Forums › Laser Treatment Tips and Techniques › Hard Tissue Procedures › Osseous Surgery- Open Flap
- This topic is empty.
-
AuthorPosts
-
Glenn van AsSpectatorHi folks: I took some time to go to Danny’s great surgical perio restorative course with Bill Strupp and it really was fun to be there. I think I learned some stuff as well.
Hack2 , Andy and Danny have preached surgery with or without lasers in an open flap environment and here is a case I did today that required osseous surgery. I have the three of them to thank for any successes and of course me to blame for any mistakes.
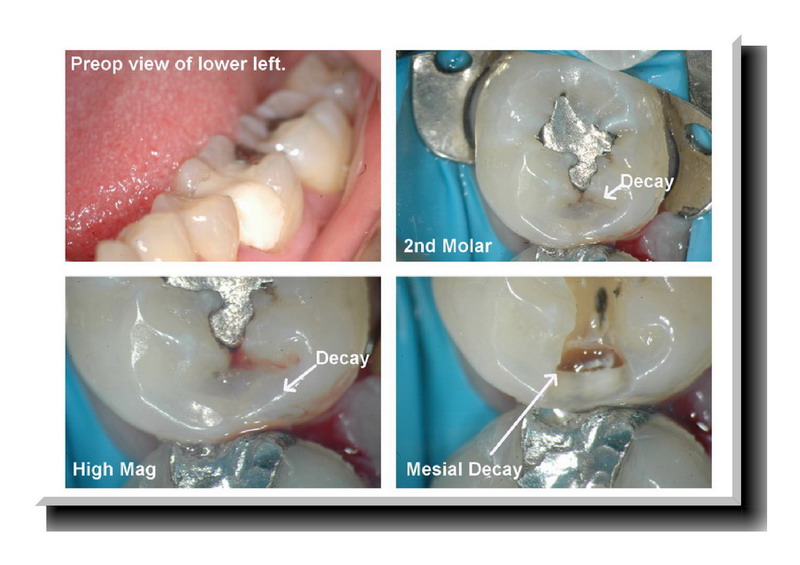
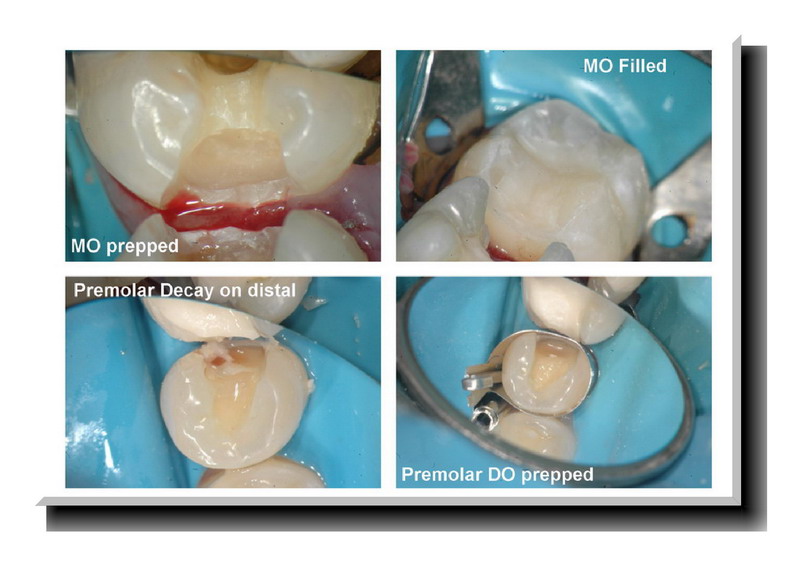
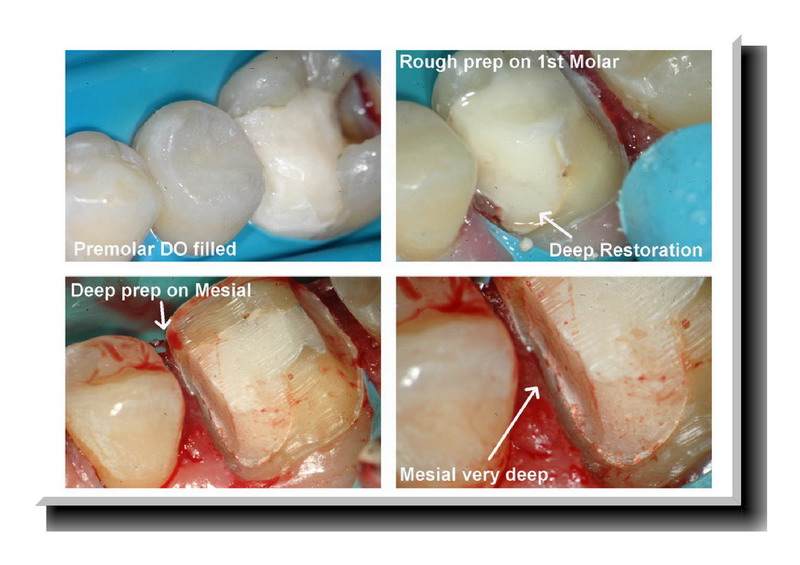
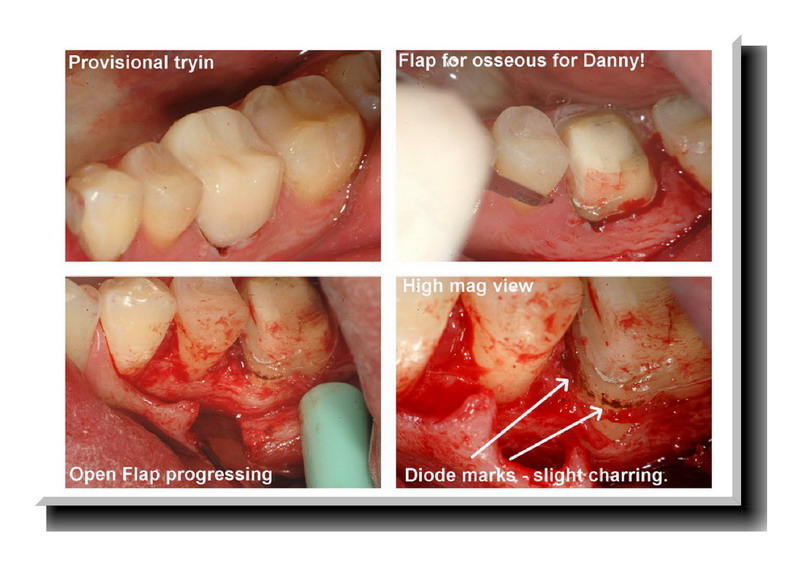
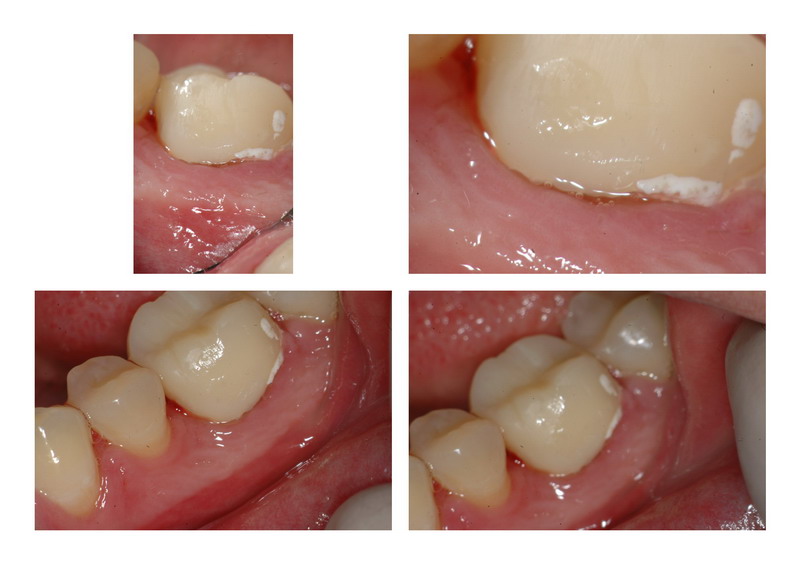
In this particular case (having seen some of Bill Strupps work) I am trying to do more quadrant type work. I did an MO on the 2nd molar and a DO on the premolar with direct resins. Then in Dannys course I learned to temporize first so I then prepped the first molar and this tooth had the need for osseous on both the mesial and mesial buccal line angle of the tooth.
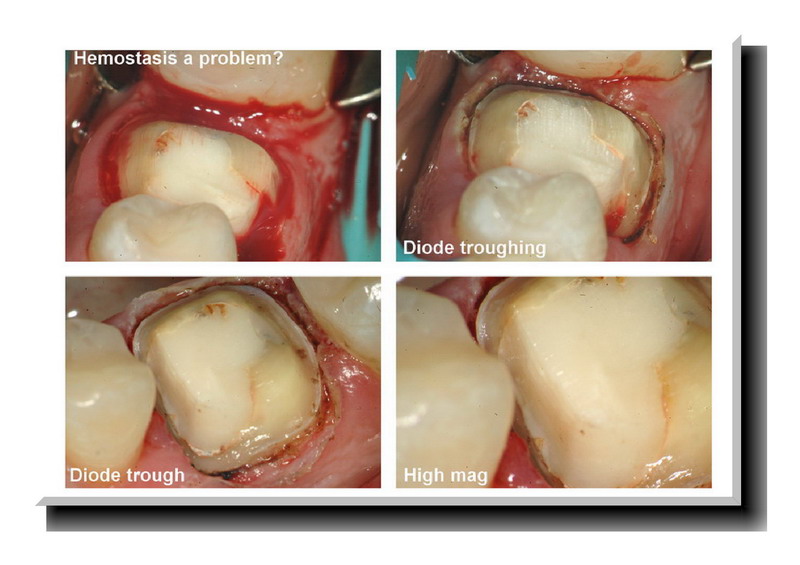
If its multiple surfaces or multiple teeth I find visualization with open flap and the laser for surgical bone removal to be the way to go. After prepping the tooth for the crown you could see how deep the mesial was so I used a diode at 1.1w Continous Wave to get some hemostasis and then made a provisional crown. I flapped the case with a microsurgical blade and proceeded to raise a fairly minimal flap. (The endodontics for this case was done by my associate who has since left but did a decent job not perhaps getting to the end of the distal root quite perfectly).
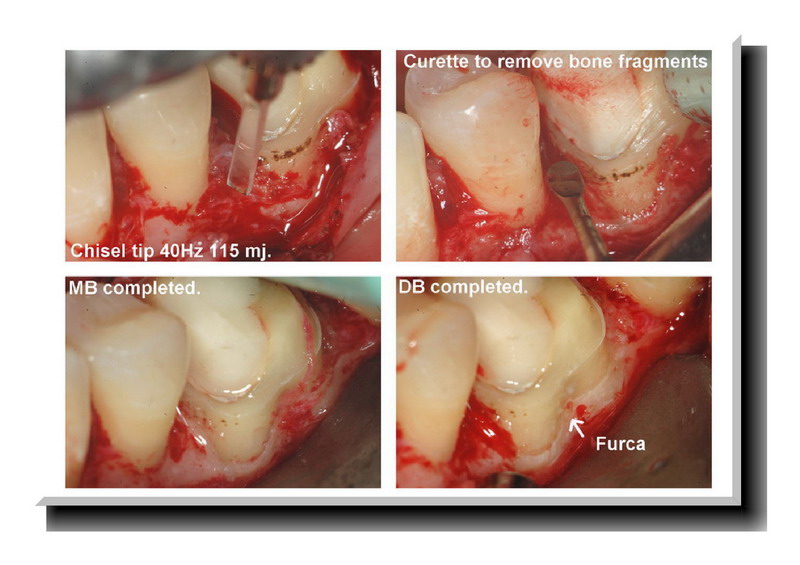
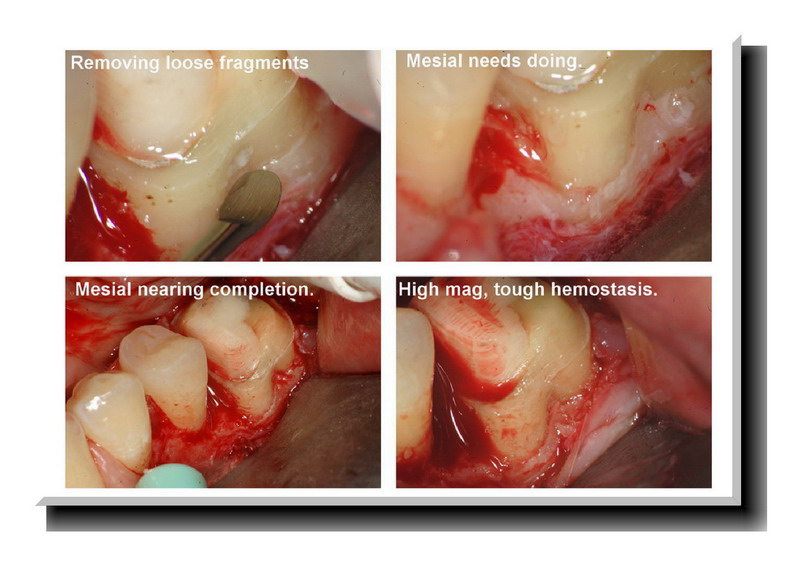
Osseous took place first on the MB root, then on the DB root and finally on the Straight Mesial which was more difficult from an access standpoint. I used a chisel tip at 30 Hz and 140 mj and 40 Hz and 115 mj. The 400 micron tip with alot of water at 50 Hz and 30-40 mj. This smaller tip has the propensity to create vertical defects if not used at very low settings. It will pluck the bone. I use hand instruments to remove bone fragments and finally if you want you can try ultrasonics to remove tissue or bone adhering to the root.
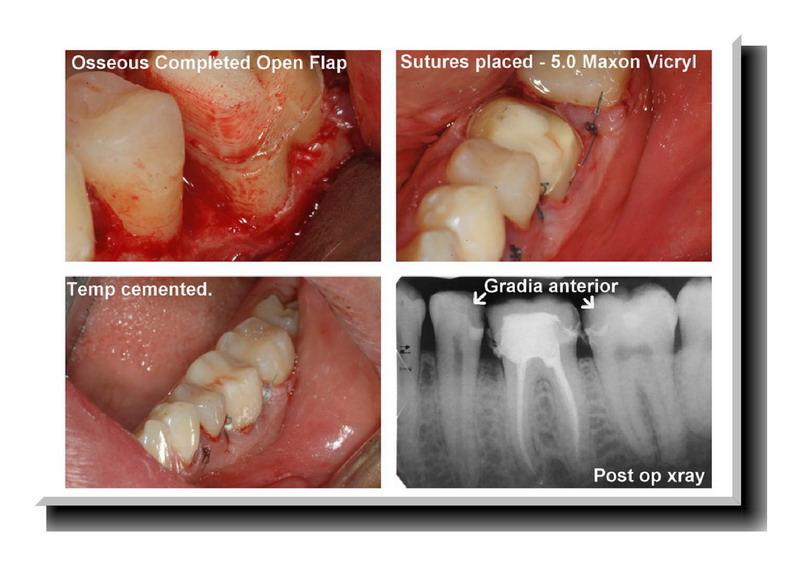
I closed the case with 5-0 vicryl sutures interupted (Hollywood sutures as Danny likes to call them) and then cemented the temp with ZnPO4 because I didnt have Durelon or the cement Danny prefers (Darn it all forgot which one that is).
It took me 2.5 hours to do the whole case and I know its a long time but I needed time to think it all through.
I hope that its of interest and again I can handle some constructive criticism on anything you see that I should have done better. The buccal was easier to do then the mesial which was tough to create the parabolic ,and flowing contours that Danny likes.
Anyways, hope its interesting.
Glenn
SwpmnSpectatorThe thing I like about you is you have the you know whats to take a course, go home, perform and photograph the procedure, then post it for the whole world to see!!!!!!!!
I’m not a fan of Closed Flap Laser Crown Lengthening and in my opinion this is the manner in which erbium lasers could be utilized – as an adjunct to an open procedure. Have only done a SINGLE similar procedure so I’m no one to comment. A suggestion would be you might have considered a little bit more “unroofing” of your buccal furcation.
What flowable composite did you use as your initial layer for composites on the adjacent teeth? I like the radiopacity. Only thing I don’t like is the radiolucency of the Gradia anterior which you are obviously pointing out.
Nice job man!!!!!!! I’ve learned so much over the years from the stuff that you are never afraid to post!
Al
Glenn van AsSpectatorHey Allen……I learn as much from posting these cases because so many people show me stuff that I would never be able to figure out.
I actually did two crown lengthenings yesterday but only 1 with the laser, the other was a lower left third molar buccal…….YA WHAT FUN THAT WAS……..NOT
I dont mind closed flap and am starting to figure out when to use it , and really am gathering some nice case results now.
As for learning, alot of it came before the course actually because Danny, Hack2, and Andy were patient (well sometimes) with my mistakes and I am starting to get a little bit better. I have now done over 60 osseous procedures and I am feeling alot better about it.
Allen , maybe in Canada it is a little different , not so litigious. In addition the confidence the scope gives you is another factor.
I made a mistake with the Gradia as it was supposed to be posterior and not the radiolucent anterior. The flowable was either Matrix from Discus (Dont think so) or more likely the one from Caulk Dentsply that they also make in a hybrid.
Cant remember the name of hand.
Finally Al, thanks, your friendship over the years and good nature fun to keep me grounded has helped me begin to see why I do these collages.
Hope all is well in Florida and that we get a chance to share a beer, and a laugh again soon.
All the best
Glenn
lookin4tSpectatorI like what you’re doing..and I’m not sure I want to see my cases mag’d that high.
One comment-DB of the molar-I’m sure you smoothed it in a later photo, but notice what the end cut of the chisel tip creates in that area that you smoothed out later. A little divot-may be easier to smooth is out with something that is not solely end cutting…..you’re doing very nice work however. As I said, I’m not sure I want to mag my work that high

Glenn van AsSpectatorThanks Lookin4t, I think your cases would look far better especially in the suturing department. I agree that you have to think alot with end cutting only devices.
Its alot of work not having side cutting and some divots do get created.
Hope all is well in sunshine land……off to Charlotte to Nash tomorrow.
Cya
Glenn
lookin4tSpectatorYou’re suturing is fine here…and suturing any “nicer” than that wouldn’t mean anything in terms of healing.
In addition, I’m not sure what benefit getting fancy in this area of the mouth you get..other than spending more time to get the same result and have a prettier picture.
Lee AllenSpectatorGlenn,
Thanks for posting this case. Classy.
I am trying to work out the power densities you used on the bone. What is the area of the chisel tip? I have noticed the groove making with the smaller tips, also. The larger diameter/area tips are the best solution.
Great photos. Makes me feel like I was there.
Glenn van AsSpectatorHi Lee: I am constantly changing my ideas based on what I find closed flap going to open, and open flap plus what Danny and Lookin4t and also Andy advise.
In general for open flap
Chisel tip is first at 40Hz and 110 mj or for higher energy 30Hz and 140mj with lots of water , and little or no air.
Chisel tip is 400 by 1200 microns (I think) or its 400 by 800. I think it is the former not the latter.
For the 600 micron tip 50Hz and 50mj or 40Hz and 60-70mj or 30Hz and 70-90mj
For the 400 micron tip 50Hz and 30 mj, 30Hz and 50 mj.
HOpe that helps and check out these 2 week healing photos of the case I did above when I took out the sutures on Monday.
Glenn

Lee AllenSpectatorGlenn,
I am revisiting this post because I have done some (dozen or so) crown lenghtening using the open technique, and while I enjoy the results find that it is so time consuming, I am beginning to wonder if there are some shortcuts. Any tips that you have run across?
I like the “fat” tip for osseous even though it takes more water to make less charring, which if it occures relates to post op pain, but it is very slow. How high can an Erbium power density go and still be atraumatic?
Is the angle significant? I am beginning to think that it is in addition to the parallel to the root concept. Perpendicular to the boney surface seems to work well but in a tiny area. Slow slug (slimy giant snail without shell for those not bless with these garden creatures) march across the osseous area to reduce then becomes the working mode. An angular approach is necessary when feathering out the reduction further under the flap (I use a periosteal elevator wide end to protect the flap and reflect and stray beams) and it goes even slower.
My conclusion is that I need different calculations on power settings for my tips or different tips. I refuse to change machines, so do not even go there. I am using the S and C series tips for the Waterlase “Classic”.
Any thoughts on power settings in Watts? I converted your settings by watts=mjoules*Hz.
Glenn van AsSpectatorHi Lee: great to hear from you again and I have some final photographs of this case that I should post if I have time.
One thing that I have found in doing open flap surgery is that I am not as gentle handling tissue as I could or should be. I also am not as good with sutures. Some of my results have been great, some pretty average. I have found that I get better results on those areas where I can do closed flap crown lengthening (I know Danny will kill me for saying that) where there is one surface on one tooth (for instance margin location for deep subgingival preps) compared to some of my open flap cases.
I have a huge amount of respect for the way Danny does surgery now because I cannot seem to get the esthetic results that he does.
As for Erbium crown lengthening open flap there are a couple of things that I do…….these are just ideas so use them as much or as little as you want.
First off it is slower than a bur so if you have a torus or something to remove you should look at cutting a trough
and then sectioning the large piece off.For crown lengthening I find that the bigger the footprint of the tip the better. I use a chisel tip that is 1200 microns by 500 microns with a ton of water and not much air. I then go to smaller tips with lower settings so as not to pluck the bone away.
I use hand instruments to smooth the bone (small spoons) and then use ultrasonic scalers around the teeth to remove fragments of tissue or bone.
Now having said this I typically am not doing large amounts of bone as it just is too slow in my hands.
Settings wise it depends on the tip and water flow.
typically
Chisel tip might be 30-40Hz and 100-150 mj so 3-4 watts.
600 micron tip 30-40 Hz and 80-100 mj (2-4 watts)
400 micron tip 30-40 Hz and 30-80 mj (1-2 watts)These are just ballpark figures and should not be relied upon for all people as I use the scope and will vary my settings alot on what I see happening at the bone site where the laser tissue interaction is taking place. Higher settings for cortical bone, lower for marrow.
Watch vertical defects so I keep moving reasonably quickly to again avoid plucking or vertical iatrogenic troughing.
As for angle ,yes it is important to vary the angle of attack to not get a vertical trough. Subtle movements changing the angle of attack and higher levels of magnfication help because it is a non tactile thing.
I know Mark Colonna has developed some C tips which have a bigger footprint (I discovered this in the brochure I just got from Biolase) and these Ctips (Colonna chisel tips) are around 1200 by 500 microns and 6mm long I think.
In any event I hope this helps but I am still playing with things and my closed flap cases sure do heal up nice.
I will post some if I get a chance after November 3-5th when the AMED meeting is over.
Glenn
etienneSpectatorHi Glenn
I really appreciate the fact that you post your complete settings with your cases, not just “use the setting for crown lengthening” or something!! In order for somebody to understand what is going on during the procedure the full settings are indispensable.
Take care
Etienne
Glenn van AsSpectatorHey Etienne , thanks for the kind words. I am in NY right now and lecture on Tuesday then it is off to Dubai for a day or two.
I will post a case soon on here with closed flap once I get healing photos. It looks ok and I had a specific reason for doing it.
Gotta run but thanks for the kind words
Glenn
Andrew SatlinSpectatorWow Glenn,
Somehow I missed this case. Great job. Interesting how the slight mesial inclination of certain teeth can make these cases challenging.
I have started incorporating some more root reshaping on cases like this–thanks to Danny. Have you tried it yet?
I love the way you ramped the osseous from the furcation without opening it up. Thats textbook. You know what else works well, is if you “flute” the buccal and lingual interproximal areas. Like the old denture wax ups? That little bit of osteoplasty helps the interprox tissue tuck in really nicely.
Anyway, these cases are probably old news to you by now!
Really nice work as always!
Andy
Glenn van AsSpectatorHi Andy: I still manage to do some closed flap and some open flap cases. I did a closed flap the other day on the lingual of a lower 2nd molar which needed one -2mm of reduction of bone and there wasnt much hope with this patient (not easy to work on) of reflecting a flap and getting access there, so I did a closed flap.
I will post it if I have a chance. I still dont find my surgical skills to be above average. I wish I had the energy and time to spend on courses to improve on that , and to be honest , I firmly believe that is one reason why I dont do more open flap cases is because I lack the surgical skills to be above average at them.
I have never done a root reshaping case but I think Danny knows or thing or two on how to handle some of these tough cases.
WEll gotta run, next patient is here and thanks so much Andy for the kind words. Even the older cases are fun to revisit every once in a while to see what I did then and how I would handle it now.
See ya
Glenn
Andrew SatlinSpectatorGlenn,
Lower 2nd molar areas can be intimidating. Unfortunately they often require considerable osseous recontouring on people with thick biotype. They are also very challenging on uncooperative patients becasue of the obvious access problem and the strength of the tongue.
You really should pursue the root reshaping treatment (with all that free time on your hands!). Because of your restorative experience I bet you would find it easier than I did. Tissue ends up healing fast and really nicely!! Less ostectomy required also. The fancy periosteal sutures and the CT grafts that Danny does in conjuction with crown length is a separate issue.
You are too hard on yourself. Your surgery looks great!
Keep in touch
Andy
-
AuthorPosts
