Forums › Diode Lasers › General Diode Forum › Laser Perio
- This topic is empty.
-
AuthorPosts
-
Robert Gregg DDSSpectatorQUOTEQuote: from Swpmn on 7:55 pm on June 30, 2004
One more question for anyone that has used lasers for treatment of periodontitis. Gregg, Kaminer, Kimmel, Schalter please chime in here:I don’t know much about either diode or Nd:YAG periodontitis treatment protocols but it seems I’ve been told the diode fiber should be placed 1mm shorter than the perio pocket. On the other hand, I think Rusty Schaeffer told me with the LPT protocol the fiber should be placed to the full depth of the periodontal pocket???
What is the logic behind these differences? Does it relate to activated vs. inactivated tips or pulsed, high-peak powers attainable with the Nd:YAG?
If the doctor has to re-measure each perio pocket and then re-set his fiber length with a diode, isn’t that a real PIA(Pain in the A$$)? Who actually does this and how practical is it considering diode laser handpiece design? We should have fibers that are marked in 1mm increments!!! But the laser would probably focus on any pigmented markings.
So on number four I have a mesio-buccal 4mm and on the disto-buccal I have a 6mm. I’m actually going to stop and extend my diode fiber from 3 to 5mm for the DB pocket?
 ? This seems silly and not clinically reasonable.
? This seems silly and not clinically reasonable.Al
Al,
Ron said it better than I could. He is exactly right.
You’ve got your hand on some of the critical differences between diodes and FRVP Nd:YAGs.
With the diode activated, one should not be trying to touch the bone. However, since it is a hot piece of glass, the soft tissue might very well be “quenching” and cooling the activated tip down to a warming effect. Very bad in lasers. You want to reach ablation thresholds, so the hotter the better to some extent. Warming is very deliterious. So the proscription against diode on bone might not be for the reasons many think and advance.
But a lot of this goes WAY back to the pseudo-pscience political proscription against using even the FRP Nd:YAG on bone many years ago. Why? The Academic Thought Police in the ALD.
1mm short of the measured pocket depth (with or w/o anesthetic???) was the established reason as part of the Curriculim Guidelines for Standard and Advanced Proficiency. If you didn’t say that as part of your presentation, you got points deducted–perhaps even failed.
We have been “walking” on bone for over 12 years. Well that little fact didn’t put us in good with those who had a different “opinion”.
The fact is science supports FRP on bone for a number of reasons and beneficial biologic effects.
Furthermore, it makes absolutely no clinical or SAFETY sense to put the fiber short of the depth of the defect. You cannot always determine just where your fiber goes in the closed pocket. Sometime you “bump” into bone, calculus, root protuberance, fibrous tissue, or pocket wall. Even w/o firing the laser, you can pull the fiber out and have LESS fiber than when you put it in!
Now, did you break it off in the pocket? Or did you just push it up into the canula? Only a FLAP will tell for sure!
With the fiber extended to the pocket measurement PLUS 3 millimeters, if you break a fiber against bone or something, you simply grab some cotton pliers, pick it out and move along.
Unfortunately, a lot of the stuff that folks were told years ago that were advanced by non-clinicans–including one-patient-a-week academicians–was just not accurate, practical or even safe, let alone effective.
There is no other reason that two full-time practicing clinicians came up with the LPT/LANAP protocol, that is the ONLY protocol to prove human periodontal regeneration with lasers in a controlled human histology study, than we did it by day-in and day-out clincial practice which I define as a daily exercise in Problem Solving of patients’ severe, hopeless, or painfull issues they present into our private practices EVERY DAY.
Sorry for the rant, but this is one of those hot-button topics where Del and I get so annoyed over the “accepted” thinking, when the evidence is otherwise.
Bob
whitertthSpectatorI really do love that i started this thread beacuase I have learned alot from the multiple posts…I have some questions that may seem silly Bit I have a mental block on this subject…
We know with the diode we stay 1mm from the base of the pocket totally away from the attachment…. Clinically we see very often great results in pocket shrinkage yet the belief is that is long junctional epithelium not attachment…. If that is correct..and we can repeat the diode procedure when that breakdows since it is isnt as stable as attachemnt…is that acceptable and if not why? Are there studies and I’m sure there must be of the stabilty of Long junctional epithelium… With the periolase are u going throught attachment partly because reattchemnt definitetly occurs so it is predictable and safe? Just trying to understand some more…
Loving this thread….
Kenneth LukSpectatorHi Bob,
It’s great that you are answering all these questions and confusions over this topic.
I hope I’m not going to cause more confusion ( just myself) or going through the basics here:
1) For LPT, I thought the first pass with the Periolase was to de-epithelialise the poscket as well as remove debris. At least that was my assumption from the diagrammatic LPT protocal.
2) Diode decontamination was to carry out after SRP in a non-activated mode. Does this not penetrate into tissue to remove bacteria? (or not as effective since the intensity is much weaker than Nd:YAG.)Ken
(Edited by Kenneth Luk at 11:07 pm on July 1, 2004)
Robert Gregg DDSSpectatorHey Ron,
Q&A format:
We know with the diode we stay 1mm from the base of the pocket totally away from the attachment…. Clinically we see very often great results in pocket shrinkage yet the belief is that is long junctional epithelium not attachment….
Resolving inflammation (regardless of the technology)will get pocket reduction and long JE–even some bone that will push up against the long JE. We saw that in Yukna’s study with the S/RP control group, but it was “repair” not regeneration.
If that is correct..and we can repeat the diode procedure when that breakdows since it is isnt as stable as attachemnt…is that acceptable and if not why?
Sure, it is acceptable because it is “health” (the absence of disease). But who wants to keep retreating pockets, any more than retreating endo or restorative? And what a chair time and practice management nightmare it was 14 years ago when I used to do it that way. I mean, how do you charge for a service that requires repeated re-entries and later on retreatent? What do you say to the growing # of patients that start asking why the need for re-treatments?
I guess I could keep putting IRM into a cavity prep, or I could take the time and use the right materials to bond a long lasting restoration and charge a comensurate fee for that service…….;)
I see too many perio patients to try to manage such a population of patients that will eventually be breaking down. I’ve been doing about 2 quads of LPT at ũ,000 per quad for the past 2 weeks–some days 4 quads. I want to minimize the # of patients I need to re-treat and revisit by creating a stable new attachment.
One of our doctors in Texas recently did 48 quads in 6 weeks at 迲 a quad after some media exposure. If he isn’t doing single treatment LPT–one visit per quad, and one quad per hour–he’s not going to address that sort of volume with repeat entries and eventual breakdown…….
Are there studies and I’m sure there must be of the stabilty of Long junctional epithelium…
I would have to check.
With the periolase are u going throught attachment partly because reattchemnt definitetly occurs so it is predictable and safe?
Yep. And well established in the perio literature.
Hi Ken,
1) For LPT, I thought the first pass with the Periolase was to de-epithelialise the pocket as well as remove debris. At least that was my assumption from the diagrammatic LPT protocal.
Yes. Also to:
1. to trough the tissue open, thereby creating a “funneling” of the coronal/crestal tissue at the gingival margin.
2. create a blood free environment
3. establish access and visibility by relaxing the tissue tension on the gingival crestal tissue.
2) Diode decontamination was to carry out after SRP in a non-activated mode. Does this not penetrate into tissue to remove bacteria? (or not as effective since the intensity is much weaker than Nd:YAG.)
Diode decontamination from my experience and Harris’ study is a surface effect. FRVP Nd:YAG is a surface AND sub-surface effect 2-4mm. That, and Harris’ study showed Nd:YAG has a 16 fold increase in lethality of PG than 810nm diode w/o effecting the blood agar.
Good questions!
Thanks for starting the thread Ron!
Bob
Kenneth LukSpectatorHi Bob,
I hope I’m getting this right and not boring everyone:
1) For Nd:YAG,when the fiber enter the pocket un-initiated, the laser removes bacteria / debris (Does the laser de-epithelialise without initiation? How?).
Then the fiber periphery gets clogged up with these proteins helping to remove more tissue and debris but there is a temp increase ( not as much as a hot glass effect ).
2) An un-initiated diode can only do biostimulation , coagulation ; and surface decontamination ( no sub-surface decontamination as the intensity is low.
High enough power produce heat stacking effect causing bacterial decontamination BUT collateral tissue damage.
Thanks,
Ken(Edited by Kenneth Luk at 2:11 am on July 3, 2004)
dkimmelSpectatorI have actively used the diode to tx periodontal ds for close to a year. Taking the patient through RPC’s decontaminating the pocket then de-epithelialise the pockets. 3 mo. later I was seeing relapses. Since I like to spend money I bought the perioscope. In every case there was still calculus present.
Then I tried using the perioscope at the RPC appt. . This did not work because it takes 1 hour to do one root surface if your lucky. Finally settled on doing the RPC using the laser then waiting 3 mo. reeval for relapse and then treat with the perioscope. After which you start all over again with the laser.
This procedure will work. Is it Long junctional epi attachment? Do I get any bone regeneration? In some case it is just LJE attachment. In some of them I did get bone regeneration.
The problems:
1. Not predictable.
2. Labor intensive.
3. The laser if used only by the dentist becomes costly.
4. Patient compliance is a real big problem. They have to be seen every 7-10 dqays.
5. A scheduling nightmare. Imagine having a bunch of patients you have to stick into your day just for a couple of min.This is what I do until I can come up with enough money for Bob and Rusty.
1. I’ll do RPCs as usual only using the diode to decontaminate the sulcus.
2. Reeval at 3mo.
3. Unresolved sites are then treated with the perioscope.After which we start with the deepi. sequence and see them as needed. Unless there is a restorative component and then they go to sx.David
Dan MelkerSpectatorDavid,
I know I can’t get in trouble for this statement. Today, Bob Gregg and I were talking about remaining calculus with the Periolase. Bob said Cobb found up to 50% remaining calculus after debridement yet high degree of success.
Bob certainly can back up what he says. I have always thought all calculus must be removed for regeneration and in fact have failures when I reenter procedures where calculus was left. However the calculus was not detoxified. Really interesting because potentially it could totally change the way we treat perio disease.
If Bob you read this, I am still unclear how reattachment occurs through the calculus so we now have regeneration.
Thanks alot Danny
Robert Gregg DDSSpectatorHi Ken,
I’m pretty sure no one is bored by the questions. If they are, they can lurk or log-out, right Ron?;)
OK, let’s go through your questions:
1) For Nd:YAG,when the fiber enter the pocket un-initiated, the laser removes bacteria / debris (Does the laser de-epithelialise without initiation? How?).
Yes the FRP Nd:YAG de-epithelialises w/o any “initiation” whatsoever. In fact, if it is unitentionally done or the Hot Goop (protein accumulation) Effect starts in, or the fiber end is scuffed or damaged, we cleave to get as clear and clean a bare fiber as we can.
The “how” of it is just a matter of physics.
CW diodes, even in gated diode mode, can only reach mathematical “peak powers” of 10’s of watts. And that’s with an un-initiated fiber.
Free-running pulsed Nd:YAGs (or erbium YAGs or Er, Cr, YSGG for that matter) have peak powers in the 1,000’s of watts, but they are only “on” for 100 millionths of a second (if the pulse duration is 100 microseconds(usec). At 20 Hertz that means there are 50,000 pulses at 100 microseconds in a second. So that would mean for every 100 usec at 20 Hz, there is 49,900 usec “off” time. That’s what gives high intensity (heat), but for a very short time, AND with nearly a 500 fold time period for the tissue to cool down.
So at 4.00 watts (average power), 20 Hz, 100 usec = 2000 watts per pulse (peak pulse power), but for only 100 usec. Then because the laser is “off” for he next 49,900, the average power calculates out to be 4.00 Watts.
So it is the high intensity, for very short periods of time, that cause the vaporization, denaturation thresholds to be rapidly reached and accomplished, and then a relatively long period to cool down before the next 2000 watt blast comes along to do it again.
It is because of this pulsing that result in rapid heating followed by cool down, that requires the operator to move a lot slower than someone who has used a diode. You have to allow the pulses to do the work, NOT the edge of the fiber.
It is very much non-tactile in the beginning like with the Er; YAG and the Er, CR, YSGG
Then the fiber periphery gets clogged up with these proteins helping to remove more tissue and debris but there is a temp increase ( not as much as a hot glass effect ).
That’s right.
Think about what an 800 degree C object does when submerged into something that in 48 degrees C. I call it “quenching”. It is an immediate and constant transfer of heat from the fiber to the tip o the tissues that have little chance to cool down.
2) An un-initiated diode can only do biostimulation , coagulation ; and surface decontamination ( no sub-surface decontamination as the intensity is low.
High enough power produce heat stacking effect causing bacterial decontamination BUT collateral tissue damage.Yes, that’s about it…….
Bob
(Edited by Robert Gregg DDS at 4:16 pm on July 3, 2004)
Robert Gregg DDSSpectatorQUOTEQuote: from Dan Melker on 10:49 pm on July 2, 2004
David,
I know I can’t get in trouble for this statement. Today, Bob Gregg and I were talking about remaining calculus with the Periolase. Bob said Cobb found up to 50% remaining calculus after debridement yet high degree of success.
Bob certainly can back up what he says. I have always thought all calculus must be removed for regeneration and in fact have failures when I reenter procedures where calculus was left. However the calculus was not detoxified. Really interesting because potentially it could totally change the way we treat perio disease.
If Bob you read this, I am still unclear how reattachment occurs through the calculus so we now have regeneration.
Thanks alot DannyHi Danny,
Perio people who are smarter than me, and have read the literature in great detail have given me some insight why the inability to achieve complete removal of calculus still results in new attachment.
I have been told that in the abense of bacteria, calculus is basically Hydroxyapatite! If there is a way to decontaminate the bacteria (and there is some evidence from the UMKC/Cobb studies that FRP Nd:YAG can and does), then we can see re-atachment “over, through, and around residual calculus. I’ve been told there are human histo studies that show PDL growing through un-infected/dis-infected calculus???
But I have ALWAYS said, I think it is CRITICAL to remove as much calculus as possible. But the amount needed may vary from patient to patient depending on their response to bacterial challenge, and our ability to lower the critical threshold for that host.
That’s why we often include as part of the purchase price for the PerioLase, an EMS Piezon 400 Master piezo electric power scaler.
I have been using the Detectar now for several weeks. I am recently amazed at how much the Piezo gets off on the 1st pass–as determined by the Detectar–about 90%. My next pass or two (with different tips) seems to get all but the calculus “smear layer”, and calculus chunklets down in the 10mm+ defects–as determined by microscopic visualization and the Detectar. Those deep ones need extrra attention or possibly a Detectar.
I’m pretty impressed with David’s assessment of the diode wound heal. Thanks for sharing that perspective Dave. (I think it worth a free Piezon Master 400 with your September purchase:cheesy: )
Bob
Robert Gregg DDSSpectatorFor Danny:
I finally got around to opening up this case to inspect the mesial as to why there was not radiographic and clinical fill as there was on the distal–AND to give Danny the physical and photographic evidence he wanted that the radiographic appearance of bone was indeed bone.

Pre-Op x-ray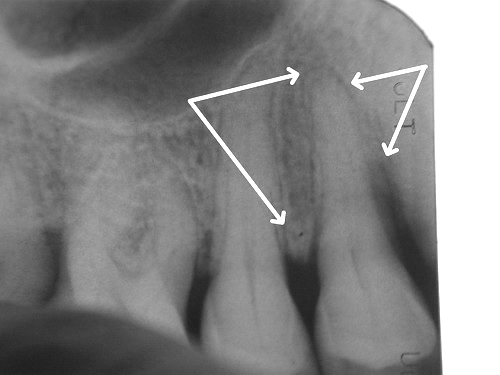
9 month post op x-ray. Bone fill on distal seems evident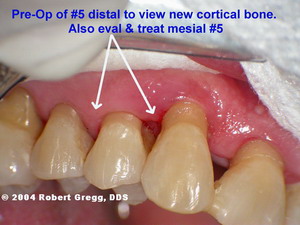
Pre-op photo before raising an envelope flap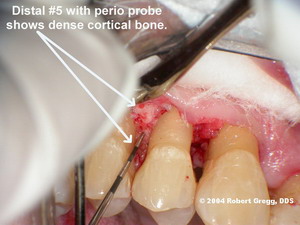
Probe in place. Cortical bone is rock hard and very pronouncedBone to the buccal had a “peak” of bone pushing up.
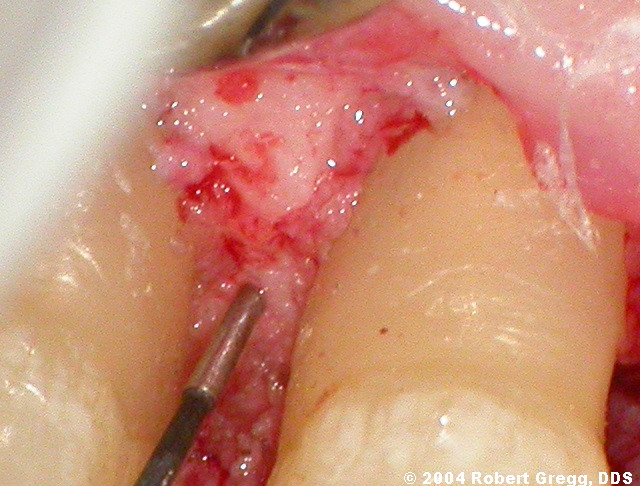
Hi Res of distal areaI have many more pictures of this case both of the mesial and the distal, but this addresses the question of photo-documentation of bone fill.
Thanks for your patience.
Bob
SwpmnSpectatorImpressive. At a minimum deserves it’s own thread – suggest Hard Tissue procedures. Ideally, this case should be formally presented to the dental scientific community.
Perhaps the lack of osseous deposition on the mesial is related to the root groove/concavity on the mesial of maxillary premolars? I’ve heard some periodontists call this “God’s only mistake”.
Just a question and not meant to be critical. On the pre-op radiograph there appears to be caries on the distal of tooth #6. Was this area restored, I can’t tell from the post-op radiograph? Reason I ask is I’m convinced sub-gingival caries contributes to periodontitis.
Presentation was for Dr. Melker but couldn’t resist some comments on what appears to be an important finding.
Al
dkimmelSpectatorBob,
Pretty cool. You do have to tell the rest of the story about what happened on the mesial.David
whitertthSpectatorBob,
Awesome stuff I mean awesome…Thanks again for sharing….
Dan MelkerSpectatorBob,
This comes as no surprise to me! We discussed this case awhile back and I knew what you were going to get.
Al, early on I thought Bob would have a problem with #5 mesial because of the concavity as you said. That is why I like to reshape these areas.
Back to Bob! Way to go and keep going. In your case a picture tells a million words!
Thanks for your incredible contributions to Dentistry!
Danny
Robert Gregg DDSSpectatorThanks Ron, Dave, Allen and Danny for the kind comments.
I have been holding on to this case for a few months due to having a few things with MDT and my practice to deal with (like training 4 new clinical staff members!!). But I wanted to at least get the bone picture proof up for Danny.
I have a whole series on this case for the mesial and the distal. How I flapped it, inpsected it, what I found, what I feel confirmed my initial impression when I first saw the failure on the mesial. I will post the entire case after I get some time to label and resize–maybe in the hard tissue thread.
I think it important to point out that the mesial failure is a rarity in the LANAP protocol, but if there is to be a failure, this will be one place that is a good example as to why. It is a mistake of inexperience, not root concavity per se–completely preventable which is why we use it in our training of what NOT to do.
Since the published success rate of Laser ANAP in private practice in the AGD article is 95%, what I feel is important to show is that we have a strategy to prevent typical early mistakes, understand why they happen, and when they do, how to treat them.
Anyone who does perio therapy knows about “asymetric” healing. Laser ANAP has that too. If I were to suggest otherwise, I would simply be putting out BS.
But the reasons for our asymetry is much easier to isolate since we are very simple in what we do to manipulate the tissue in the protocol.
Iwould also like to point out on the Hi Res photo, that there is clearly residual calculus present. Not for one minute do I think the distal is any cleaner than the easier accessable facial. Something appears to render the calculus less toxic (the 1064nm wavelength?) that perhaps is creating a more hospitable environment?
But this is not unique to lasers or Laser ANAP. Charles Cobb in the Annals of Perio in Mechanical Instrumentation cites Johnson and the paradox of perio pocket healing even in the presence of 50% residual calculus. What may be unique is the nature of the heal–cementum-mediated NA vs long JE.
Allen,
Always appreciate your questions. The distal of #6 was treated shortly after to remove decay and in fact perform RCT. It now has a temporary composite restoration and endo fill.
Thanks for the positive comments everyone.
More later……
Bob
(Edited by Robert Gregg DDS at 9:58 am on Oct. 28, 2004)
-
AuthorPosts
