Forum Replies Created
-
AuthorPosts
-
AnonymousSpectatorQUOTEQuote: from Benchwmer on 8:16 pm on May 19, 2003
Is this a WaterLase only topic? If not stated differently I guess we are to assume WaterLase?Only if no other wavelengths get posted 😉
Jeff, I always try to post wavelength rather than brand.QUOTEI thought we were going to give out treatment parameters, tip size, duration, etc. I never see Hertz posted in WaterLase posts, even if it is fixed, it would be helpful in treatment interpretation.Sorry, I left out G4 tip and the Waterlase (er,cr:YSGG )is fixed at 20H. Tx time approx. 1 minute. My fault for posting between patients.
Time for some other wavelength users to post similar cases!
Glenn van AsSpectatorI think that the laser cuts the OH molecule in the resin portion of the material (not the filler) and that is why it can cut the material. This is the VOCO material for temps and I know it cuts that but I havent tried the polycarbonate material with the laser.
Yes Mark Colonna has taught us a thing or two over the months……hes been quiet lately , probably living in Tahiti with all the funds from his great spoons and instruments.
Grin
Glenn
Glenn van AsSpectatorHi Allen………thanks. One thing I have noticed with the erbium is a cleaner socket and less trauma to the bone , tissue and less debris in the socket.
I have done this a couple of times and thats just what I noticed clinically. I got enough root available for the forceps to grab hold of and was able to get a tough tooth out in one piece. You can see the gold post on the last photograph in the root.
It worked well and did so last time too, neat way to take out the root I think.
Glenn
Glenn van AsSpectatorHi Al: the G4 tips are narrow at the end (400 microns) than the G6 tips which are 600 microns and the power density is much greater so it will cut better but remember that these tips can be more sensitive for the patient as well.
Glenn
BenchwmerSpectatorRon,
Here is how it is done with a pulsed, FR, Nd:YAG, contact fiber, 3.0W 20 Hz 110usec, less than a minute.
3 point infiltration, 2% Carbocaine w/ 1/20,000 Levordefrin
Before treatment
Immediately after treatment

two weeks post-op
Robert GreggParticipantHi Al,
I love how you are thinking about this!!
“Is the ability to obtain hemostasis more a function of wavelength or of pulse duration?”
More of pulse duration.
Doesn’t a wider pulse duration invoke a wider band of thermal necrosis and thus achieve the desired hemostasis?
I’m impressed with your analysis. Not quite, but that’s pretty close. With conditioned or initiated fiber tips, yes. With unconditioned pulsed laser fibers with high peak powers, no.
Thermal (coagulation) necrosis is a surface effect of laser wounds. Varying the pulse duration will effect the deeper layers below the surface zone of coagulation/necrosis—the zone of injury or stasis.
A wider pulse duration gives a wider zone of thermal injury or “stasis” i.e. hemostasis—not necessarily a wider surface zone of coagulation or thermal necrosis – unless it is a short pulse duration of a deep penetrating wavelength (1.064).
That’s why being able to VARY the pulse duration we can vary the effects from a surface effect only, or a gradually deeper effect on the zone of stasis to get HEMOSTASIS without necrosing the surface. That’s why the pictures look so un-effected on their surface. They are! And that’s how we are able to get the wet “soft clot” not the dry necrotic wound (eschar) you would see with an initiated contact fiber laser.
Does that make any sense?
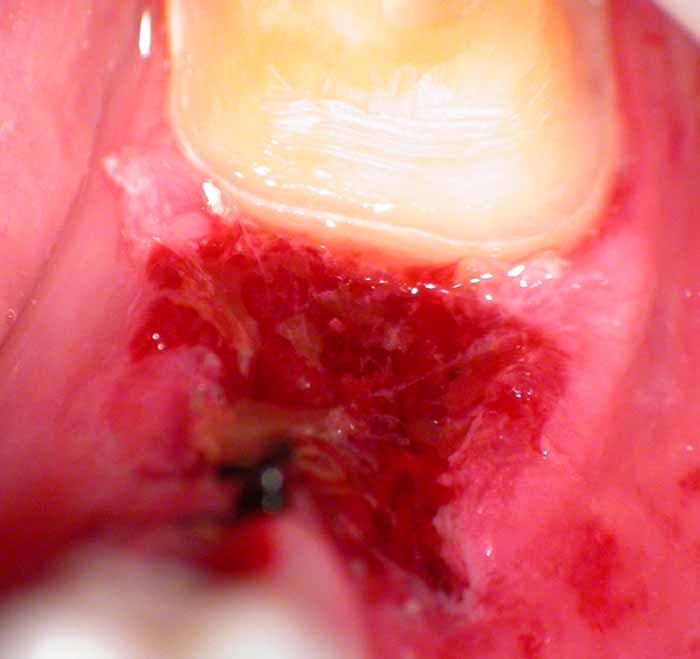
Here’s a photo I took today of a stable fibrin clot in an extraction site after I removed the tooth and lased the site at 4.0 watts, 20 Hz, 150 usec for 200 Joules with a 360 micron fiber. The patient is taking 100mg of aspirin a day and says he tends to bleed easily. Ha! Not around me he won’t. This distal tooth was prepped after getting the clot so I could watch the clot stabilize. It stabilized in about 3 minutes and only got more stable as I prepped the tooth. This is the photo after I prepped the tooth – 10 minutes later. Ready to make a temporary. That black thing there is a suture. Contrary to my periodontist friends, I do use a blade and sutures once in a while (root decayed below the gums)
Here’s a general description of laser wounds from the surface down:
Histology of the Laser Wound
1. zone of ablation – the zone of vaporized tissue (or not)
2. zone of coagulation (necrosis) – the surface of the wound.
3. zone of stasis (injury) – deeper and peripheral effected zone
4. zone of hyperemia (edema) – deepest tissue zoneFurther defined:
ZONE OF COAGULATION (NECROSIS)
This zone is comprised of the surface tissue necrosis of the initial burn eschar. Irreversible injury.ZONE OF INJURY (STASIS)
Deeper and peripheral to the zone of coagulation, there is an area of tissue injury where cells are viable but can easily be further damaged. Fibrin deposition, vasoconstriction, and thrombosis occur. Early epithelial cell death in this area, unrelated to blood flow, can be quite high, leading to slowing of healing.ZONE OF HYPEREMIA (EDEMA)
Peripheral to and below the zone of stasis is the zone of hyperemia. The area is characterized by minimal cell injury but with vasodilatation (edema) due to neighboring inflammation-induced mediators. Completed recovery of this tissue is expected unless there is an additional severe insult such as an invasive infection or profound tissue inflammation.QUOTEIf I could vary and thus increase the pulse duration on my Erbium from say 150 to 550 microseconds would I see an improvement in hemostasis in soft tissue?Unfortunately, no. It’s due to the fact that erbium being highly absorbed in any tissues in the mouth, you would not get a deeper effect on the zone of stasis, but a deeper effect in your zone of ablation and the amount of tissue vaporized.
QUOTEHow come today’s Erbiums don’t come with user adjustable pulse durations? I guess the Cavilase that Jack Miller showed me one time did have a variable PD – anyone know if the PD is “user-selectable” on the Opus Er:YAG?Erbiums are still evolving. The devices on the market today are 2nd and 3rd generation. Cavilase was going to be about 4th generation erbium with its 3 different pulse durations (100, 250, 350 or something like that). The PerioLase 5th generation. But the erbiums are ALL still analog versus digital for the PerioLase, which makes selectable pulse durations so much easier and efficient. The technology for the erbium is still developing compared to the technology for the pulsed Nd:YAG to some extent.
Also, the manufacturers will need to understand that there is a clinical need for different PDs. For that to occur, the clinicians need to be able to determine (as Del and I did) how different pulse duration effect, in the case of erbiums now, hard tissue differently. In some respects, we have a means to compare two different erbium pulse durations – Waterlase at 90 to 140 microseconds (depending on who’s numbers you accept) and DELight at 240. That’s a significant spread. I think that while very similar, there are advantages at times to using the 140 usec say over the 240, and vice-versa. Now combine that difference in pulse duration and add the effects of different rep rates and higher millijoules per pulse, and now even I am getting interested in the erbium. (Oh, that’s right, I’ve ALREADY been interested since 1990……..).
So quite literally, the advances in erbium devices will be the direct results of clinicians like Glenn, Bryan Pope, Mark Colona, and others who pay careful attention to the effects of different parameters, and engineers listening to what the clinicians are saying (a very hard thing to occur), and THEN do something about it. But the clinicians are KEY to the next big advance in erbiums. Like we talked about at CDA Anaheim.;)
Great questions!! Thanks for asking. I love it when I have to stretch my mind to make sure it makes sense on paper.
Bob
Glenn van AsSpectatorHi Andrew: I will say this that when I started using the scope 5+ years ago I was astonished at what I could see and I started trying to take photos (35mm). Man was it hard. I was so thrilled when some of the digital cameras could be mounted to the scope…..it was revolutionary for me.
To be able to photograph what I saw through the scope was unbelievable. Over the years I have read quite a bit on digital photography and learned some more from masters like Gary Carr, Eric Herbranson and some who dont use a scope. The amazing thing about the scope is how easy it is to take the photos and to document procedures……
ACDSee 5.0 is a pretty good archiving program and the ability to make collages from the photos is pretty easy in there so thats how it all came about.
Who knows……maybe one day I will make a book out of them all but that remains to be seen.
I gotta get a DVD burner soon and back up all the images I have on a hard drive or a DVD or two.
Take care and thanks for making my day……
Glenn
Glenn van AsSpectatorHEy before I read the rest of the post……….COOL photo.
Nice picture, now you are getting the hang of it. It took me forever to take the pictures and get them that good…..I hate to see where you will be in another 3 months with the scope , digital camera etc…….
GRIN
Nice stuff.
Glenn
whitertthSpectatornice job!!
Robert Gregg DDSSpectatorThanks Glenn,
I AM getting the hang of it! And I owe it ALL to you!!
My first pics (as you saw) were for s _ _ t.
I’m really only as good as you have helped me to be!
I LOVE being coached by a skilled Master and excellent teacher, as you are. The student is the reflection of the teacher, don’t you think?
You are my photo Yoda!:biggrin:
This is just an incredible way to communicate clinical dentistry and the effects of technology. Unfortunately, it is such a powerful medium it can cause some negative reactions, as well as positive impressons.
Can I borrow your flame retardant suit next time I post on Dental Town? Ha!
Bob
2thlaserSpectatorHey guys, I’ve been here! Glenn, you’ve been MIA!! with all your meetings lately!
I have taken off polycarbs as well as luxatemp temps. It is so easy, and the patients don’t feel a thing. Like butter!
Also, you guys are too nice, you teach ME quite a bit as well. That is what is so cool about this forum. Glenn, I am presuming I won’t see you this weekend. I am in Vancouver for the day 2 lectures, then off to Seattle to be with my wife on her birthday that night. Oh well, I will be back up there soon I am sure. We will have to get together.
See you all soon.
Mark
Robert GreggParticipantCLAP CLAP CLAP
Here Here!!
I concur.
Woo Whoo!
I EXPECT a book one day from you Glenn. Heck, It oughta be on DVD.
Andrew, I forgot how handsome and distinguished you are!! Dang that’s a great picture of you and your next-door neighbors!
Bob
Robert GreggParticipantJeff,
Is that DT mean Dental Town or Dentistry Today??? I’ll check it out. Did you get some ink or face-time??
Ron,
Sorry to take so long to respond. Gettin busy around here!
“If there were no pigment present (stain) would you still get etch effect?”
No. There has to be something organic on or in the enamel for the Nd:YAG to absorb into. Unless it is dentin. Then it looks like this:
[img]https://www.laserdentistryforum.com/attachments/upload/NdYAGetcheddentin.JPG[/img]
A recent article in ESOLA journal mentions melting of enamel and dentin surfaces by nd:YAG, is this what would happen w/o the presence of the stain?”
Which article was that? Fried’s?
I don’t think so, is the answer to the question I think you are asking. Organic material must be present at or pretty darn close to the surface for the Nd:YAG to have an effect. Due to the focal length (spot size) the energy density drops down too much for any absorbtion to occur at the CEJ below that enamel (unless air or a passage way exists).
Did that answer your question?
“If there is some melting and recrystallization, is the tissue more resistant to acid?”
Oh, Yes. How much and how long, etc., I don’t know (or I forgot).
Bob
Robert GreggParticipantHey Al,
Sorry It took me a while to see your post and Del’s–and he’s across the hall fom me, not the country like you are!
How does the 1064nm FR Nd:YAG affect the pulp on vital teeth?
No detrimental effect at all. It will have a pulpal sedation effect like what is talked about with erbiums.
Doesn’t the energy penetrate much deeper than my 2780 Er,Cr:YSGG?
The energy of the Nd:YAG will indeed penetrate much deeper than the Er, Cr:YSGG, but will be transmitted since there is little tissue that will absorb Nd:YAG in a healthy pulp.
Did you select a short Pulse Duration in this case to prevent pulpal damage?
Yes, I chose the shortest I have available to me–100 microseconds.
Is the fiber in contact with the dentin/caries?
Oh yes.
Is it possible or would there be any advantages to using a water spray with the FR Nd:YAG?
Some, but only for removing carbon deposits and keeping the plasma plume down–which causes gray plasma deposition on tooth and soft tissues nearby.
But remember that this wavelength is completely transparent to this 1.064 light and the interaction at the surface would be hindered with water or mist covering the dentin/decay.
Good questions. Thanks for asking.
Bob
BenchwmerSpectatorBob,
Picture and info on May issue of Dental Town, page 38.
Today, The Severna Park Voice (5/15/03 issue), local weekly newspaper, had an original article I wrote Advances in Laser Dentistry/Technology w/ photo.
Mentions LPT and Erbium uses.
Jeff -
AuthorPosts
