Forums › Erbium Lasers › General Erbium Discussion › Laser treated pulp exposure on a buildup
- This topic is empty.
-
AuthorPosts
-
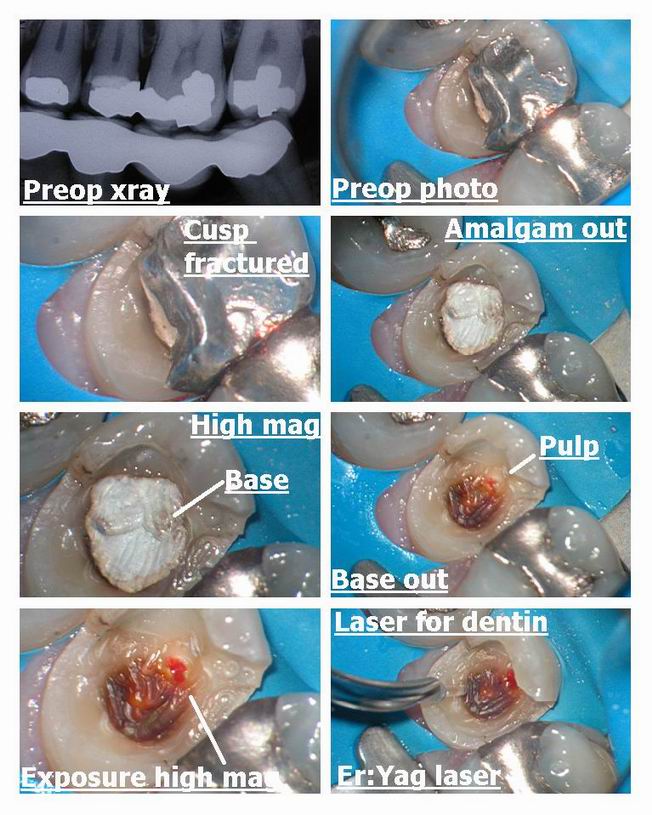
Glenn van AsSpectatorHI folks: here is a case I did today that will stir up some emotion I am sure.
Its why the scope is so crucial for helping me document cases and communicate with patients and why you never know when something simple will come back to bite you.
I was doing a core build up on this premolar where the linqual cusp fractured. Got the amalgam out and found alot of old base which I hate leaving behind. Guess what I found under the base……old decay left behind and an exposure which started bleeding after I got the base out and it was a vital exposure. I read in wavelengths this abstract so I decided to try it.
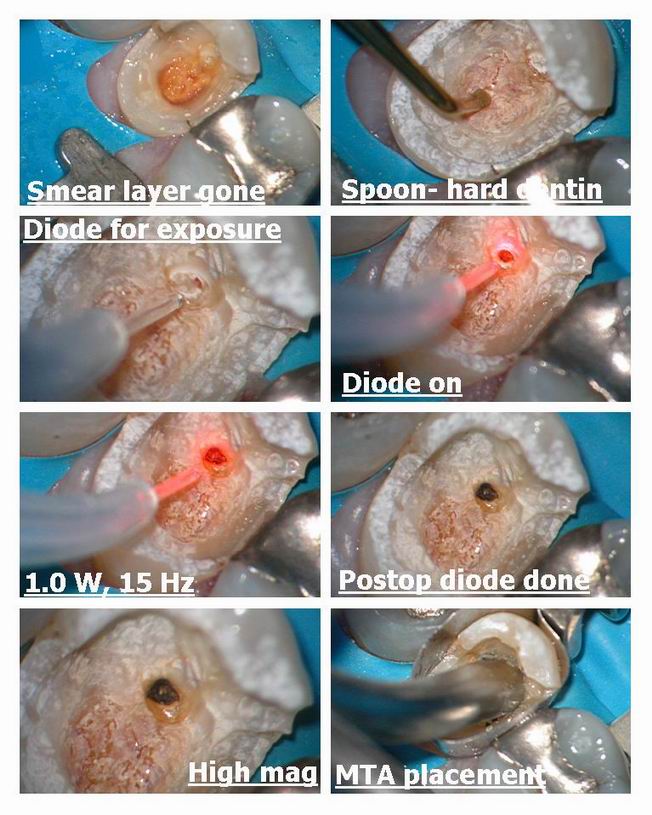
We used the erbium yag to remove the decay and smear layer on the dentin and then used the diode to help with the exposure. The bleeding stopped within a minute prior to using the laser.
Erbium yag on dentin was 30 Hz and 100 mj with H20 and air.
Diode was 1.0w 15 Hz without water and a gentle stream of air.
I used the diode because I was afraid of causing more bleeding with the erbium on the exposure.
Patient felt a little with the diode he said (very minor) and then we placed MTA over the exposure , used a very slightly moist cotton pellet to clean it up and then placed flowable Dyract overtop of the MTA and then the Buildup was done in tetric flow and tetric ceram.
Post op and preop films included and we will wait for 6 months to evaluate pulp which in this study stayed vital 90 % of the time after 6 months and was stable. Look at what the pitiful success rate was for Dycal.
Hope it raises some eyebrows, and I have found the MTA has set in other cases which I have used the laser on and then placed MTA overtop with flowable but I am open to suggestions on how to handle this. I still dont feel comfortable with total etch of the pulp as often it starts to bleed again.
Here is the study……..fire away , I got my flame retardant suit on.
Glenn
J Clin Laser Med Surg. 1999 Apr;17(2):69-75.
Dycal versus Nd:YAG laser and Vitrebond for direct pulp capping in permanent teeth.
Santucci PJ.
Center for Advanced Dental Education, St. Louis University, St. Louis, Missouri, USA.
PURPOSE: To determine the efficacy of laser-assisted direct pulp capping by comparing the survival rates of permanent teeth treated with Nd:YAG laser and Vitrebond (3M Corporation, St. Paul, MN) direct pulp caps to permanent teeth treated with the traditional calcium hydroxide direct pulp cap over intervals of up to 54 months. SUMMARY BACKGROUND DATA: While there are case reports and evaluations of various laser techniques in the literature, statistical studies comparing the success of laser-assisted applications to traditional techniques are needed. This is a retrospective investigation of one such laser assisted application. METHODS: A retrospective chart review of all active and inactive patients resulted in the identification of 83 patients who received direct pulp caps in a total of 93 permanent teeth; 29 with calcium hydroxide and 64 with Nd:YAG laser and Vitrebond. RESULTS: Life table analysis of the data of this retrospective study demonstrated that the teeth treated with the laser and Vitrebond direct pulp cap showed significantly greater survival rates than those treated with Dycal direct pulp cap over intervals of nine to 54 months postoperatively. The cumulative proportion of teeth surviving postoperatively for the Dycal (L.D. Caulk Corporation, Milford, CT) direct pulp cap was 89.7% at 1 month declining to 79.4% at 3 months and 76% at 6 months and then continued to decline in the final two intervals finishing after 54 months at 43.6%. For the laser and Vitrebond direct pulp cap the cumulative proportion surviving stood at 98.4% after 1 month, declining to 93.8% at 3 months and 90.3% after 6 months but then held steady in the final 2 intervals finishing at 90.3% after 54 months. CONCLUSION: The laser and Vitrebond direct pulp cap produces a significantly more predictable pulpal response after the first 6 months than the Dycal direct pulp cap. The survival rate of teeth treated with the laser and Vitrebond direct pulp cap is significantly greater than those treated with the Dycal direct pulp cap over intervals of 9 to 54 months. Direct pulp capping is a worthwhile procedure that should be performed when indicated, especially in light of the 90.3% survival rate achieved with the laser and Vitrebond direct pulp cap at 54 months.
PMID: 11189978 [PubMed – indexed for MEDLINE


Robert Gregg DDSSpectatorHey Glenn,
Time will tell. Wait and see. The pulp looks large enough to have enough ability to recover and lay down a calcium bridge. How about the apical canal space. Juicy or restricted?
What was your reason for using the diode for the pulp cap after the erbium? Was there blood flow? A concern over contamination?
Just curious as the erbium would decontaminate, but yet not stop a bleeder, and yet close proximity would open up your exposure even bigger……wjich you wouldn’t want to do.
Bob
Glenn van AsSpectatorHey Bob : great to hear from you again…….
Good point about the pulp space…..he is a young guy.
I wonder about the apical canal space and the widen ligament space but you saw it was vital and there was no pain prior to me starting (asymptomatic).
With the erbium a couple of problems. One it will widen the exposure and no coagulation so I was worried about bleeding starting again. Yes the erbium could decontaminate but I couldnt get it as close to the site as with the diode.
I often on cases like this will cut the crown and cement it was tempbond for a year or two and reevaluate pulp test and also PA along the way.
If it goes then I will do the endo after removing the crown.
Watch the public outcry on Dental Town…….hehehe
Glenn
whitertthSpectatorGreat stuff glenn!!!! If u remember i did something similar a while back with an exposure…cauterized ( mine with the waterlase) and etched and bonded nad we are at 6 months so far…so who knows with this stuff…maybe we r onto something….As far as MTA I have never used it although have heard about it….can u enlighten me on when u use it etc…….Thanks again
AlbodmdSpectatorThis isn’t specifically laser literature, but it’s some literature comaparing MTA and Portland Cement (which is a lot cheaper) that I copied from DentalTown.
Regards,
Al BMTA vs. Portland cement–the literature speaks:
1:Aust Endod J. 2003 Apr;29(1):43-4.
A comparative analysis of Mineral Trioxide Aggregate and Portland cement.
Funteas UR, Wallace JA, Fochtman EW.
The purpose of this study was to compare the composition of Portland cement and
Mineral Trioxide Aggregate (MTA). Samples of MTA and Portland cement were
analysed for fifteen different elements by inductively coupled plasma emission
spectrometry (ICP-ES). Comparative analysis revealed there was significant
similarity except there was no detectable quantity of Bismuth in Portland
cement. Quantitative results are given in both parts per million (p.p.m.) and
wt%. It was concluded that there is no significant difference between the 14
different elements in both Portland cement and MTA.2: Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003 Apr;95(4):483-9.
Cell and tissue reactions to mineral trioxide aggregate and portland cement.
Saidon J, He J, Zhu Q, Safavi K, Spangberg LS.Objective. Mineral trioxide aggregate (MTA) is being widely used for root-end
fillings, pulp capping, perforation repairs, and other endodontic procedures.
MTA and Portland cement (PC) have many similar physical, chemical, and biologic
properties. PC cement has shown promising potential as an endodontic material in
several studies in vitro and in vivo. The purpose of this study was to compare
the cytotoxic effect in vitro and the tissue reaction of MTA and Portland cement
in bone implantation in the mandibles of guinea pigs. Study Design. Millipore
culture plate inserts with freshly mixed or set material were placed into the
culture plates with already attached L929 cells. After an incubation period of 3
days, the cell morphology and cell counts were studied. Adult male guinea pigs
under strict asepsis were anesthetized, during which a submandibular incision
was made to expose the symphysis of the mandible. Bilateral bone cavities were
prepared and Teflon applicators with freshly mixed materials were inserted into
the bone cavities. Each animal received 2 implants, one filled with ProRoot and
1 with PC. The animals were killed after 2 or 12 weeks, and the tissues were
processed for histologic evaluation by means of light microscopy. Results. There
was no difference in cell reactions in vitro. Bone healing and minimal
inflammatory response adjacent to ProRoot and PC implants were observed in both
experimental periods, suggesting that both materials are well tolerated.
Conclusions. MTA and PC show comparative biocompatibility when evaluated in
vitro and in vivo. The results suggest that PC has the potential to be used as a
less expensive root-end filling material.3: Braz Dent J. 2001;12(2):109-13.
Healing process of dog dental pulp after pulpotomy and pulp covering with
mineral trioxide aggregate or Portland cement.
Holland R, de Souza V, Murata SS, Nery MJ, Bernabe PF, Otoboni Filho JA, Dezan
Junior E.
Considering several reports about the similarity between the chemical
compositions of the mineral trioxide aggregate (MTA) and Portland cement (PC),
the subject of this investigation was to analyze the behavior of dog dental pulp
after pulpotomy and direct pulp protection with these materials. After
pulpotomy, the pulp stumps of 26 roots of dog teeth were protected with MTA or
PC. Sixty days after treatment, the animal was sacrificed and the specimens
removed and prepared for histomorphological analysis. There was a complete
tubular hard tissue bridge in almost all specimens. In conclusion, MTA and PC
show similar comparative results when used in direct pulp protection after
pulpotomy.
Glenn van AsSpectatorExcellent stuff Albert, and I mean it.
I hear that the MTA is sterilized and that is it and otherwise it is PC.
I havent used the white stuff yet , apparently it handles differently and also may not set as well.
I only use a small amount out of the 100 dollar package, per patient.
It is tough to handle (like sand really) and I try to mix it dry.
Joe Dovgan makes a set of three pluggers called the Dovgan pluggers which are nice carriers and in different sizes. I will look to see who supplies them.
MTA I use mainly in perfs, or in large open canals which dont calcify over with CaOH. It also has been shown by many to be effective in pulp caps as it is biocompatible.
Some use it in apicos as well as the root end filling material.
You can get it from Dentstply and it is expensive. The powder you just mix with water , and in addition it is a little tough to handle the first couple of times you use it.
Cya and thanks
Glenn
ASISpectatorHi Glenn & Bob & All you other Keeners
In use of the diode to pulp cap, are you in contact or near contact to coagulate the exposure?
Thanks again.
Andrew
2thlaserSpectatorGlenn, I have been using Messing Guns for delivery of the MTA. They have very small orifi for delivery, mainly for use in apico’s, but I have found it very useful in placing MTA in cases like you have above. Great stuff.
Thanks for sharing this stuff. I need a scope, just need the $ for it first (wife thing!!).
Mark
Kenneth LukSpectatorHi Glenn,
I did a similar case recently.
Patient ( Female, 20 )attended with fractured mesial lingual cusp.Carious exposure after amalgam removal.

Coagulated exposure with 980

Placed MTA on the area.

I have an endodontist at my office and he was advicing on placing a very thin layer of calcium hydroxide over the MTA (to be safe to ensure MTA sets hard). He was saying that sometimes the MTA does not set rock solid. He tend to check the MTA on a second visit at times when the exposure is large.
(He was saying that the MTA does not set well on acidic condition. Also MTA requires some moisture to set.)
No photo showing calcium hydroxide placement.Photac fill ( compomer) lined the cavity
To avoid futher tooth fracture, Crown prepped and troughed with 980 ( 1w cw )
Impression


Troughed margin 1 wk post-op

Crown fitted




She experienced no symptoms during the week.
She was also made aware of possibility of future RCT.Ken
(Edited by Kenneth Luk at 4:51 pm on July 16, 2003)
(Edited by Kenneth Luk at 4:53 pm on July 16, 2003)
(Edited by Kenneth Luk at 5:00 pm on July 16, 2003)
ASISpectatorHi Ken,
Nice treatment. What setting did you use to coagulate and was it noncontact or contact?
Andrew
Glenn van AsSpectatorHi Andrew: I am near contact but not in contact to coagulate.
Maybe a mm away.
Mark as for the scope……I was reading PPAD from JUne and two great articles about scopes in there and some of the endo stuff is phenomenal.
Doing a review for a paper for Journal of Esthetic and Restorative Dentistry on photography with the microscope due out soon……..
Lots of stuff coming out now and many people quietly emailing me to tell me they are planning on putting one in their office and thats how it started with lasers didnt it.
Once you are bitten by the bug, its hard to not think about it.
My wife went balistic all those years ago with the scope.
I was ready to get out of dentistry, I hated all the failures I had with 2.5X loupes be it endos, crowns etc.
I know working at higher mags made me a much better dentist , but my wife mentioned to me the other day,
“…….enough toys for you, how about a new house for me”
She is right too…….i have had a huge amount of fun and enjoyment from dentistry the last 5-6 years……..man what a ride.
Cya and looking forward to seeing you in August , and hopefully you can come by our humble abode and see the scopes and lasers.
He Kenneth……..CLAP CLAP CLAP…yes the MTA will not set sometimes and in my experience pus and blood arent that great but thats in my hands.
I covered up the MTA with Dyract flowable overtop. Then etched etc.
Good ideas and thanks for a great case.
Glenn
Cya
Glenn
Kenneth LukSpectatorHi Andrew,
Coag 1w cw with irrigation non contact. This is the first time I tried with cw. Normally, with gated pulse.
Ken -
AuthorPosts
