Forums › Diode Lasers › General Diode Forum › Laser perio consult
- This topic is empty.
-
AuthorPosts
-
AnonymousGuestHi all,
Lady mid thirties presented today with this tooth(see xray below) 10mm pockets mobile. Went to periodontist last week who did probings and rescheduled next week for FMX and ext 4. Generalized 5-6mm pockets .No medical problems.
Lady desperately wants to avoid extraction. Any hope in scale and root planing followed by tx with diode (sorry Bob , couldn’t get her to go out to see you) and occlusal adjustment?
I’ve had pretty good success with 5-7mm pockets resolving but have not attempted any like this. I’m willing to try, she’s willing to try knowing she will still probably need ext. Is it a total waste of time? Thoughts? Suggestions?
Thanks[img]https://www.laserdentistryforum.com/attachments/upload/dmack.JPG[/img]
whitertthSpectatorwhat do u have to lose? I would try with no guarantees….if it works u have a nice case to publish…
RodSpectatorAny chance we could see a VERTICAL BWX?
Here’s what I’d try:
First of all, I’d do NO pre-surgical root planing, etc. Pre-surgical (phase 1) root planing could cause the tissue to firm up and shrink. It would also cause the immunilogical factors that are present in high amounts to diminish (by becoming temporarily more healthy). This means that the tissue would be more difficult to manage if it had shrunk and become more fibrous. And you WANT all those immunilocial factors present in mega amounts when you do regeneration. (learned this from Bill Becker himself)
Some sort of temporary splint — even if you had to put a glass fiber ribbon splint on both the buccal and lingual, with the idea that with success, you can remove. Keep it away from the gingival area.
I currently don’t use the laser when I do these. But it certainly couldn’t hurt (possible biostimulation?).
I’d do a great endo. I personally think this is a must. With this much bone loss, there has got to be some endo problem via lateral canals — lotsa literature to back this us — esp. by Selzer (sp?). They’ve shown that even when you get a normal pulp response to EPT and thermal tests, when there is this much bone loss, there are virtually ALWAYS areas of ischemia in the areas of the lateral canals.
I’d flap the area, root plane WITH ZEZA ULTRASONIC CURETTES (this is important in my opinion), absolutely impeccable debridement of the boney defect with the same ultrasonic curettes, taking away a little layer of bone. Just be sure to ONLY use the ‘root planing’ inserts, and NOT the surgical inserts. The ‘surgical’ ultrasonic curette inserts are WAY too aggressive, even for the debridement of the osseous defect (which is what they’re meant for). Just use the ‘root planing’ ultrasonic curette inserts for both root planing and osseous defect debridement.
And yes, do de-epithelialize the internal of the flap, but don’t get all that aggressive — you don’t wanna impair circulation in the flap.
OH, by the way, very important — when you give anesthetic, be sure you use 1:50,000 epi at least 25 minutes prior to your incision. And be sure you give it both buccally and palatally adjacent to the root. This will give you good hemostasis, and that is important in this procedure.
So after your GREAT root planing, GREAT debridement of the defect, and de-epithelialization of the internal of the flap, treat the roots with PrefGel (by Biora — the Emdogain people) for 2 minutes. Literature says you could use citric or even phosphoric acid, but in much shorter times. I disagree. Citric acid will denature proteins, and I don’t like that idea. And phosphoric stimulates bleeding — not good with this technique.
Rinse well. At this time you should have virtually no bleeding.
Inject the Emdogain gel into the defect, onto the prepared root surfaces and to the internal of the flap. Then place your graft material (I’ll discuss below)to fill the defect and close with matress sutures (you don’t want the suture material going through the graft material. I suture with GoreTex sutures. You need to get primary closure.
If I get EXCELLENT primary closure, I usually don’t put on packing. But if the closure is not as ‘sealed’ as I’d really like, then I place packing.
The graft material. I specifically like the Pepgen P-15. Consider this — we know that DFDBA (Demineralized Freeze-dried Bone Allograft) will hasten bone regeneration to a degree. It’s been found that only one out of 3,000 proteins in DFDBA is responsible for this enhancement of bone regeneration. And that protein? Yep, it’s ‘P-15’. Obviously a product that is saturated with pure P-15 is a big plus — studies of this are totally awesome.
But P-15 is dense as all get-out — and this would prevent in-growth of blood vessels and bone percurser cells. So I mix DFDBA and Pepgen P-15 in about a 50-50 mix. The DFDBA will resorb very quickly and is very spongey — thus allowing rapid ingrowth. And the Pepgen P-15 will accelerate attraction of these cells.
I first mix them together when dry (much easier to get a homogenious mix when dry). Then I hydrate with sterile water — I personally mix just a ‘pinch’ of tetracycline in with the water first.
Place the tetracycline in some sterile water (or saline) — just a VERY LITTLE (we don’t want the HCl in the tetracycline to give us much acidity). It should give the water only a very slight hint of ‘yellow’ if you only put the slightest bit in. Let the solids settle to the bottom and suck up the top of the water in a syringe and squirt that into the graft mixture to start the hydration. I do this right before I make my flap. The material should hydrate for a minimum of 15 minutes.
And don’t ‘float’ the graft mix with this water. Once the DFDBA absorbs the water, you want it rather dry (barely moist).
I don’t use a membrane. The Emdogain enhances acellular cementum formation, which in turn forces fiber generation, and that in turn forces bone generation. And the graft material then enhances the ‘fill in’ of the bone between the teeth. If you use ONLY Emdogain, you sometimes get only a thin coating of bone forming on the root surface, with no bone inbetween — this is still good, but I’d prefer bone right straight across.
Emdogain has been found to prevent epithelial down-growth, so I don’t use a membrane. Pepgen P-15 has also been shown to prevent epithelial downgrowth, but this may not apply when mixed with DFDBA (don’t really know)
I then place the patient on Peridex rinse as well as Doxycycline 100mg bid for 2 weeks.
When I say that these patients have no post-op pain, I mean they have NO post-op pain. It’s weird!! You haven’t ‘recontoured’ bone. You haven’t place irritating membranes. And I truly think there’s something about the Emdogain that virtually tells the tissues that nothing has been done.
So far, every single patient, without exception, has said they didn’t even need to take Advil or Tylenol! I kid you not!
GTR membranes always seemed to work very well in my hands, yet this technique has results that are even better.
So yes, if the patient wants to ‘try’ to save the tooth, I’d say OK, and THIS is the technique and approach I’d use.
How ’bout that vertical BWX?
Rod
(Edited by Rod at 12:39 am on Jan. 25, 2003)
2thlaserSpectatorNow, Rod has GREAT perio background with excellent results, so I would go with his advice here, depending on your skill level Ron. Not all of us, especially myself, has done alot of what Rod has done, but am learning. I would DEFINITELY perform a laser root canal, using the Waterlase, and it’s incredible effect on the tubules in the canal. If you haven’t seen the SEM’s of that, I can send them to you, they are incredible. Since my staff has seen them, I am NOT allowed to perform endo without the use of the Waterlase! We have had GREAT results. I think that you DO have a combined endo/perio/occlusal issue here. I agree with Rod, a vertical BW is very helpful. If you have any questions on the RCT with the Waterlase, just ask. It’s so very easy. Great case, I would DEFINITELY try it. I have had a similar one, and we had excellent success with it so far.
Hope this all helps you decide what to do, from us in the peanut gallery!
Good Luck!
Mark
2thlaserSpectatorPS…if you haven’t done so already, I have replaced using a scalpal for incisions. I use the T-4 tip with about 1W 13%air, 11%water, and have had success with very little bleeding whatsoever, and a great “playing field” in which to work in during flap surgeries. The tissue approximates back excellently, BUT DON’T use too much wattage. Low powers are so effective, especially with the T-4 tip, which seems to exude much more energy per pulse than the G series tips. Just a PS.
Mark
AnonymousGuestWow ! Thanks for the input guys. I have lots to present to my patient.
Rod, I knew you would have a very well thought out approach to this. What’s even better is , once again you’re willing to share it with the rest of us. I checked out the pepgin on line and got an idea of cost but what about the emdogain, as expensive? Got all the literature ordered from Biora.
Mark, I haven’t picked up a scalpel since August. Fortunately on my training day, I did a crown lenghtening where a flap was layed using the laser.Since then I use it for all my surgical extractions or other things I need to flap. I also found the 1.0w was very effective but I think I have the water and air a little lower than you 7/11. How ’bout posting the endo procedure you’re doing? I saw the SEM’s in Ft Lauderdale at the Biolase meeting last spring and they are impressive. I just didn’t get a clear understanding of how, once the laser had cleaned the canal , how the endo was filled. Tapered canal or what do you fill with?Soon as we get the vertical BW I’ll post and let you know if my patient wants to give it a go.
Thanks again,
smileagainSpectatorHi Ron
I saw your 1/26/03 request to see Mark’s Biolase endo procedure which I would like to view. Has it been posted, if so how can I find it?
With thanks,
Jerry Rosenfeld, DDS
Avon, CT
AnonymousGuestJerry,
I don’t think it has been posted. the SEARCH link at the the top of the page works pretty well for finding topics that have already been posted. Your reminder will give Mark another chance to build those posting numbers 😉
Robert GreggParticipantHi Ron,
This is an occlusal/orthodontic/perio problem in my opinion. Look at the bone loss on the distal of the molar, and consider the absence of the second molar in the occlusal scheme of disease.
Like Rod said, it needs splinting and most likely endo.
Are there anaerobes to be dealt with. I’d say so.
Rod has studied perio a lot longer than I have, and knows a lot more about it than I do.
I agree with Rod on no pre-surgical S/RP 100%.
I also agree with Rod as to splinting (i.e Ribbond).
And I agree with the likihood of endo (with a qualifier).
But I would not (probably cuz I can’t) get as elaborate as Rod would.
I would treat the pocket with a pulsed Nd:YAG, use peizo electrics to lightly debride the root surface, make sure I developed a stable fibrin clot using my laser of choice………
Then I’d leave it alone for 9 months.
Here’s some stuff previously published in Dentistry Today, but with a new unpublished color graph of each probing site as they healed over 27 months. It helps one to appreciate the 3-D aspect of these defects. There are no “distal” bacteria, nor “mesial/mid-root” bacteria.
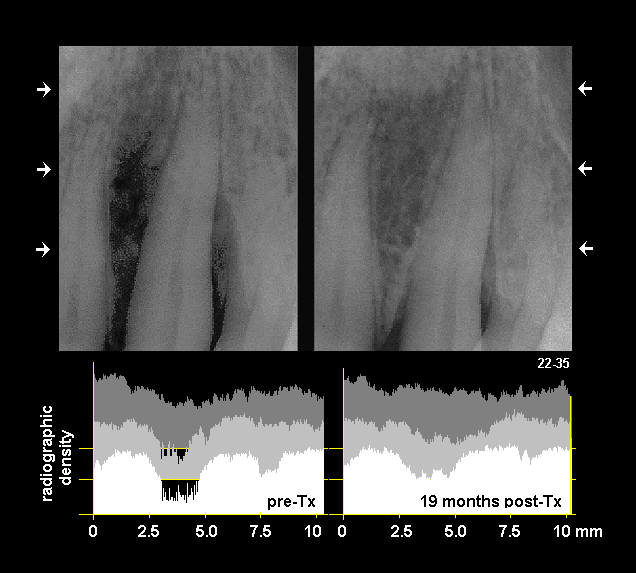
This tooth was treated only once in the first 9 months. The “mesial” defect was 19mm and the “distal” defect was 16mm.
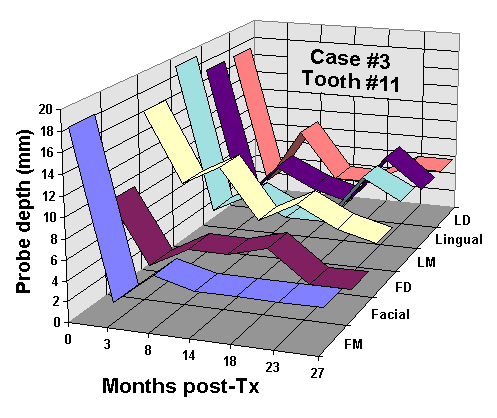
This color graphic shows the pocket reduction for each of 6 probing sites over a 27 month time frame.
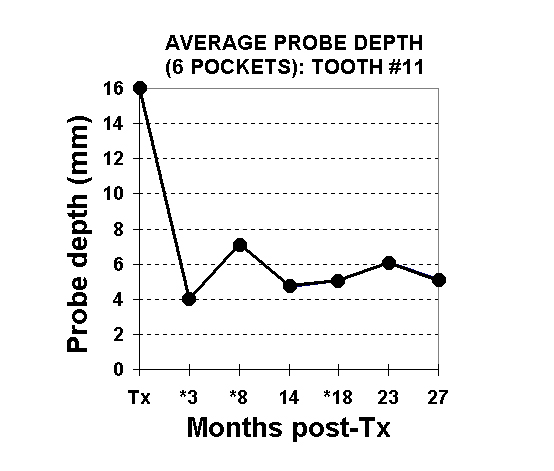
This graph depicts the total of all 6 probing depths averaged at pre-treatment; and the average pocket depths over time.
What is interesting, is that healing of periodontal defects–regardless of the method employed, tend to show a similar “rebound” effect at 3-6 months (a reverse “hockey stick”).
What was of great interest to us, is that use of LPT kept the pocket depths stable over 27 months without retreatment (except for the distal 6mm which was retreated 3x’s over 4-5 years).
Bob
(Edited by Robert Gregg at 4:43 pm on Feb. 19, 2003)
AnonymousGuestBob,
Only the 1st image uploaded. Email me the 4 and 3 jpegs and I’ll post them
Thanks
lasersmiledrSpectatorHi Ron!
Great question! I have experience with the Diolase ST. The functional capablilities of each of these devices are different. I have tried several similar cases in the past. I did note as Bob and Rod mentioned earlier, occlusion is definately key in good perio therapy as well as splinting and removable occlusal splints
Due to the wavelength and absorption characteristics of the diode lasers, lateral damage is a significant issue. Often the very tissues that could form new bone and attachment, are burned with the intensity of Diode laser hence, the attachment desired is not achievable.
To this date, I have not seen a paper that outlines a logical protocol with repeatable results. Although this would be advantagous to the manufacturers to prove and provide this information, I do not see anyone pursuing this project.
I would be very interested to see the long term results on this case. I have a few myself that I don’t mind sharing. Several of these I later retreated with the periolase after the marginal results achieved with the Diode. I did find that wavelength and pulse duration is extremely significant in the outcome in such cases.
I also noted that while crown lengthing with the diode worked quite well, I did not have control of healing as well and if used in the anterior region, often led to an undesirable margin exposure. The NdYAG allows for much more control in the esthetic zone and I now do all crown lengthing procedures (specifically soft tissue) at the same time of preparation. With proper use, I have yet to have an undesirable result and far superior hemostatis than Diode or Er.
Again, high peak power, with much shorter pulse duration with this specific wavelength lend to greater control of tissues and hemostatis.
Best wishes in your search for more answers!
Todd McCracken, D.D.S.,M.A.L.D. 😉
-
AuthorPosts
