Forum Replies Created
-
AuthorPosts
-
Glenn van AsSpectatorHi Bob………I added a reply in your support……its a shame when information isnt shared with criticism that is constructive instead of destructive.
That is why Rons laser forum prospers……we may not always agree with the treatment or ideas but we have an air here of professionalism and cordiality in the posts.
That is what makes people want to post their cases.
Glenn
Glenn van AsSpectatorPosted on 05/17/2003 by glennvanas Rows | Index
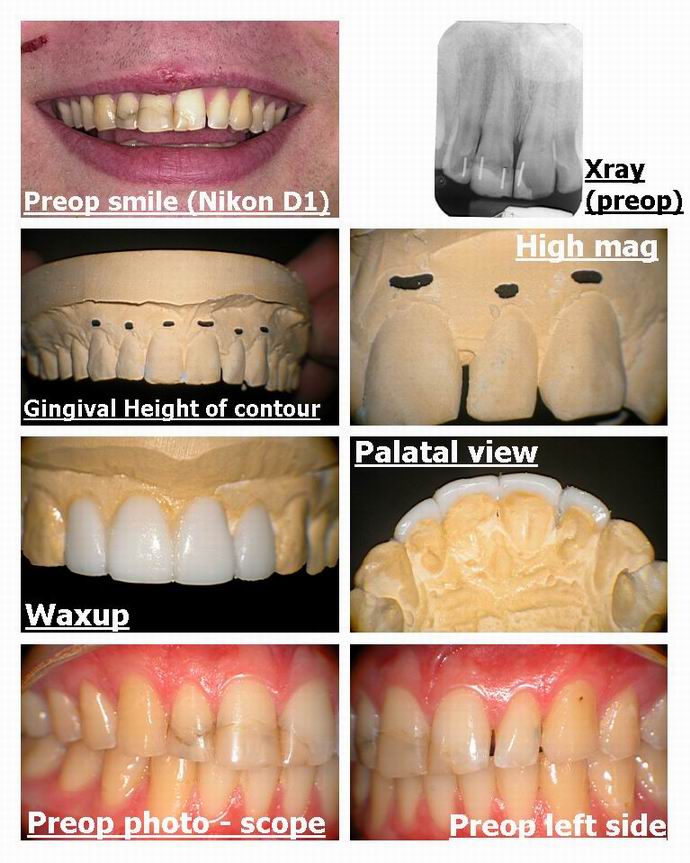
Hi there: Here is a case where were doing some cosmetics for a patient who had a bad fall as a teenager.
Using a Digital SLR camera we took a preop smile (Nikon D1) then moved over to the scope and took some pics of the waxup and study models.
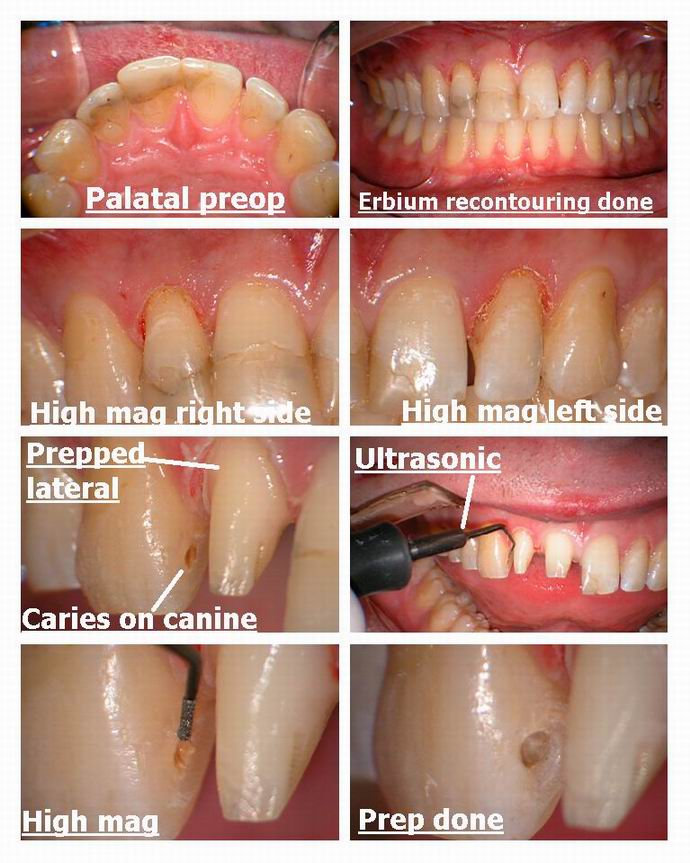
The gingival height of contour was a tiny bit of on the two laterals so we lengthened them after probing (4mm tissue on them) to get them the same height as the centrals. We use the erbium laser to do this.
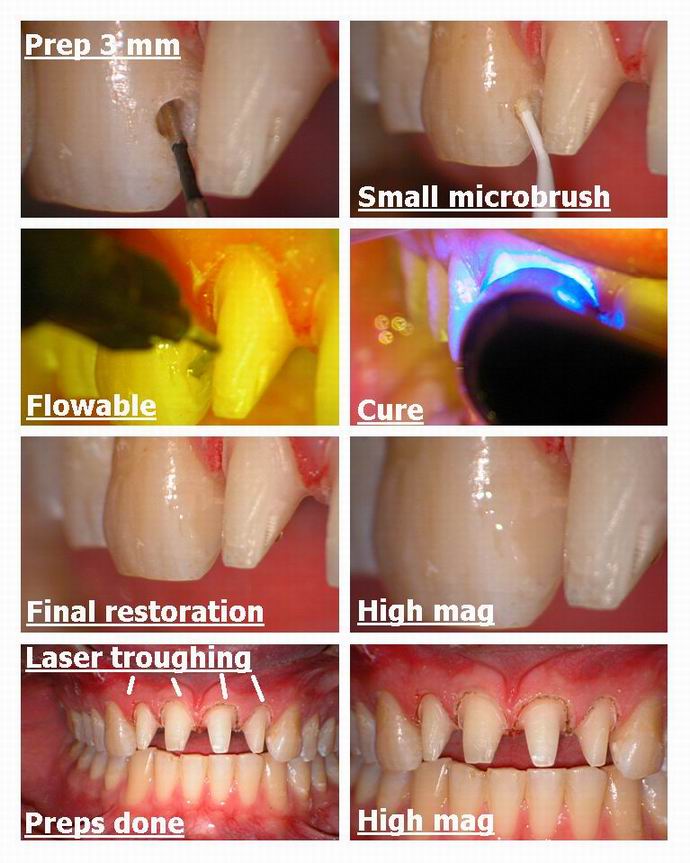
WHen prepping the lateral it was discovered that the mesial surface of the canine had a small carious lesion. I used the Ultrasonic Sheets SL tips to prep this and these are made by spartan obtura.
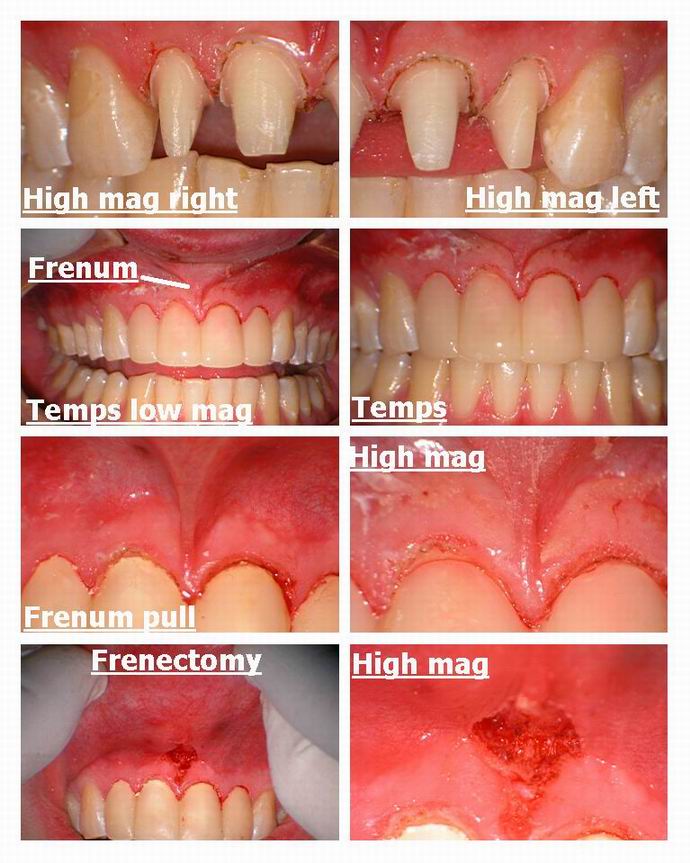
The preps were done and then a soft tissue laser was used to trough the tissue for the impressions.
Temps were fabricated and then we noticed that the frenum was quite thick so it was removed with the erbium laser (hence the bleeding).
These are just alternatives to traditional means and arent meant to be a reflection that cords, burs and electrosurges cant be used.
The whole case was done under the dental operating microscopes we use and the photographs taken through them.
I have over the last 4 years tried to install a high tech “difference” to our office while trying to retain a hi touch as well. Its kinda our practice niche and sometimes people will ask if the hi tech are just for show. We use them all day and in a typical case this is how some of the items might be used. Again dont think that it couldnt have been done in any other fashion.
Glenn
Robert GreggParticipantGlenn,
Thanks very, very much. Your comments were AWESOME. Thanks so much for your support. It helped me a GREAT deal!
I have to admit, I was really overwhelmed by the personal nature of the attacks. I understand now what you have been telling me about your previous Dental Town posts! WOW!
I also want to thank Rod Kurthy for being so incredibly supportive of me as well. I’m am really overwhelmed by the kind words and the time Rod and Glenn took out of your Saturday’s and busy schedules to come to the moral and professional support of a friend.
You guys are TOP drawer!!
Glenn, I agree completely with your assessment of the Nd:YAG as a dedicated soft tissue laser with some limited hard tissue uses. Hard tissue removal is one of the ways to try to distinguish Nd:YAG’s performance from a soft tissue only diode that is not free-running (with all of that emission mode’s advantages and capabilities).
Thanks again for all your support, my friends!
(Edited by Robert Gregg at 10:12 pm on May 17, 2003)
AnonymousInactiveBob, This is a great series of photos that show what we have been doing with the Nd:YAG for many years. New technology not only allows us to see well but to show others what we see. Great post!
Robert GreggParticipantOK Gang,
Here’s the series if you haven’t already seen it. Better images here at Ron’s Forum and a more receptive audience. Sorry about the image sizes Ron–I’m still trying to make adjustments.
Pulsed Nd:YAG lasers are often thought of as ONLY “soft tissue” or periodontal lasers. However, pulsed Nd:YAG lasers have FDA clearance for hard tissue “indications for use”. One FDA clearance is for “enamel caries removal”. That is the removal of organic pigmented debris on and within the pits and fissures of Class I occlusal surfaces. The Nd:YAG 1064 nanometer wavelength is highly absorbed in chromatic pigments whereas this wavelength has very little effect on healthy enamel or water.
The high peak powers that a “free-running” pulsed laser (neodymium or erbium) can generate are powers on the order of 2000 to 3000 watts per pulse for one to two hundred MILLIONTHS of a second (microseconds) allowing the target tissue to reach it’s ablation threshold VERY rapidly resulting in rapid removal of the target substrate/pigment.

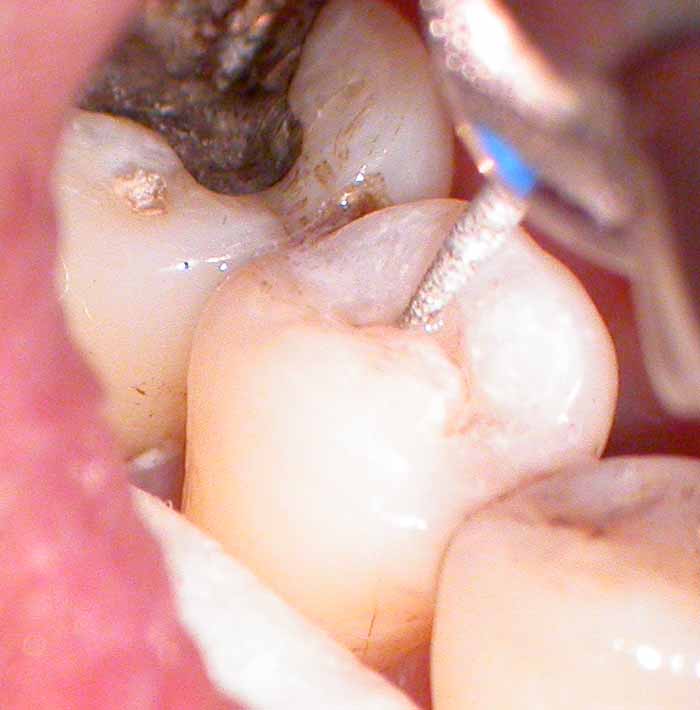
Pre-Op photo of the lower right second bicuspid on a 60 year old female with full compliment of teeth. Patient has stain and organic debris on the occlusal surface, as well as in the pits and fissures. To remove this debris with air abrasion, erbium laser or a diamond or fissurotomy bur before determining if there is decay present, could result in prepping a tooth that only has stain. Air slurry polishers might work nicely to remove the organic stain and reveal any remaining decay. However, having a laser that will selectively remove ONLY the organic stain or decay, and NOT any healthy enamel–and do so in microseconds–and before committing the patient and the tooth to a full resoration is a nice application if you indeed have such a device available.

Pulsed Nd:YAG at 100 microseconds (usec) Pulse Duration, at 3.00 watts of “average power”, 300 millijoules per pulse (mj/p), and 10 pulses per second (Hz) gives the operator 3000 watts per pulse. The stain and organic debris on the occlusal surface acts as an “initiator” or an activating pigment. Not unlike water does for erbium lasers. This was very interactive at this stage. No anesthesia was used. No “painting” of the tooth to create laser analgesia was used. No black suma ink “initiator” was used. No simultaneous water or air spray was used to cool the tooth. The patient was comfortable throughout.

Carbon deposits build up, even at short pulse durations, in the absence of water. Plasma and the ejected vaporized organic debris coat the tooth with a grey colored film. Water was sprayed on the tooth and the carbon was easily removed by lasing the discoloration THROUGH the water, obtaining absorption in the carbon, and preventing oxidation. This is a view into the occlusal pits and fissures.
Selective “photothermalysis” (a favorite term of my laser friend Geza) means I was able to remove the organic debris on and around the pits and fissures, but there is clearly more debris and/or decay present.
The inverted “V” pattern of decay once it hits dentin makes it necessary to remove enamel. The pulsed Nd:YAG will not do this. It will, however, remove decay and dentin if access is available.
So at this stage, the clinician can choose their own preference in accessing dentin and removing enamel–air abrasion, free-running pulsed erbium lasers, fissurotomy burs, etc.
In this case I used a flame diamond to open up the groove. Again, no anesthesia was used and the patient remained comfortable.

Enamel walls opened up, dentin and decay were accessed and removed with both the effect of the diamond and the use of the pulsed Nd:YAG.
Again, no anesthesia or any other effects were needed to remove decay or diseased dentin in this instance.

Tooth after etching with 37% Bisco phosphoric acid.

Bonding agent placed……..

Flowable composite placed, and polymerized with a pulsed Argon laser.
(One of the few contructive criticizms was about my use of a flowable composite. I agree, it is not the best choice for occlusal surfaces, since it is not highly filled. I simply was NOT planning on doing this for the patient as I thought it would only be a stain removal situation.)
Bob
(Edited by Robert Gregg at 10:31 pm on May 17, 2003)
ASISpectatorHi Glenn,
Very nice documentation. Indeed an illustration of a plethora of high tech applications that not only create a successful outcome, but provide an enjoyable treatment experience for both the patient and the clinician.
The WOW factor must be in the exponential for all involved.Andrew
Glenn van AsSpectatorHey Andrew………great seeing you yesterday.
I will post another interesting case in a minute, but once you get the laser and the scope you just keep pushing the envelope to see where it will end.
I pushed one too far recently and had some poor healing under a pontic on a bridge we tried to do immediately.
Dealing with that headache these days but all in all it is a fun time in the office.
ALl the best and give me a call when you get the stuff and I will try to come by and spend a couple of hours with you.
Glenn
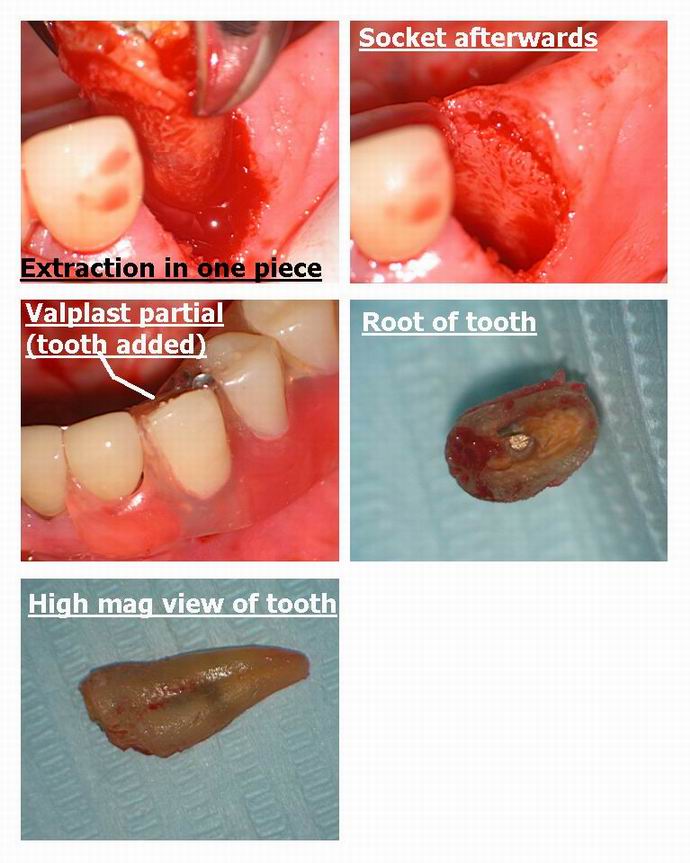
Glenn van AsSpectatorHi folks: here was a case I did the other day for a lady who is in her late 70s.
The tooth had a cast gold post and core and a crown which fractured off at the gingiva and patient was given options of post removal (tough), osseous surgery, possible graft of attached tissue, new post core and crown support her partial denture or..
Extraction and addition of the tooth to her partial with a new valplast clasp on the lateral.
She chose the simpler option and I prepared to extract the tooth.
When the partial came back with the tooth added on, we placed anesthetic and then used the laser to remove tissue around the root ( it had overgrown it) by using the laser at
30 Hz and 80 mj without water (2.4 watts) and then 30 Hz and 100 mj with water for the 3 watts pulsed for bone relief.I was then able to get the forceps on the tooth and roll it out. The socket is clean with no bone or tooth fragments. No flap was needed and the patient left happy happy happy……I got it out in one piece.
Now Mark is doing these exos without anesthetic (grin) but at least I didnt need a handpiece!!!
All the best,
Glenn

ASISpectatorThanks, Glenn.
I think I speak for all when I express my gratitude for all you share.
I really like the way in which you display your photos. The organized and sequential fashion is so pretty and captivating to look at that I find myself revisitng them over and over again.
Like the line in Bugs Life: I can’t help it! It’s so pretty to look at!
Like Mike Swick said a couple days ago: You da man!Andrew
AnonymousSpectatorBob, the images here are much clearer than on DT. You can see the ‘hole’ started in the bi.
Just to be sure I understand, is the area circled in black (below) the area of carbonization (gray,dusty appearing)?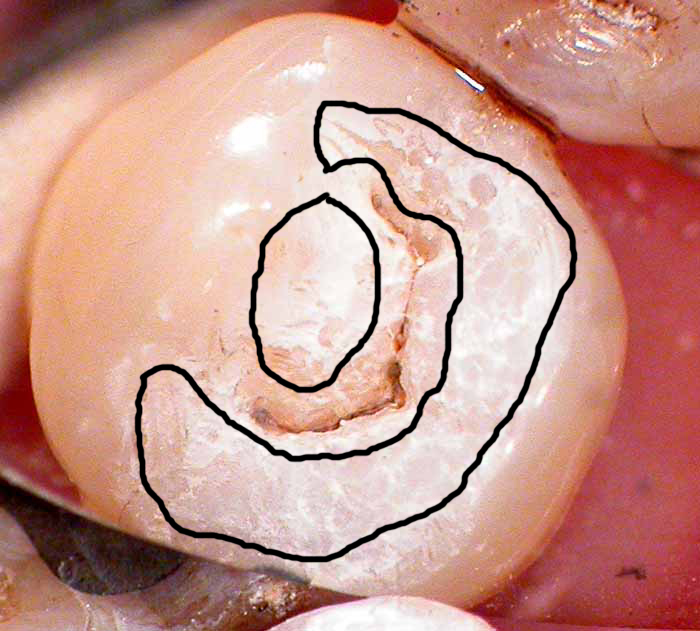
Thanks
BNelsonSpectatorBob
Sorry I missed all the excitement on DT. The negative comments often encountered is one of the reasons I seldom visit it anymore, and would seldom consider posting on it. More power to you. This forum I find much more informative and the caliber of doctors posting much more professional and helpful. Thanks for the great pictures and sharing this case. Isn’t this the exact kind of case that SS White makes fissurotomy burs for, and I have never heard any negative comments in DT about Howard advertising them in the magazine. So what’s with all the crap (excuse the French, Please) with using the laser for the same thing?
Thanks for your usual level of exceptional professionalism and insite in presenting this.
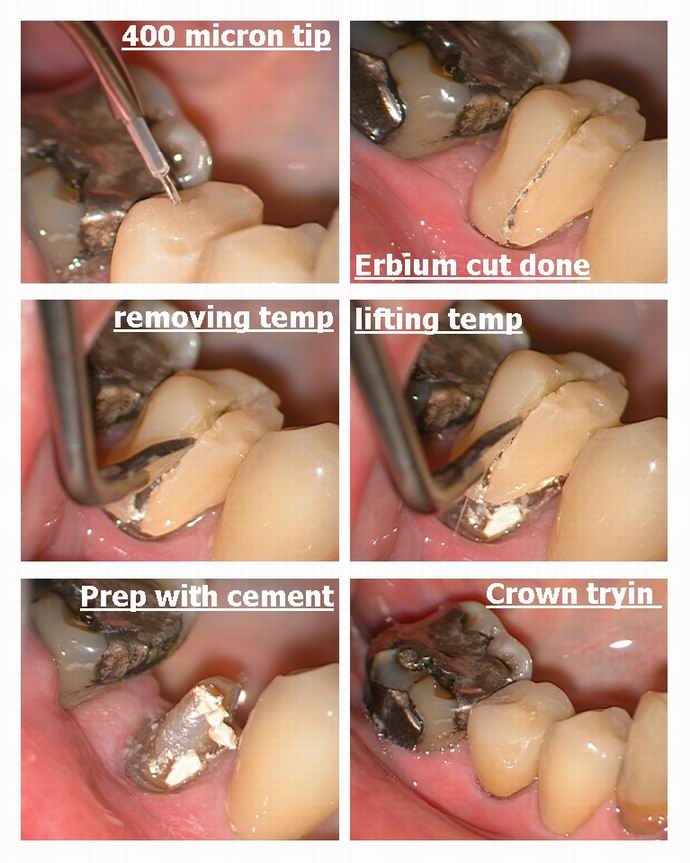
Glenn van AsSpectatorHI folks: every once in a while I get a little worried about pulling a temp crown off and breaking the prep.
SO for this case on an elderly lady (near 80) I used the laser to cut throught the temp. It took a couple of minutes but I was able to lift the temp off without anesthetic and placed on the permanent without anesthetic.
The molar needs doing as well but she only wanted the premolar which fractured to be done.
I used 30 Hz and 140 mj with water and a 400 micron tip to cut the trough.
Luxatemp was the temp………most cut though I think.
All the best……….
Glenn
AnonymousSpectatorThought I’d add a fibroma case also.
5mm diameter
er,cr:YSGG 1.0 W EMLA 11/7Preop


Postop

1 week

Ok, a few questions for you all.
Should I have been more invasive and gone deeper?
In this case after the piece was removed I went back and ‘resurfaced’Biopsy?
Pt could pin point cause from trauma.
Any suggestions?
ASISpectatorHi, Fellow Rons,
Very nice photos. Interesting that there’s no bleeding from the second case. Is that why you think it should be done a bit deeper?
Andrew
AnonymousSpectatorQUOTEQuote: from ASI on 11:44 am on May 19, 2003
Hi, Fellow Rons,Very nice photos. Interesting that there’s no bleeding from the second case. Is that why you think it should be done a bit deeper?
Andrew
Actually, most of the cases I’ve seen posted,here and elsewhere, seem to look like they are more cratered afterward. I didn’t create a crater with this one and was wondering if there is any long term diffrence.
I’ve never had any bleeding to contend with on fibroma removals, just once in awhile on frenectomies.
-
AuthorPosts
