between the different erbium wavelengths becomes clearer. In a study conducted by Shori et al, describing the Quantum Mechanics of the water molecule under Erbium laser irradiation, he recently confirmed the results of a group of previous water absorption studies with erbium lasers and reported the following:
1 As water absorbs more of the incident energy of an Er:YAG laser, and the temperature of the water increases, the length and strength of the OH bond
in the water molecule changes because of the large increase in kinetic energy.2) While this important phenomenon occurs (the lengthening and weakening of the OH bonds), the absorption peak for the water molecule shifts to
wavelengths that are significantly shorter than 2.94um.3) This negative shift in the absorption peak for water, greatly diminishes effectiveness of the beam to perform further controlled thermal mechanical ablation on tissues.
Shori et al, Quantification and Modeling of the Dynamic Changes in the Absorption Coefficient of Water at 2.94um. Journal on Selected Topics in Quantum Electronics, Vol 7, No 6, Nov/Dec 2001 pp959-970
Now, if all of the above is happening as a clinician is lasing hard tissue, and the heat is building up at the ablation event horizon, the kinetic energy of the water in the unablated tissue matrix is rising substantially, and hence is changing the vibrational modes of the water molecules making the absorption coefficient for the next series of erbium pulses go way down and become less efficient.
According to the Quantum Mechanic and Thermodynamic realities of the Erbium laser energies that we are dealing with; more energy means a hotter laser tissue interface, a hotter laser tissue interface creates a faster negative shift in the absorption coefficient for water, becausee the Er,Cr:YSGG absorption coefficient for water is almost 45% deficient to the Er:YAG to begin with, it will definitely produce greater heat.
AT THESE PULSE WIDTHS, THAT IS WHY WATER SPRAYED ON THE IRRADIATION SITE IS NECESSARY
Now, I will present another study to further back up this logic, and Shori’s findings:
Erbium laser ablation: The effect of dynamic optical properties Joseph P. Cummings and Joseph T. Walsh, Jr.
Applied Physics Letters Vol 62(16) pp. 1988-1990. April 19, 1993
In the conclusion, this Cummings and Walsh study states: “ A dynamic coefficient model for absorption has been developed based on the known change in the absorption coefficient of water as a function of absorbed energy. The model explains the shorter penetration depth during ablation, and the subsequent greater overheating at the 2.79um wavelength. The assumptions strictly hold only for Q-switched ablation where thermal diffusion is not significant. Thermal diffusion will slightly mitigate the observed effects during long pulse of erbium lasers.”
In other words, this study found that with Q-switched pulse widths (ie. In the nanosecond range) that are much closer to the “shock-wave” generation model that we previously discounted for these lasers, that the water coefficient absorption change during ablation is also greater with Er:YSGG wavelengths, and hence inhibits ablation. We are again using thermal-mechanical in 140-400 microsecond range or the “long-pulse” that the study discussed.
You Posted:
(3) Based upon postings in DT, you appear to discredit all studies published (refereed or not) when a Biolase researcher is involved or if a study supports Biolase clinical claims (Biolase supported or not) such as the two Japanese bovine bone experiments that Ron Schalter posted. I am starting to go through some of those papers in their entirety. Since the argument in favor of “ablation mechanism has to be enamel vaporization” and one of the effects has to be tooth heating (second law), then the following experimental study (under the auspices of Biolase) has to be flawed. Please read the article and educate us as to why in your view, it is flawed:
I am in NO WAY SHAPE OR FORM discrediting “ALL STUDIES” when a Biolase researcher is involved. Let’s review exactly what I wrote from the DT thread.
Now since the literature has established that the Hydrokinetic Er:YSGG produces heat like every other Erbium laser, let’s review a couple of more important studies, like these three from Eversole, Rizoiu, and Levy.
“It is already known that the infrared lasers are more likely to be associated with a thermal mechanism that causes vaporization of bone structure. The absorption of laser energy (which occurs when the tissue components absorb the laser wavelength), and conversion into thermal energy results in a local deposition of heat. The dissipation of thermal energy into the surrounding tissues is a process that continues to occur even after laser exposure. This process will enlarge the damage envelope when no limiting factors occur. Many studies suggest that cooling the ablation site will reduce the amount of heat that is transferred into the surrounding tissue.”
Rizoiu I, and Levy G., The Efficiency of Bone Ablation with an Nd:YAG Laser Beam Delivered with a Cooling Spray: An In Vitro Study, Compendium, VolXV ,pp106-111, 1994.
In the above study, Rizoiu at least recognizes that Infrared Lasers on bone produce and deposit heat, even though it is an Nd:YAG.
“Hard tissue ablation occurs in a nonthermal mode with an erbium laser used in conjunction with a water spray…….. Most importantly, the critical role that the water spray plays in allowing the process to occur in a mechanical matter needs to be better understood.”
Rizoiu I., and DeShazer L., New Laser – Matter Interaction Concept to enhance Hard issue Cutting Efficiency, Laser-Tissue Interaction V, SPIE Vol. 2134A, 1994.
In this study, Rizoiu explains her new concept as essentially the uncoupling of the THERMAL from the MECHANICAL in what is really an already well explained (at this time in 1994) Thermal-Mechanical ablation process with erbium lasers. NO WHERE IN THIS STUDY DOES IT MENTION AN AERATED WATER SPRAY IN FRONT OF THE BEAM. The study was done with a traditional water spray aimed at the irradiated tooth structure from a fixed point at 45 degrees.
From where does she get the New Concept?
Even with the plethora of work published before 1994 discussing the Thermal-Mechanical ablative effect of erbium lasers, Rizoiu only references two studies in this paper. One well known paper from 1964, and one paper from 1989 discussing laser applications of erbium YAG lasers in dentistry.
The following study however is the one that really stands out.
“The wound cavities were smooth, clean and straight. At 24 hours, the wound sites for both bur and Hydrokinetic System showed a clean cut margin with a thin zone of basophilia characteristic of a thermal coagulative effect.The zone measured 40-60 microns.”
Eversole L.R., Rizoiu I, Kimmel A., Osseous repair subsequent to surgery with an erbium hydrokinetic laser system, International Laser Congress, International Proceedings Division, Sept 25-28, Athens Greece 1996, pp 213-221.
This is the inventors OWN WORDS with his/her OWN SYSTEM giving results of a “Thermal Coagulative Effect” with the hydrokinetic system.
Here is problem: It is not safe to tell any dentist that does not understand the thermodynamics and physics of these systems (95% of them) that they are using a laser device to cut BONE that does not produce HEAT! The inventors said it themselves in their own article.
THAT IS WHAT I WROTE. Check the DT thread. I completely agree with the first and last studies from Eversole and Rizoiu. It is the second study that I disagree with.
Finally, with the Bovine studies that you mentioned, again, THIS IS WHAT I WROTE.
I have not read either study that you have posted, but would certainly like to before a full comment.
1) Could you e-mail them to me?
2) Were the sites lased with the Er,Cr:YSGG energy with water spray on the site of irradiation/ablation in the bone, or with a system that sprays water in front of the beam?
Without having read the studies, my assumptions would be these:
A) 1st assumption is that there was enough water on the site of irradiation/ablation (as delivered by any delivery system)to act as a viable heat sink to prevent thermal damage to the bone. Since these were done in Tokyo, (no questions about the science), just which laser and water delivery system was the Er,Cr:YSGG crystal in?
2) 2nd assumption is that with either laser (Er:YAG and/or Er,Cr:YSGG) -(did all of my your just an OpusDent pusher critics catch that) if there was enough water on the site of lasing, the results seem reasonable.
Again, my main issues are with the “no heat” logic and an “aerated water spray” in front of any erbium beam on dental or bony tissues, instead of on the irradiaton/ablation site.
Waiting impatiently to see the studies. Thanks.
Eric Bornstein DMD
lagunabbSpectatorDr Bornstein:
Thanks for a very nice post. You addressed the light penetration depth nicely.
(1) I think your numbers are close enough for engineering purposes even not taking Shori’s et al findings into consideration. Now we have to throw in thermodynamics. The energy required to convert liquid water to supersaturated vapor is the enthalpy going from room temperature to 100 C plus the enthalpy of vaporization expressed in total enthalpy required per unit mass. Can you take a guess as to which part of the droplet (or water film) converts to vapor first? It is most definitely the outer shell whether you have a YAG or an YSGG.
You said
“If we are dealing with a 1 micron water film, then you are already into the dental enamel.”
No dispute there. That’s why many older experiments (Hibst 1997 for example) did not see any augmentation with water film or sprays. Fried et al used manually applied droplets on bovine enamel and found dramatic effects. Fried said it was a “thick” water layer but they didn’t measure the thickness. Even with the smallest syringes, I would think the droplets had to be much much thicker than a few microns. The results clearly surprised Fried et al as they mentioned not seeing that dramatic an effect in their prior studies with thinner water films + laser.(2) I am afraid we are in talking past each other here too and confusing others as a result. The shock that I am referring to is an effect of laser converting water to vapor. I am not talking high intensity femptosecond pulses causing photoablation (distruction by breaking of molecular bonds). Entirely different subject matter and I am afraid people are getting more confused by photoablation which is not the way current dental lasers work.
(3) You still haven’t educated us to the flaws in this paper: (here in its entirety)
http://www.etechadvisors.com/PDF/Pupal_temp_YSGG.PDF
You cited the study below regarding bone cutting. I haven’t read the paper (please email if you have it). It sounds as if Dr Eversol may have turned down the water spray to purposely achieve some coagulation or may be not. Also, since bone is much more porous than enamel, there is little advantage to having an external water film (or droplets). Just blast the water that’s already insitu by turning the water spray low and vaporize away. Again, I am guessing and would rather read the whole paper.
>>The following study however is the one that really stands out.
“The wound cavities were smooth, clean and straight. At 24 hours, the wound sites for both bur and Hydrokinetic System showed a clean cut margin with a thin zone of basophilia characteristic of a thermal coagulative effect.The zone measured 40-60 microns.”
Eversole L.R., Rizoiu I, Kimmel A., Osseous repair subsequent to surgery with an erbium hydrokinetic laser system, International Laser Congress, International Proceedings Division, Sept 25-28, Athens Greece 1996, pp 213-221.
This is the inventors OWN WORDS with his/her OWN SYSTEM giving results of a “Thermal Coagulative Effect” with the hydrokinetic system.
<<sorry had to be away for a few minutes so let me finish editing the post:
I am waiting for the Japanese YSGG papers on bovine bone cutting as well
(Edited by lagunabb at 11:25 am on Sep. 18, 2003)
ericbornsteinSpectatorLet me try to be clear on these points, from not only a physics point of view, but from a medical and histological point of view.
First, you posted:
I think your numbers are close enough for engineering purposes even not taking Shori’s et al findings into consideration. Now we have to throw in thermodynamics. The energy required to convert liquid water to supersaturated vapor is the enthalpy going from room temperature to 100 C plus the enthalpy of vaporization expressed in total enthalpy required per unit mass. Can you take a guess as to which part of the droplet (or water film) converts to vapor first? It is most definitely the outer shell whether you have a YAG or an YSGG.
Response:
Ray? We are dealing with infrared photons traveling at 300,000Km/sec! I do not think it means a dam thing what part of the droplet is igniting first, at this speed, from a force-counterforce perspective. When Newton’s third law is interpreted with propulsion in mind, the whole droplet is essentially igniting at the same time with a 2um absorption length in water at these speeds, unless the droplet is over 8um in size. Even then, (in my mind) there is no way “enamel cutting force” is or can be imparted on the tooth by the rest of the water droplet. I do not think simple enthalpy plays any significant part in arguments at relativistic speeds like this. Also, THE REST OF THE ERBIUM ENERGY IS STILL HITTING THE TOOTH FIRST. Bottom Line.
You posted:
(3) You still haven’t educated us to the flaws in this paper: (here in its entirety)
http://www.etechadvisors.com/PDF/Pupal_temp_YSGG.PDF
I have read the above paper many times, and here are my comments on its flaws:
First, and most important, the following were the only studies cited, when Rizoiu and Eversole discussed the “hydrokinetic system” being used in the paper.
1) Rizoiu I., and DeShazer L., New Laser – Matter Interaction Concept to enhance Hard
tissue Cutting Efficiency, Laser-Tissue Interaction V, SPIE Vol. 2134A, 1994.In this study, Rizoiu states:
“Hard tissue ablation occurs in a nonthermal mode with an erbium laser used in conjunction with a water spray…….. Most importantly, the critical role that the water spray plays in allowing the process to occur in a mechanical matter needs to be better understood.”
In this study, Rizoiu explains her new concept as essentially the UNCOUPLING of the THERMAL from the MECHANICAL in what is really an already well explained (at this time in 1994) Thermal-Mechanical ablation process with erbium lasers. NO WHERE IN THIS STUDY DOES IT MENTION AN AERATED WATER SPRAY IN FRONT OF THE BEAM. The study was done with a traditional water spray aimed at the irradiated tooth structure from a fixed point at 45 degrees. From where does she get the New Concept?
Even with the plethora of work published before 1994 discussing the Thermal-Mechanical ablative effect of erbium lasers, Rizoiu only references two studies in this paper. One well known paper from 1964, and one paper from 1989 discussing laser applications of erbium YAG lasers in dentistry.
That study was the predicate seminal work to the next two studies cited in the paper we are discussing, “Pulpal thermal Responses to an erbium, chromium, YSGG Pulsed Laser Hydrokinetic system” by Rizoiu, Kimmel and Eversole, published in Oral Surgery, Oral Medicine and Oral Pathology in August of 1998.
2) Eversole LR, Rizoiu IM., Preliminary investigations on the utility of an erbium, chromium, YSGG laser. California Dental Association Journal 1995:23:41-47.
I have requested the paper from the CDA, and have not received it yet.
3) Kimmel AI, Rizoiu IM, Eversole LR, Phase doppler particle analysis of laser energized exploding water droplets. Abstracts of the International Laser Congress; Sept 1996; Athens, Greece, Abstract #67.
This (Abstract) study is long gone and hard to find. I have never been able to find it (in all of cyberspace), and never spoken to anyone that has ever seen it. You be the judge.
Now, this study (we are currently debating) again is: “Pulpal thermal Responses to an erbium, chromium, YSGG Pulsed Laser Hydrokinetic system” by Rizoiu, Kimmel and Eversole, that was published in Oral Surgery, Oral Medicine and Oral Pathology in August of 1998.
In the results section of this study, Rizoiu et al states, “ On the basis of Phase Doppler partical analysis, Kimmel et al (see above reference #3) have proposed that the laser-target tissue interaction is dependent on a hydrokinetic tissue-cutting effect. Hydrokinetic tissue- cutting refers to the process of removing biologic materials through the use of high speed controlled water droplets. Strong absorption of laser energy at 2.78um by fine water droplets results in a violent yet controlled microexpansion inducing strong mechanical forces on targeted tissue surfaces. Resulting hydrokinetic forces produce mechanical separation of the calcified tissue surface, yielding quick and clean tissue removal. Other factors at the tissue interface that involve water, mineralized tissue, and photon energy may also contribute to the cutting effect.”
Let us try to decipher this paragraph in sections:
Problem #1: “Strong absorption of laser energy at 2.78um by fine water droplets results in a violent yet controlled microexpansion inducing strong mechanical forces on targeted tissue surfaces.”
What the hell does that mean? It sounds like they are describing the forces imparted on enamel by water expansion IN the enamel (the correct thermal-mechanical mechanism).
Problem #2: “Resulting hydrokinetic forces produce mechanical separation of the calcified tissue surface, yielding quick and clean tissue removal”.
Hydrokinetic forces from what? They have still not mentioned in this paper anything other than “microexpansion” of the water. THERE IS NO MENTION OF THE WATER BEING PROPELLED AT THE TOOTH.
Problem #3: “ Other factors at the tissue interface that involve water, mineralized tissue, and photon energy may also contribute to the cutting effect.”
NO KIDDING! It is only the other forces (that we all know as thermal mechanical ablation) that are contributing to the cutting effect!
They are completely Double-Speaking around the ablation mechanism, completely confusing and uncoupling the THERMAL from MECHANICAL in an attempt to explain Hydrokinetics.
Please, someone else chime in here and tell me if I am full of Sh-t.
With questions like that about their results, how should I interpret the Data?
Now, on to your Bone question:
You Posted:
You cited the study below regarding bone cutting. I haven’t read the paper (please email if you have it).
First, I do not have it in a PDF file. However, this is directly from the results section:
“The wound cavities were smooth, clean and straight. At 24 hours, the wound sites for both bur and Hydrokinetic System showed a clean cut margin with a thin zone of basophilia characteristic of a thermal coagulative effect.The zone measured 40-60 microns.” The conclusion to this study was essentially that the heat, and thermal coagulative effect in the bone, was equivalent to that seen with a dental surgical bur on bone. This is from:
Eversole L.R., Rizoiu I, Kimmel A., Osseous repair subsequent to surgery with an erbium hydrokinetic laser system, International Laser Congress, International Proceedings Division, Sept 25-28, Athens Greece 1996, pp 213-221.
Now, let us compare and contrast this hydrokinetic bone study by the Hydrokinetic System Inventors, to these results with Er:YAG lasers and water sprayed ON the ablation site:
Er:YAG bony ablation has been successfully accomplished in a variety of clinical situations. In a review of the use of this laser for middle ear ablation procedures, Frenz et al (1) stated that otological surgeons have identified the advantages of this laser for osseous surgery. These are the water absorption characteristics of the wavelength, and the precise bone ablation with minimal residual thermal energy. The histological data for Er:YAG lasers, when used by otological surgeons to perforate stapes footplate (osseous ear tissue) in surgical procedures, demonstrates that the lateral thermal damage associated with the bony cut was restricted to only 5-10µm beyond the cuts.
When attempting to cut nasal bone with a laser, Truong et al (1) described two specific criteria that should be met before a laser wavelength is chosen. These are rapid tissue ablation and an absence of visible char in the ablation site. They concluded that an Er:YAG laser produced an excellent result, and further stated that the addition of a water spray on the area being irradiated during ablation resulted in the lowest level of char and presumably the lowest thermal damage to the tissue. It was also noted that as long as the surface of the ablated tissue remained moist with a water spray throughout the ablation process, and the laser was used at appropriate settings, char was not seen regardless of the size/volume of the treated tissue. (2)
These results agree with an earlier study by Romano et al (3) using Er:YAG lasers to cut cortical bone. These investigators observed a linear increase of ablation depth with the number of pulses. A greater number of pulses, translates into more ablative energy in the area being irradiated per unit time. It was found that as long as adequate water spray was provided to the area, more bone was ablated with additional pulses (per unit time) without the char formation that would normally be an expected consequence of extra heat from the added pulses. It was also calculated that repetition rates beyond 20Hz would not significantly increase the peripheral thermal damage to the bone. These studies are germane since all commercially available FDA approved Er:YAG dental lasers function from 7 to 30Hz with a continuous water spray option.
1) Frenz, M. et al, Laser Applications in Middle Ear Surgery: Advantages and Possible Side-Effects. Lasers in Surgery: Advanced Characterization, Therapeutics, and Systems XII, SPIE Vol. 4609, 2002
2) Truong, M. et al, Erbium:YAG Laser Contouring of the Nasal Dorsum: A Preliminary Investigation. Lasers in Surgery: Advanced Characterization. Therapeutics, and Systems XI, SPIE Vol. 4244, 2001
3) Romano, V. et al, Bone Microsurgery with IR-Lasers: a comparative study of the thermal action at different wavelengths. SPIE Vol. 2077, 1994
Now, You further Posted:
It sounds as if Dr Eversol may have turned down the water spray to purposely achieve some coagulation or may be not. Also, since bone is much more porous than enamel, there is little advantage to having an external water film (or droplets). Just blast the water that’s already in situ by turning the water spray low and vaporize away. Again, I am guessing and would rather read the whole paper.
My Response based on the above literature findings:
First of all, PRIMARY FOCUS OF CUTTING BONE IS TO KEEP IT COOL. There is absolutely NO reason to want or desire coagulation in bone. Ultimately we want the bone to heal. This occurs with the pluripotent mesanchymal cells from the marrow spaces repopulating the area where the bone was ablated to form new bone tissue. Under no circumstances do we want to heat (to a point of coagulation) the haversian canal system in the bone that will act as a conduit to repopulate the bony ablation site with these bony osteogenic and morphogenic cells. ALL RELEVENT STUDIES DISCUSSING CUTTING OF BONE WITH LASERS THAT I HAVE EVER SEEN, AGREE WITH THAT LOGIC.
Even Rizoiu:
“It is already known that the infrared lasers are more likely to be associated with a thermal mechanism that causes vaporization of bone structure. The absorption of laser energy (which occurs when the tissue components absorb the laser wavelength), and conversion into thermal energy results in a local deposition of heat. The dissipation of thermal energy into the surrounding tissues is a process that continues to occur even after laser exposure. This process will enlarge the damage envelope when no limiting factors occur. Many studies suggest that cooling the ablation site will reduce the amount of heat that is transferred into the surrounding tissue.”
Rizoiu I, and Levy G., The Efficiency of Bone Ablation with an Nd:YAG Laser Beam Delivered with a Cooling Spray: An In Vitro Study, Compendium, VolXV ,pp106-111, 1994.
Ray, unfortunately it seems to take someone with significant background to take this argument apart and make sense of it. I have the significant background, and to me it makes perfect sense.
1)Er:YAG’s produce less heat.
2)Water spray on the irradiation site acts as a necessary heat sink.
3)Water (in any form) in front of the beam attenuates the ablation effect, and requires more energy output for the ablation.
4) Please do not try and bullsh-t me with an effect that has no real basis in fact (that I can see) and the the inventors (in your cited article) either cannot, or will not adequately explain.
5) ALL of these lasers are safe and effective if used properly. BUT THEY ARE SAFER IF DR’S ARE TOLD HOW THEY REALLY WORK, AND WHAT KIND OF HEAT THEY PRODUCE.
Eric Bornstein DMD
Robert Gregg DDSSpectatorQUOTEQuote: from lagunabb on 12:46 pm on Sep. 18, 2003
Bob,when and where did Biolase ever make or made the claim below?
“The photons are completely absorbed into the water droplets and the droplets accelerated to the speed of light (apparently) towards the target tissue.”
It’s one of those statements that make me question your knowledge of physics and/or your credibility.
(Edited by lagunabb at 9:49 am on Sep. 18, 2003)
Ray,
There you go again…………“It’s one of those statements that makes you question……”
 What other statements cause you to question my credibility, Ray?
What other statements cause you to question my credibility, Ray?
There are ways to ask the question you made w/o being disrespectful such as you were in adding your last sentence.
Since you have raised questions regarding my credibility in a public forum again gives me no other choice but to respond to your unfair and unjustified characterization of me.
How does a word description of a still photo describing the depiction in the animation make the stretch to impugn someone’s personal/professional credibility? It seems easy enough for you, as I have seen now on two separate forum postings of yours.
(My apologies to Ron and the forum, but I’m not putting up with the personal disparagements for sharing the marketing and claims material put out by the company Ray seems to want to protect (for what reasons?), or for having a differing opinion that has twice been put in personal terms and questions my knowledge and credibility regarding laser physics and laser tissue interactions–especially since I have made personal phone calls to Ray attempting to invite better decorum from him. Extended olive branches don’t seem to work…….:confused: )
First, Ray, I will answer the question you pose, and point out the obvious:
The statement I made was in reference to, and in description of, the animation that the quote appeared beneath. That’s because the forum does not allow the animated GIF files, so I could only post it is a JPEG.
I never once said that Biolase made that statement. It was a caption to a photo, describing the animation not viewable
But you already new this as I sent you the animation in an email for your comment on August 13, 2003 and you replied the next day with this, “I have seen that vastly idealized version of “HK” before. Not sure how to describe my impression of that Web site other than that I am glad that it is a dentist rather than Biolase hyping.” So you knew very well what I was describing, and you used that lack of clarity in the still photo to impugn my credibility in an online forum. Shame on you, Ray.
Your first post to me about the animation photo is also revealing in the embarrassment you felt at first for it, knowing what the animation really was showing. So, then you decided to be disparaging since you didn’t think others would know.
If YOU are going to be credible, then you need to make the quote in the context of which it was given, and with the understanding of the animation that you already had! Not to do so exposes your credibility into question.
I have been reading your exchanges with Eric Bornstein on Dental Town and here, and while I don’t question your understanding of physics in general (certainly better than mine–as I don’t have an advanced degree in it), I absolutely do question your knowledge and/or credibility of laser physics and your knowledge and/or credibility regarding laser tissue interactions of human teeth.
What have you ever done in the lab, in a research project, or in live humans on their teeth? What clinical or applied problem have you solved? Where’s even the slightest research or clinical credibility from you as it pertains to applied physics, not just your theoretical fantasies?
Have you ever used a single laser on a single human tooth? How about in soft tissue? I have used ALL types of lasers–including erbium YAG, Holmium YAG, Neodymium YAG, to name a few–experimentally and on human teeth and soft tissue, and I have been using them clinically and researching them for over 13 years. Very few other clinicians have more knowledge or expertise in understanding how different lasers work on dental tissue than I do–and I certainly won’t take a back seat to you or what you think about my knowledge and understanding. And I certainly won’t take the disparagements from those who think they “Know-it-all” because they are making a some money and therefore think they know more about human laser tissue interaction and mechanisms because they have studies some theoretical research, than I do.
I was researching erbium lasers in 1996 in the lab before Premier or Biolase (I think they were still calling themselves “Laser Medical Technologies” then–I wonder why they have changed their names so many times over the years, Hmmm?) had a decent product or even an FDA clearance. I worked then and still work with former Premier and Biolase engineers. I addressed and solved some of the clinical problems I see being discussed (“discovered” ) by erbium laser users here and on Dental Town back in 1996 and 1997. So I have a pretty good working knowledge of lasers, the delivery systems, the physics, the effects on human tissues (not beagle dogs) etc. I have seen the so-called HKS effect using erbiums AND neodymiums, and I understand how someone could draw an idea that there are photo-acoustics and photo-mechanical effects in play (versus photo-thermal mechanical effects).
As Dr. Bornstein and others can tell you, once you hit human teeth with a pulse of laser light, that substrate tissue changes into another substrate. And vital human tissues, I have found, react differently in the controlled lab experiments that I seen over the years than what my findings have been clinically. But, then according to you, I don’t know what I’m talking about.
But building a company, a product, a marketing campaign on a theory that is not yet resolved in the minds of scientists or clinicians is putting the cart before the horse. And anyone who feels that something as revolutionary as cutting teeth with energized water would be (if true) is appropriate to sell devices and shares of stock, based on the “new theory” w/o scientific or clinical acceptance, needs their credibility license revoked.
Well, over the past 13 + years now, in turns out I’ve known more about this stuff than a whole lot of folks who thought they were smarter, more knowledgeable, or credible or whatever than I. Guess what? I’m still here. The others are gone. I have outlasted all the past engineers and laser company executives and investor/underwriter Know-it-all types that have come down the pike for the past 13+ years (ADL, Premier, HGM, Sunrise, Excel-Quantronics, Laser Endo-Tech–now Biolase), and I’ll bet I’m still practicing laser dentistry long after you and the current crop have left the laser dentistry marketplace to make your money elsewhere.
Your interest in denying credibility to others, it seems to me, is in anyone that doesn’t see it the way you have a bias for. You want to believe in HKS, I suspect, because it stands to make you money, not because it results in a better bond to dentin or you enjoy the collegiality of dentists on dental forums (that myth got put to bed with your last post).
I have a bias for what I believe, as does Dr. Bornstein. But my bias came before my investment in the lasers I bought, acquired or use on my patients. And I continue to re-evaluate my bias from an objective viewpoint. Objective? Yes, because my patient’s health and welfare requires it. You wouldn’t understand that sort of ethical integrity to those who you must care for physically–because you are not a heath care professional. As health care practitioners, we have an ethical duty to assess the devices and materials that we consider for our patient care. My ethical duties to my patients is a higher duty than a business or fiduciary one. (Can you say Enron?) That professional objectivity is what encourages and requires us to take an objective outlook–even as a corporate officer of a manufacturer who is a practicing clinician (and perhaps more so since I am both). Your objectivity has been lost to your bias over wanting the stock to perform to your liking. With your objectivity lost, your credibility is now gone as well.
On this forum, I discuss the physics and the tissue interactions of ALL types of lasers in order to better understand and help others understand what they do to and for our patients. You do it in order to profit financially.
Why else are you here Ray? You certainly not here to learn about patient care. And, even though I don’t measure up to your knowledge of laser physics, I understand it better than you know or may want to acknowledge. Anyway, I don’t think this forum was established so that you or anyone could make personal insults and denigrate others, let alone those who contribute to the entire forum contents.
However, you aren’t the only one to throw personal aspersions my way from the HKS persuasion. I have experienced, this week in fact, personal attacks on me and my credibility by folks at the Biolase company, that when I confronted them on it was dismissed as, “just hearsay, you know how it goes in this industry….” Well, I guess I do know know that’s how that company “goes”. I guess that’s just how that company and you have decided to deal with me and my professional differences with what you and they advocate–personal disparagement.
Seems I’ve been down this path before with other companies. When the company and their minions feel they have to be nasty to promote their product and sales, and get personal and denigrate those who disagree with them, the nasty run out their professional welcome.
Sorry for the rant everyone. But I’ve had enough of the personal insults and affronts to my credibility that have been regularly coming from due South of Cerritos!
Robert H. Gregg, DDS
Robert Gregg DDSSpectatorEric,
I would love to chime in on your discussion with Ray, but your logic and science and facts are doing a terrific job.
Ray simply doesn’t want to accept that the company he has invested lots of money in, makes sales on a “New Theory” that is not supported in science, and is likely to be a discredited theory soon, as will be the company for promoting it.
I have watched Ray talk back and forth with you here and on DT, try to match your references, stretch the findings to suit his bias and interpretation, and he has failed completely to provide any credible evidence or science that HKS is in play. And when that hasn’t worked, he trys to talk over and around your well stated and supported points.
You are absolutely correct on the mechanisms in play for pulse durations in the 140 to 400 microseonds that are comercially available today for the dental marketplace.
In pulse durations of 1 microsecond or less, Ray may have a point. But that’s not what our erbiums used in dentistry deliver in pulse duration.
Bob
SwpmnSpectatorHey Guys!!!!!!
Boy I sure am enjoying this debate but can we try to be nice and not question one another’s credibility? Let’s just argue the evidence for and against photon energized water ablation and not get into personal attacks. Like Glenn said this weekend, the pub is at <a href="http://www.dentaltown.com!!!
Thanks,
Your” target=”_blank”>www.dentaltown.com!!!
Thanks,
Your Friendly Thursday-Saturday Temporary LDF Board Administrator 😉
lagunabbSpectatorDr Bornstein,
The posts are getting quite long so I would first like to discuss the Pupal Temperature Response experiments by Riziou et al. My understanding of what you view as problems with the paper are the authors limited citations of prior work and their characterization of ablation mechanics (HK). You did not address directly the meat of the article which is the pupal temperature response data on beagle dogs. Do you see any problems with the way the measurements were done, the data, or the way temperature response was interpreted.
Thanks.
(Edited by lagunabb at 7:47 pm on Sep. 18, 2003)
lagunabbSpectatorBob,
When referring to the claim that water is being accelerated to the velocity of light. You wrote:
“I never once said that Biolase made that statement. It was a caption to a photo, describing the animation not viewable”
Who made up the caption? You or Biolase? I remember the web site you pointed me to in the email (Chris Walinski DDS) and I would have noticed a caption like that!!
I stand by the opinions I made to you in private emails or public forums and you have my permission to reveal them and the same goes with the emails I send to others here.
PS. I would rather not reveal in detail my long or short positions in any stocks. I will say that I have a long position in Biolase whereas I had no position a month ago. It would not be in my own interest to be subjective rather than be objective when it comes to the technical and business underpinnings of various companies I am interested in, whether long or short. Of course we all operate in an environment of imperfect understanding and I assert my right to be as wrong as everybody else contributing to the discussions and I acknowledge that many of you know much more than I do. I also see respected “gurus” throwing unsubstantiated statements (perhaps just for the sport of it) with the expectation of not being challenged.
(Edited by lagunabb at 8:39 pm on Sep. 18, 2003)
-
AuthorPosts
