Forums › Diode Lasers › General Diode Forum › Treating Peri-implantitis with 980
- This topic is empty.
-
AuthorPosts
-
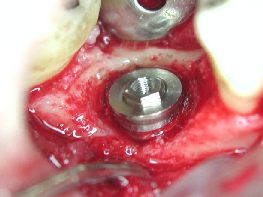
Kenneth LukSpectatorPatient returned for stage 2 implant treatment symptom free. A pin hole sized pus was draining on the ridge.
CONTAMINATION!
Flap was opened and granulation tissue was all around the implant. The implant has already osseo-integrated.
All infected tissue removed with 980 under saline irrigation. At the deepest bone level, the implant surface was lasered circumferentially.
Area infected limited to under 2 polished threads of 3i implant, no bone augmentation done. Flap closed with healing abutment.
After 4 weeks, impression taken and crown cemented.
Ken(Edited by Kenneth Luk at 11:03 pm on June 4, 2003)
Kenneth LukSpectator



Hope the photo sizes are ok
Ken(Edited by Kenneth Luk at 2:00 pm on June 5, 2003)
ASISpectatorHi Ken,
Nice crown-tissue interface and emergence profile. Looks as though it is a natural crowned tooth.
Andrew
Robert Gregg DDSSpectatorNicely done Ken!
Bob
Andrew SatlinSpectatorHi Ken ,
Interesting case. Peri-implantitis is probably my least favorite scenario to treat. I place a fair amount of implants.
I am curious why you chose the laser in this situation as opposed to plastic curettes. Risk of heating or modifying the surface.
Also, for those not familiar with implant uncovering, I wanted to point out that the degranulation should always be completed with the cover screw on. The picture shows it removed.
Last, I am not a fan of biomaterials but it looks like an ideal case to collect some bone from the surrounding area and graft the exposed threads. No membrane or synthetics needed.
Most importantly, It appears to be placed well. I bet it will continue to be a very successful case.
See ya,
Andy
Glenn van AsSpectatorVery nice case Ken……great pics and a nice result. You have the handpiece with the water in it dont you.
What settings did you use , for how long.
Glenn
Kenneth LukSpectatorHi Andy,
Plastic currettes would have been quicker at removing the granulation tissue. I just wanted to try this out using the 980 as Biolitec was saying that the implant would not be damaged.
The cover screw was in place during tissue removal.
Yes, it would have been a much better solution to cover the threads with autogenous bone. How much longer will I have to wait if I were to place the graft?
Your comments are most welcomed!
Ken(Edited by Kenneth Luk at 1:35 pm on June 16, 2003)
Kenneth LukSpectatorHi Glenn,
I used the irrigating handpiece with cool sterile saline dripping along the 400nm fiber to the tip.
8W on 0.05s/ off 0.05s
Granulation tissue removed circumfrentially, slight contact trying not to blacken the tip of the fiber ( 2 min ).
As I got closer to the implant , the fiber is moved more quickly so as to further avoid any heat building up on the surface.
Ken(Edited by Kenneth Luk at 1:58 pm on June 16, 2003)
Andrew SatlinSpectatorHi Ken,
So many variables if we are discussing bone grafting.
Many implants are placed as single stage these days so you do not even get the opportunity to see that scenario before it is restored.
In your case, because the implant is integrated I might wait 4-6 weeks. Honestly, a couple of exposed polished threads wouldn’t bother me at all.
On the other hand, no news is good news when it comes to implants. Implants in my experience that become symptomatic in any way are much more likely to fail.
I have placed a few hundred fixtures so I am no authority on the subject but from the pictures you showed it looks like the cover screw may have loosened slightly and allowed the infection. Cleaning it out is the best thing to do.
Keep us all posted.
Andy
Kenneth LukSpectatorHi Andy,
I’ve not placed as many implants as you’ve done.
I was worried of contaminating the area again if I were to place bone graft. So I opted not to.
I guess it would either be contamination on the cover screw before suturing or as you said, loose screw. It didn’t feel loose when I unscrewed it after degranulation though.
Thanks for your input!
Ken
Kenneth LukSpectatorA paper was published in J. Periodontal 2000;71:810-815
Effects of Diode and Nd:yag laser irradiation on Titanium Discs by Romanos, Everts and Nentwig.
Titanium discs were irradiated with 980 at 5.0, 10.0, 15.0W (cw). disc was irrdadiated using a contact handpiece with a 400um fiber held perpendicular to thedisc surface for 5 sec. Surfaces were irradiated by a linear movement of the fiber, with linear areas 3mm apart.
Irradiated areas were compared with control titanium sites which were not lased. Examined under SEM.
It was concluded that the 980 does not damage titanium surfaces.
Author noted that Temp changes on titanium was to be studied.
Ken
ASISpectatorThis is not surprising as at 980nm, the chromophores are hemoglobin, oxy-hemoblobin and water in the tissue. Metal is non absorptive at 980nm. Thereby it is quite safe to use this wavelength around titanium.
Correct me if I am mistaken.
Andrew
ASISpectatorExcept for the thermal aspect of course. Much like other metal restorative materials.
Andrew
Robert Gregg DDSSpectatorHi Andrew,
Near-infra-red wavelength laser are transparent through water, and has no absorbption (or extremely weak–say 40+mm) in the water in the tissue. That includes 810-980-1064-1500nm. I know some folks say 980 is highly absorbed in water, but I strongly disagree in spite of the charts that have been used to support the proponents arguements.
We have held 980 up to a zip-lock bag of water, and fired the beam into an infra-red camera–NO attenuation was detected by the camera. If 980 was highly absorbed, the camera could not have detected ANY light. Imagine shining a 1064 to a black piece of paper or baggie of black ink with a near infra-red camera–nothing would get through to the camera.
Biologic interactions with live human tissues are VERY complex. In fact, once the tissue is “hit” with a laser (or electrosurgery) it is NO LONGER the same viable tissue constituents that you started with. So what is being interacted with at that point? Heat altered proteins.
The measurements and data collected by some investigators are looking at DEAD tissue and lab experiments that do not necessarily translate to live human tissues.
When we get water to BOIL in our patient’s tissues using near infra-red lasers (not erbiums), it is secondary to absorbption in another substance (the hot glass of the “activated” fiber) or tissue components (blood pigments or other tissues, or proteins).
Human tissues are VERY tolerant of the abuses we impose on them. The “heat sink” (the ability to dissipate heat quickly to body temperature) is great in the area around the implant due to the thickness of bone. There is a limit to that heat sink, but one would have to deliberately hold the fiber in one place for too long with these lasers.
Bob
(Edited by Robert Gregg DDS at 10:49 am on June 19, 2003)
ASISpectatorThanks, Bob.
There is so much more than the simplified electromagnetic spectrum chart that shows different absorption of chromophores, isn’t there?
Andrew
-
AuthorPosts
