Forum Replies Created
-
AuthorPosts
-
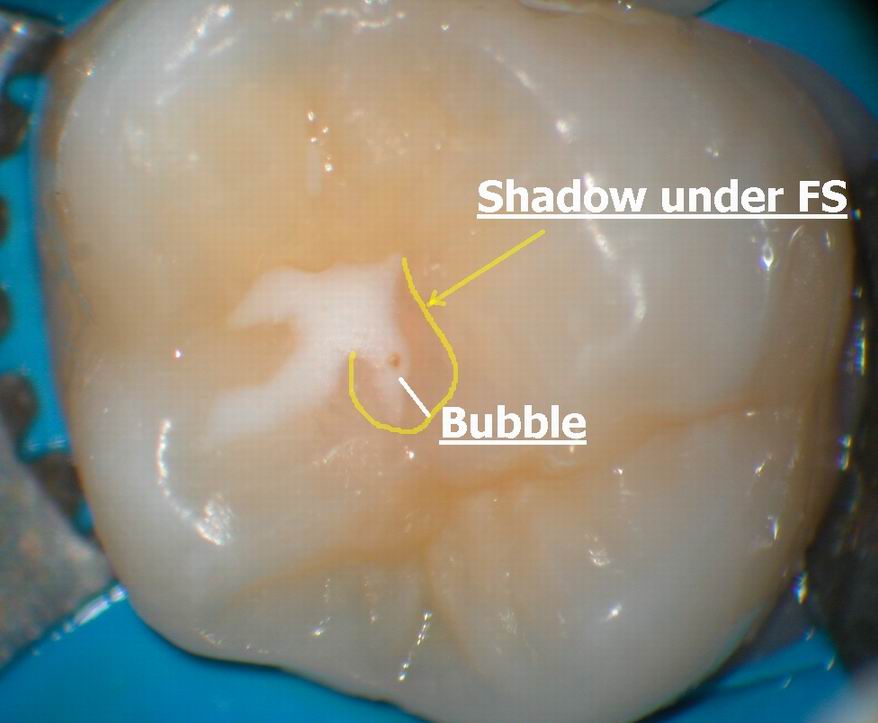
Glenn van AsSpectatorHere is a magnified image of what I saw but you must remember that the microscope image is much clearer than this, but hopefully it gives you an idea of the shadow and the bubble. I see this lots with the scope.
Glenn
ASISpectatorHi Glenn,
Another impressive statement for scope use in dentistry!
Andrew
Andrew SatlinSpectatorRod,
Laser dentistry is very new to me. I do however have alot of experience in periodontal surgery. Crown lenghtening or any preprosthetic surgery in the esthetic areas are particularly challenging. I am still unclear about your technique and your rationale. It seems that you : 1- performed 2-3 mm of laser gingivectomy
2- used a probe / explorer for blunt dissection into the connective tissue attachment
3-ablated the connective tissue with the laser
4-gingivoplasty with diamond burs
How does this create a new sulcus? could you have accomplished the same procedure with a 15 blade and a diamond bur?
Aren’t you just violating the biologic width and alowwing the periodontium to heal on its own?
I am not an expert on wound healing but it seems that if you did not leave enough space for epithelium, connective tissue and sulcus depth then the periodontium will reestablish its natural biologic width via attachment loss.
Cases like this one with thick tissue may be very forgiving. Others may not be.
I do not mean to sound critical. I am always looking for better ways to preserve papillae and obtain adequate crown lenghth.Andy
mickey franklSpectatorThank you all for your coments.
Marc, I went to your lecture in London last week and was very impresed!
You definitly know and Love your Laser.
I hope to learn from you and the rest of the experianced laser users after I get my own laser.
Thank You all
MIckey
London UK
Andrew SatlinSpectatorBob,
Laser dentistry is very new to me but as a periodontist I can tell you that if aggressive ostectomy is required, particularly in the interproximal area, conventional flap surgery is indicated. As you mentioned, it is important not to leave negative architecture. Also, don’t forget to evaluate root morphology, root proximety, length of root trunk/location of furcation and overall thickness of the periodontium. I firmly believe that lasers are have important roles in the future of dentistry. We still should not throw out the basic rules we learned about proper oral health.Andy
dkimmelSpectatorThe fustration with this premolar at the start of the thread was a big deal for me. The second patient Tooth #31 was going to be seen the next day. This patient was allergic to all anesthetics and if numbing with the laser did not work, I was going to have a tough time. This was a long term patient of mine that had just developed an allergic reaction to the anaestheics. She is also one of the big reasons I bought the laser. I was really relived that it worked. She is also a reporter for the St. Pete Times. She showed up with a photgrapher. Since it worked it turned out fine. It could have been bad if it had not worked.
It was a great ending. Woke up this morning with a call from one of my staff. We made the front page of the Pasco section. It was a pretty good article. She left only one small thing out of the article. My name. What a hoot. I had even talked about Allen and the closest other laser to me. Sorry Allen your name did not make the article but at least she put what town you were in. So you made out a bit better then I did.
What a hoot. Well at least the laser worked!
David
AnonymousInactiveMark,
I read with enthusiasm your posts on this endo case. Great job! What a pleasure it is to see the renewed excitement with lasers in dentistry.
I don’t want my comments to dampen your excitement or your desire to try new and varied techniques that will expand the knowledge of lasers in dentistry – but, there are a couple of technical concerns that might be considered when using an Erbium laser as the last instrument on the internal walls of the root canal. In the August 2002 issue of Journal of Clinical Laser Medicine & Surgery an article was published that I believe would be of interest here. The article, on page 215, is titled “Effect of Nd:YAG and Er:YAG Lasers on the Sealing of Root Canal Fillings.” The study was performed in Brazil so the translation is missing a couple of words along the way but you can get the drift of the message. I have included a few of the salient points and would be happy to send you a copy of the entire article if you request.
In the interest of better lasers in dentistry…
ABSTRACT
Objective: The ability of the laser irradiation to promote the cleaning and disinfection of the radicular canal system has become this type of treatment in a viable and real alternative in endodontics. The purpose of this study was to evaluate the apical marginal sealing of root canal fillings after the irradiation with the laser of Nd:YAG or of Er:YAG. Materials and Methods: Forty-two human, extracted single-rooted teeth had their crowns sectioned and the root canals prepared with a no. 70 K-file. Then, they were dried and divided into three groups according to canal wall treatment: group 1: the canals were filled with EDTA for 3 min, followed by irrigation with 1% sodium hypochlorite solution; group 2: the canal walls were irradiated with Nd:YAG laser; and group 3: the canal walls were irradiated with Er:YAG laser. Afterwards, the root canals were obturated by the lateral condensation technique. The roots were externally waterproof, except in the apical foramen and immerged in 2% methylene blue aqueous solution during 48 hours. Results: The results showed that the largest infiltrations happened in the group 3-Er:YAG (7.3 mm), proceeded by the group I-EDTA (1.6 mm) and by the group 2-Nd:YAG (0.6 mm). The group Er:YAG differed statistically of the others (p < 0.05). Conclusion: It was concluded that the Er:YAG laser intracanal irradiation previously to the root canal filling must be used with caution until future research is define the best parameters for it's use.
(A piece of the) DISCUSSION
The results of this research shows that group 3 (Er:YAG) presented higher mean and statistically significant infiltration levels, when compared to the levels of the other groups (Table I and Fig. 3).
It was expected that a lower infiltration degree would be observed with the use of Er:YAG laser, since it promotes exposition of the dentin tubules, removal of the smear layer, with increase of dentin permeability.10,11 These observations would justify a better marginal sealing of the root canal obturations after the use of this laser.
Although the Er:YAG laser does not promote the melting of the dentin neither the closure of the dentinal tubules, it causes a reduction on the dentin layer due to the ablation process, forming craters and consequently a rough surface with great irregularity as described by DostAlovd et al.,12 who observed a decrease of the dentin layer in cavity preparation with the use of Er:YAG laser. Besides that, during the ablation process, the dentin is not vaporized, and can be dislodged to other areas, including to the apical region, making more difficult the adherence of the obturation material to the root canals walls.Address reprint requests to:
Dr. Marcia Carneiro Valera
Av. Dr. Francisco José Longo, 777
Faculdade de Odontologia de São José dos Campos-UNESP
Caixa Postal 314
Sã José dos Campos, SP, Brazil
CEP 12201-970
E-mail: mcvalera@iconet.com.brAgain – I appreciate your enthusiasm for lasers!! I wish we had had these resources available to us 14 years ago when I started. What a benefit they are and how much faster we will learn and better our procedures will be as we learn together “Lasers in Dentistry.”
Delwin McCarthy
AnonymousInactiveAndy,
How did your training go? Did you get all your questions answered? Your success will depend a lot on the training so that you do not need to “reinvent the wheel” in your search for understanding of lasers in dentistry. There is a lot of good information in this web site.
RodSpectatorHi Andy,
Some very good questions. Many of these have already been answered, but may have been answered on the DentalTown forum or case presentation area.
I’ll ‘quote’ you and then answer each quote below.
QUOTEQuote: from andy on 5:37 pm on April 12, 2003
RodQUOTELaser dentistry is very new to me. I do however have alot of experience in periodontal surgery. Crown lenghtening or any preprosthetic surgery in the esthetic areas are particularly challenging.Yes indeed they are — VERY. It’s easy to do more, but if you get too aggressive the first round, it’s more difficult to ‘put it back’.
QUOTEI am still unclear about your technique and your rationale. It seems that you : 1- performed 2-3 mm of laser gingivectomy
2- used a probe / explorer for blunt dissection into the connective tissue attachment
3-ablated the connective tissue with the laser
4-gingivoplasty with diamond bursFor the most part, yes, but actually #1 and #3 above seem to be saying the same thing — removal of ‘soft’ tissue with the laser.
QUOTEHow does this create a new sulcus?Actually, saying this creates a new sulcus is not exactly correct. What this does is help create epithelial attachment. Above the level of the bone we’re gonna have connective tissue attachment via fibers, epithelial attachment and sulcus. Sometimes the connective tissue fibrous attachment is wider than others. If you start out with a very wide connective tissue attachment, you can usually reduce this width of attachment successfully.
You will commonly find this in cases of ‘gummy’ smiles. In cases like this, often the bone is where it would be even if this patient didn’t have a gummy smile. Whereas the ‘average’ patient would have a narrower band of fibrous tissue, the gummy smile patient may have a much wider band. In a case like this you can reduce the width of the band of firm fibrous attachment without the amount of rebound that you’d expect if you encroached on the bone level.
One key is getting rid of some of those fibers. By severing the fibers, and then use of the laser, you’re more likely to establish some epithelial attachment — whereas if you left that tissue attached via fibers, you’d be more apt to grow more tissue (rebound) to establish the epithelial attachment portion of the ‘biological width’.
QUOTEcould you have accomplished the same procedure with a 15 blade and a diamond bur?Yes, absolutely, and I have many times. But there are two problems with that. One is pain. The post-op pain is quite significant without the laser. The other is that the fibers (which we intentionally sever) are more likely to re-establish without use of the laser. But yes, I’ve done this numerous times with instruments other than the laser.
QUOTEAren’t you just violating the biologic width and alowwing the periodontium to heal on its own?I’m very confused about this question, and unsure of what you’re getting at. I’m certainly taking away some of the biologic width, it that’s what you mean. However ‘violating’ is a different thing. I’d say that ‘violating’ the biologic width would be removing more than you need to have a healthy biologic width. I wouldn’t call removal of ‘excess’ biologic with ‘violating’. Is that what you meant? True violation of biologic width simply doesn’t work — whether or not you use a laser.
However, if the patient starts out with excess biologic width, you can successfully reduce this with and without a laser, although it’s easier with a laser. The main thing is to retain a biologic width that is acceptable.
Before I forget, take a look at the DentalTown case presentation at another case I posted in response to similar questions. It’s a case where I removed a large amount of biologic width over one of the centrals. We could have been more ‘perfect’ by doing a touch of osseous in a couple areas, but this is presented to show a 9 month post-op.
QUOTEI am not an expert on wound healing but it seems that if you did not leave enough space for epithelium, connective tissue and sulcus depth then the periodontium will reestablish its natural biologic width via attachment loss.Huh? Again not sure what you mean by ‘attachment loss’. Are you saying that the biologic width will reestablish itself via bone resorption? In other words, are you saying that if you violate the minimum biologic width, and place restorations to the level of the new gingival margin, the gums will not grow back up, and instead will reestablish via bone resorption? This may very well be the consequence, however there would be a chronic inflammation during this period, which may be more extended in some patients than others. I have found that very slight violations of minimum biologic width are usually tolerated if they occur only here and there, but not if significant areas are involved.
QUOTECases like this one with thick tissue may be very forgiving. Others may not be.Again, not at all sure of what you’re getting at. Are you saying that cases with thick tissue are forgiving, but cases without thick tissue are NOT forgiving? If this is what you’re saying, you’re entirely correct. That’s why I’ve mentioned that we first established where the bone was before deciding what technique to utilize. Given that we started out with an excessive biologic width, to use your phrase, we understood that the case would be ‘forgiving’ and not require osseous.
Or are you saying that some cases of thick tissue will be forgiving, and some cases of thick tissue will NOT be forgiving?
Actually, there was a little more behind our decision making process than meets the eye, and it may turn out that we’ll regret not doing some osseous now. In the beginning, we anticipated doing the cosmetic work on the gums, and then a combination of porcelain jackets and veneers all around. We were to gain some tooth length via reduction of the gingiva, as well as lengthening of the incisal edges in porcelain. Given this scenario, the amount of gingival contouring would have been perfect. HOWEVER, the patient (who is himself a dentist) has now changed his mind and decided to ONLY treat the two centrals. Because of this, lengthening the teeth will not be an option, and even more gingival removal would have been ideal.
As mentioned before, we ALWAYS anticipate growth of some gingiva, and therefore when we do the procedure, we must ‘overdo’ it a bit. We remove epithelial tissue down to the connective tissue. We WILL ALWAYS have regrowth of epithelial tissue over that rather durable connective tissue. So we deal with a ‘controlled’ amount, or ‘anticipated’ amount of rebound.
However, I’ve found that most often the laser will keep the anticipated rebound less than if the laser is not used.
For some reason several have misunderstood the purpose of posting this case — thinking that I am saying that by using a laser, we can successfully violate the minimum biologic width. I’m not sure why some are thinking this. It simply is not true. It is true that the laser will usually control rebound better than similar procedures without lasers — therefore making the procedure more predictable. But violating minimum biologic width? No.
The purpose was to show how such a case looks with a laser as the instrument, as well as to show that sometimes dentists go in and do osseous when they actually could have avoided it.
This patient was treated to remove excess gingiva by a periodontist within a few months before I saw the patient. The periodontist told the patient that to achieve more results, osseous would be necessary. Upon exam, given the apparent width of connective tissue attachment, I had a suspicion that we could have a better result without osseous. However, we were prepared to go either way, depending on how the bone sounding went after anesthetic was used.
I do not know who the periodontist was. I don’t know if he does much of this sort of stuff. I hate to say it, but what went through my mind is that this dentist (the patient) may refer to this periodontist. And because of this, the periodontist may have done this as a freebee for the referring dentist patient. And maybe he just didn’t feel like putting forth the effort to really take his time and go the distance. Maybe, maybe not. It’s not a discussion I really wanted to get into much with the patient.
QUOTEI do not mean to sound critical. I am always looking for better ways to preserve papillae and obtain adequate crown lenghth.OK, NOW you touched on something that is a ‘pet’ of mine — preservation of papillae. I don’t know if I mentioned it on this forum, but I think I did on one of the DentalTown forums. Cracks me up when I read an article where they show how to do cosmetic crown lengthening, and utilize the ‘papilla preservation’ technique. Boy!! You talk about ‘hit ‘n miss’!!
When I do flaps to do osseous, I NEVER use this papilla technique. I make my incision without going into the papilla. Yes, I ‘filet’ off the most facial portion of the papilla, but not even up to the tip, and certainly I don’t go into the interproximal space whatsoever. I do the osseous reduction and apically position the flap. Now I’ve ended up with the papillas extending farther from the gingival margin than when we started. The papilla tips has not changed, but the gingival margin has. In these cases, you never lose a papilla, but most often you need to later go in and do ‘touch-up’ contouring.
Most often you will do some facial osseous, but really don’t need any interproximal bone reduction — but sometimes you do. In cases like that, I do the same approach, but once the facial osseous reduction is finished, if I need to ‘blend it’ into the interproximal, I simply use the Waterlase and remove a little bone UNDER the papilla going into the interproximal. Works like a charm.
Anyway Andy, great questions. Believe me, I’m NOT ‘the authority’ on this. I’ve done cosmetic gingival contouring for about 23 years now — started many, many years before it was ever spoken of in the journals — way before periodontists started thinking about it as a legitimate reason for treatment. So I am somewhat experienced in it, but NOT any sort of ‘authority’ by a long shot. I too am always looking for better ways.
Thanks.
Rod
(Edited by Rod at 12:25 am on April 13, 2003)
RodSpectatorAndy,
Your last statement is a VERY important one, and I’d like to echo it again. I too have found that there are some that feel that because we’re using a laser, we can overcome some of the restrictions of the basics we’ve dealt with for years. And in some narrow applications this will be true.
However it’s important for new laser users to understand that the laser is simply a new instrument, but most often the same ‘rules’ do apply.
You seem very interested in lasers — do you own one yet? If so, which one, and if not, what sort are you thinking about and why?
Rod
Glenn van AsSpectatorDel there are some HUGE holes in this study as I see it. I knew about it a long time ago and Bryan Pope sent me the whole article to read…..
Now if you post the methods you will see how they did this and it was very close to the apex. and they used the laser after they shaped to a #70 and then did not go back and do an apical gauge with any handfiles…..
Geez I wonder why it gave so much leakage.
The power was high I think as well. There were a TON of problems with the way the study was run.
If you use the Erbium Yag laser to help sterilize and disinfect it an be very useful (as seen under the operating microscope ) for cleaning the walls of the canals.
Make sure you always draw out of the canals, always start a minimum of 2 or better yet 3 mm from the apex and draw out 2 mm per second or so.
I know that you love the NdYag and it is a nice laser for this but in my opinion this study doesnt justify not using carefully the erbium yag to clean and disinfect the root canals particularly if used judiciously.
Glenn
Glenn van AsSpectatorHi Andrew: thanks …..
I still dont use the laser exclusively for occlusals (in pediatric dentition I do) because I find that the scatter from the laser makes the prep a little wider than careful use of a small bur.
THe microscope really helps you see what it is that you are doing. Most of the tips are clear (quartz or sapphire) and of sizes that are 400 microns to 600 microns for the erbium and half that for soft tissue lasers.
THe resolution of the human eye is around 200 microns so it does get difficult to see the tip close to the tooth. I see this all the time when I travel as the users at the meetings always have the tip to far away from the tooth.
It wont cut fast then or properly if it is too far away. If the tip is damaged it is also tough to cut well. THe microscope helps in alot of situations but I wont bore the regulars with another speech from the pedestal.
Thanks for the kind words and I have alot of times used the laser to “etch ” very lightly a groove on a tooth to place a flowable in it when another pit on that same tooth is already carious.
Dont know if I am overdoing it but I like the non opaque resins better than FS and they are often a higher filled and many times less bubbles in my hands.
GLenn
Andrew SatlinSpectatorHi Rod-
I sort of always have been interested in Lasers for periodontal therapy. I am a periodontist. Used a CO2 in my residency but was never really impressed.
I recently purchased the PerioLase from Millennium. Still evaluating my results. Very much enjoying the procedures. Trying to learn as much as possible. I call Bob and Del about twice a week to ask about settings and techniques and stuff.Andy
Andrew SatlinSpectatorHi Rod
Thank you for your detailed reply. It seems we agree on many points. A couple of things still need to be clarified.
How do you determine removal of “excess” biologic width vs. violation of healthy biologic width. I have never actually heard the term “excess ‘ biologic width.Re: attachment loss –that is exactly what I was saying. If you violate the biologic width you may very likely get a chronic inflammatory response. I am sure you have seen it over the years.
Re: cases with thick tissue being forgiving. Again you understood my point perfectly. Thick periodontiums are very forgiving.
Re: Papillae preservation–We should probably talk on the phone about this one. I could not agree with you more. I acually use the same technique if I have to get access to bone. I have had minimal success with the “palatal curtains” and the old published methods. Actually, if you look carefully at those newer “cosmetic” crown length articles they are very misleading. I often reccommend orthodontic extrusion in isolated cases. Have you tried that?
Thanks again Rod –talk to you later
Andy
Glenn van AsSpectatorAndy try rubbing the troughed out area with hydrogen peroxide in a Ultradent syringe with the little brush (mop) head on it.
I like that technique for removing the tissue tags and getting loose fragments away from the margin.
I also sometimes use a bur to retouch up my margin and this will also remove some fragments often without bleeding if you are careful.
Try those two things.
Glenn
-
AuthorPosts
