Forum Replies Created
-
AuthorPosts
-
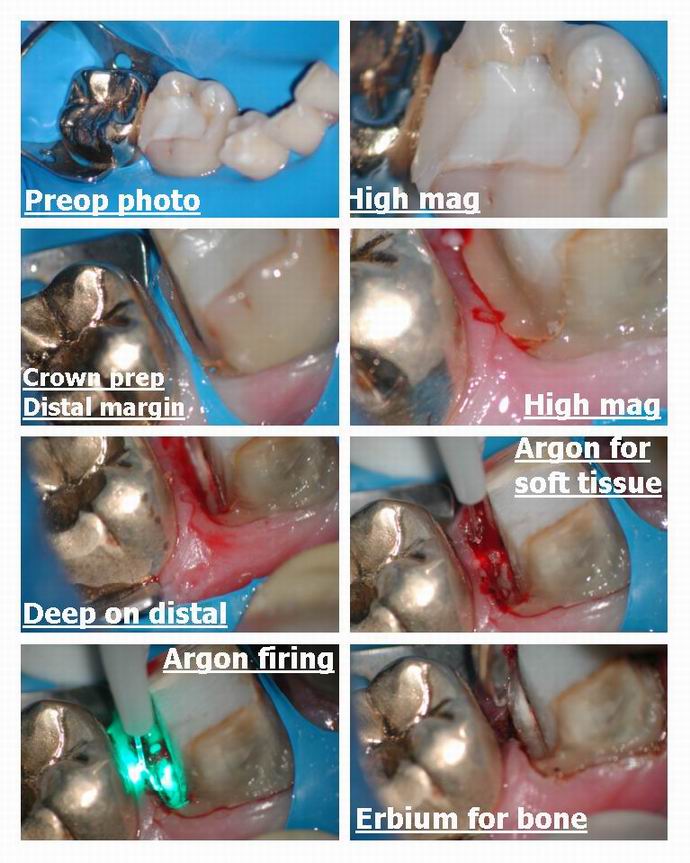
Glenn van AsSpectatorHi Folks……..I dont think I ever posted this case and if I did I apologize but here is a single appointment prep, osseous recontouring with the erbium and impression case.
The molars in the posterior had bad decay, they were endo treated and core composite buildups. Slowly with time we have been doing crowns (for financial reasons) and eventually got to the lower molar for a procera crown.
The prep was very deep on the distal and due to an open contact interproximally and food entrapment the tissue was pretty inflamed so I thought I would remove the tissue with the Argon to minimize bleeding and then use the erbium to remove bone to get a 3 mm biologic width on the distal and then take the impression if I could control bleeding afterwards with the Argon.
The soft tissue doesnt bleed much but when you get into bone with the laser there is a fair amount of bleeding.
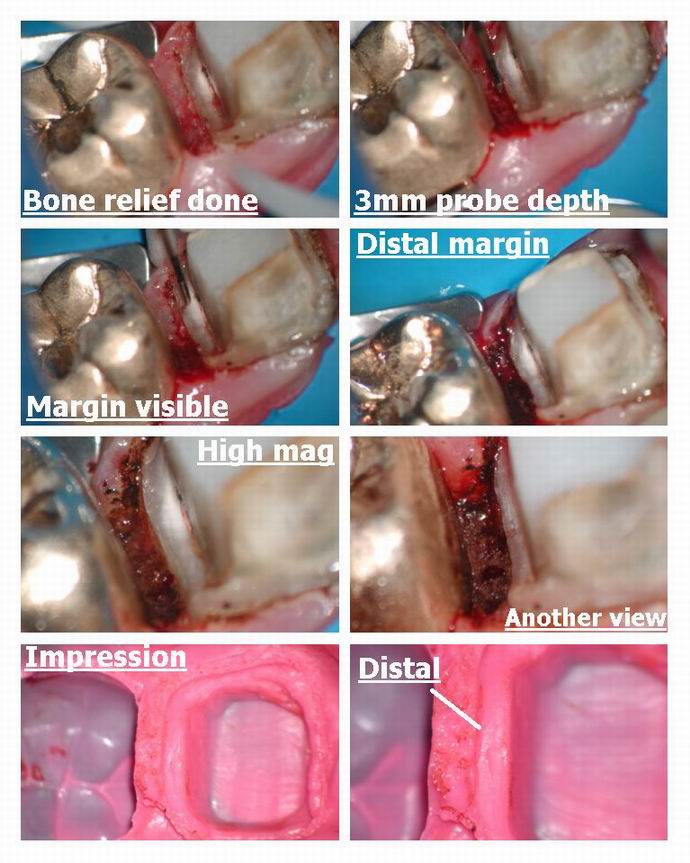
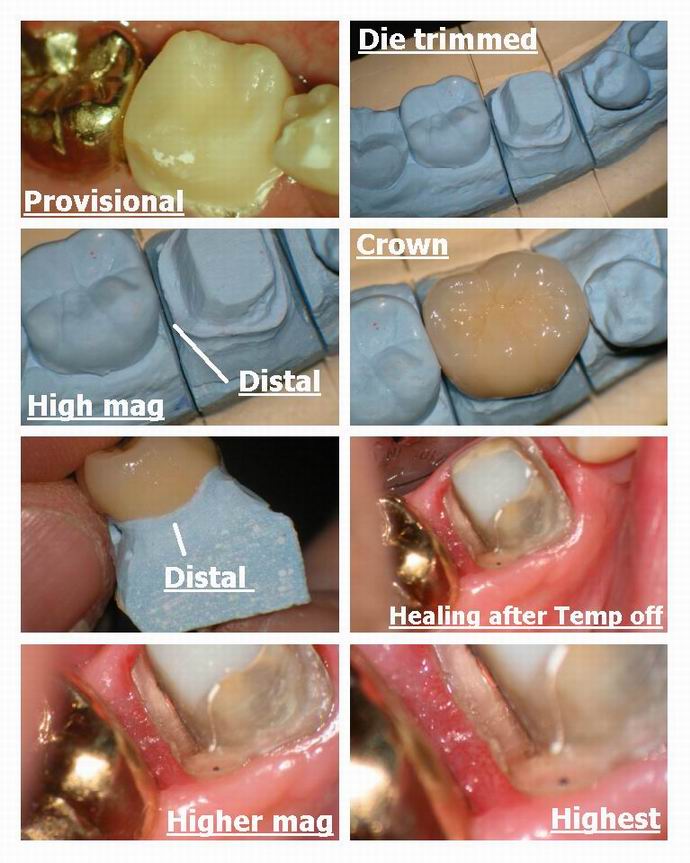
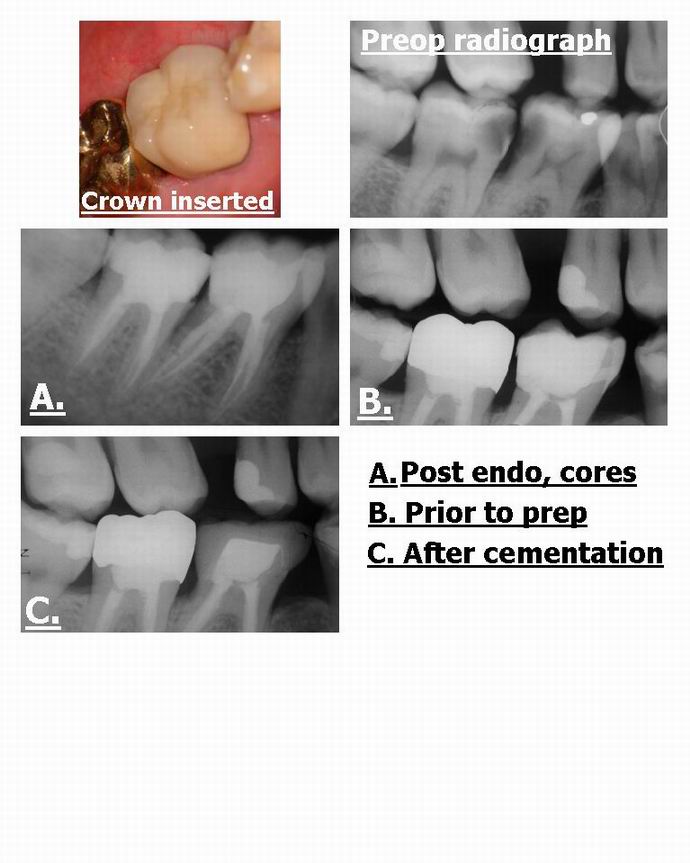
I managed to control it and then took an impression. The insertion of the crown shows the nice healthy tissue ( 2 weeks later) and the crown was placed in .
The final radiograph shows the resulting margin……
Nice easy case with the laser to help me out. This is the kind of perio you can do with the erbium laser Mickey……osseous recontouring bone, but stay away from putting in the laser into the pocket as it wont be selective for soft tissue and there are better lasers for Laser Perdiodontal Therapy
Hope you like it………
glenn
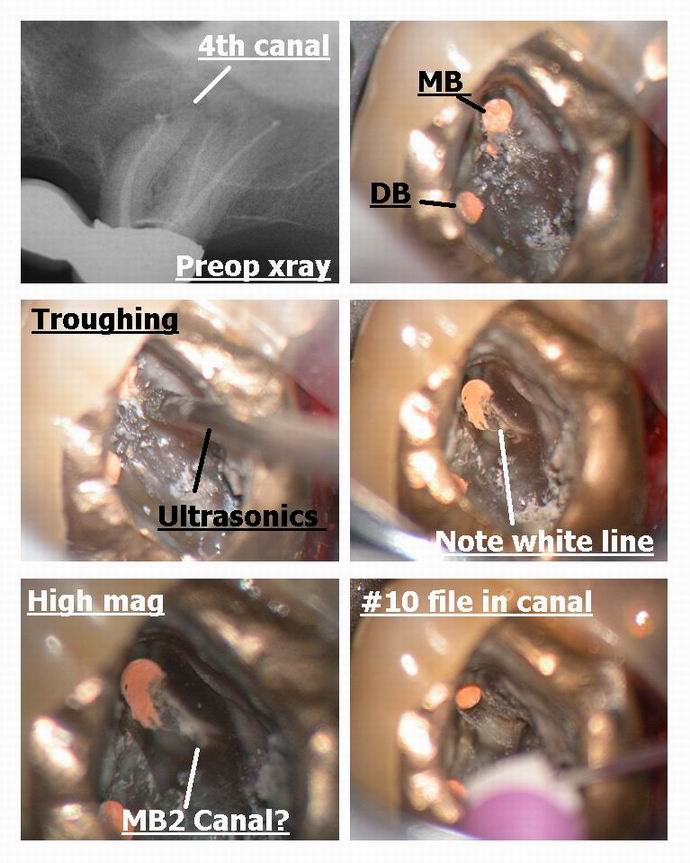
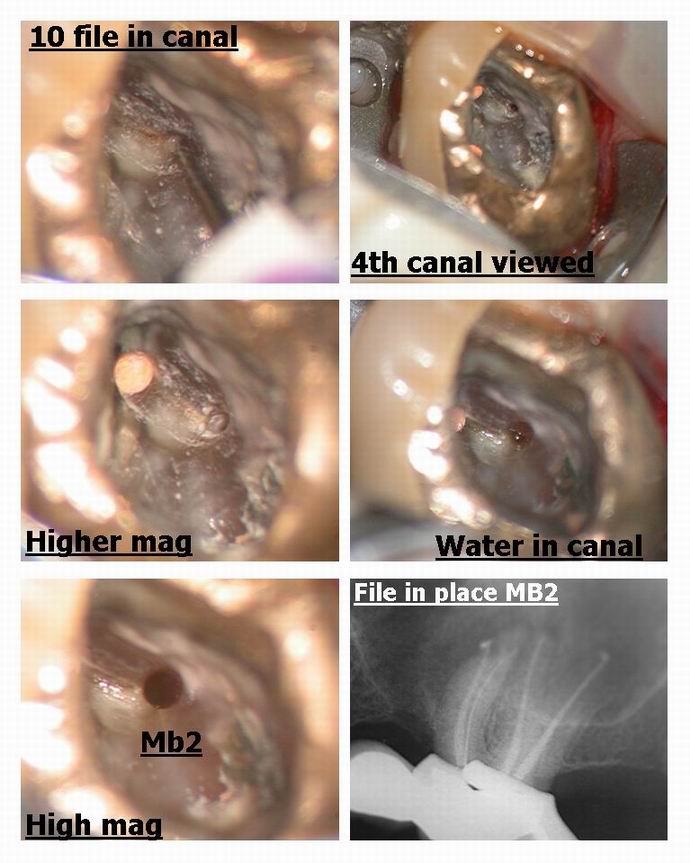
Glenn van AsSpectatorHi Bob: I just wanted to point out that uncovering 4th canals is easy with the scope ( bob used it too) and here is a case not using the laser which shows this principle.
My associate did a nice endo on this tooth but I noticed a root unfilled ( the MB gutta percha isnt centered in the root meaning another canal exists) so asked him if I could look for it (hes putting a new bridge up there).
On opening it up …….I troughed with an ultrasonic tip from the MB down to the palatal and a little mesial from a line connecting the two canals.
What is interesting is that the MB2 is often located mesial to the line drawn from MB to P canals and when you uncover it, it goes first lingual and then mesial before curving back towards the MB canal……you can see this clearly on the photos.
There is ALWAYS a white line connecting the two canals as can be seen in Bobs photos and in these photos.
The SCOPE is ESSENTIAL for finding these. I found another 4th canal on a maxillary 2nd molar on thursday on a failing case and have 2-3 times found 5 canals on cases in lower molars.
THe white line is made clearer by the Nd Yag or ultrasonics so you can locate the missing canal……MAGNIFICATION IS ESSENTIAL.
Hope this non laser post helps……
Glenn
Glenn van AsSpectatorHi there……….Bob its the 980 nm wavelength not the 908nm……..its the diode by Biolitec that is 980nm.
Just wanted to clarify because otherwise newbies might get confused.
810 nm diodes (many available in this range )
980 nm diode (Biolitec, also soon Deka)
1064 Nm NdYagAll are soft tissue lasers.
Glenn
PS great stuff Ron , great to have your knowledge for literature on lasers out there.
ASISpectatorHey Glenn,
Very nicely done. Once the 4th canal is located, was it patent in terms of ease in sliding the #10 file down?
I often find that a path finder or #8 file is needed in addition to piezoelectric(I use a Booster P5) crowning down. The scope is a real illuminator though. What a great tool!
Andrew
Glenn van AsSpectatorHi Andrew…….this wasnt the first file in but the third.
I used a #6 first til it could get as far as I could get it, Then #8 and # 10 just to get a little hole opened up.
THere is a reciprocating handpiece attachment called the M4 made by Kerr that can attach to my Technika ATR and I use that to open up the coronal half it takes regular K files in the M4 and opens it up reciprocating 30 degrees either way in a watch winding motion. I dont go to the apex because it can elipticize the apex but it helps open up the canal without risk of seperation and in addition once I open up the coronal then I can often get a small file to the apex …….
Use Glide or EDTA to help lubricate as well.
Vision is the key though.
Glenn
AnonymousSpectatorHi all,
I was reading an old Landeburg Thalman (Feb 02) Equity research report on Biolase, that was sent to me, and found an interesting statement.The paper states;
“Disposable tip sets must be purchased from Biolase at 趚 per ten tip set, with each tip intended to last for three patient procedures.” It continues to talk about how dentists use the tips longer and that the analysts “predict that the average Waterlase dentist will use each tip 25-30 patients before replacing it.”
This brings me to my questions –
How often were you told to replace tips?
How often do you replace tips?
Could less frequent replacement cause fiber failure due to the tips becoming inefficient, causing heat build up?Just wondering,
Robert Gregg DDSSpectatorGlenn,
Just pure POETRY in pictures. Beautious to the MAXIMUS! What a gorgeous case and awesome documentation!!!
That tissue response is just incredible. What a terrific service for the patient (that they will never fully appreciate).
And to think some on other forums want to insist you and the rest of have our lasers JUST for marketing–or that a blade is equal in EVERY situation (no offense Andy;)
CLAP CLAP CLAP
Bob
Robert Gregg DDSSpectatorHi Kelly,
The 320 would be easier to use in the beginning, but the 220 (200?) would definitely have greater energy density and allow you greater access deeper into the canal. But you really need to be careful and lower your energy because that is really intense.
I used a Global Surgical operating microscope, fitted with an X-mount from Global, with a Nikon CoolPix 4500 attached to that.
It has the magnification AND the coaxial illumination that allows for awesome visibility that indirect illumination alone just can’t give.
Glenn van As here is the expert on magnification & photography and can tell you lots more….
Ron,
I know what you mean. It can get VERY confusing when calculating energy density with quartz clad fiber optics.
The simple answer is I got these numbers off the ADT Pulsemaster 600 IQ energy density chart. But calculating them can be problematic.
The formula is ED = Joules divided by surface area. Surface area is Pi (3.14) times the radius squared.
So if you have a 320u fiber the surface area calculaton that was apparently used by ADT is apparently .8123. Divide 200 millijoules by .8123 = 246.21445.
Now the problem comes in when you are trying to extrapolate this to other fiber diameters, and then you find out that is does NOT correlate. The reason for this is that…..get ready…..a 320 micron fiber may not really be 320 microns in diameter. Huh?:confused:
Ok. Depending on the manufacturer specifications, there will be the quartz core diameter of say 300 microns, then a quartz coating of say 10 microns, followed with a polyimide (correct spelling) coating to protect the quartz cladding of another 10 microns. So the accurate way to calculate is using the actual CORE diameter–NOT the core diameter PLUS the resin and quartz outer layers. But is this what ADT did? I don’t know, and I need to check their numbers. Which is why I said I needed to check their numbers!?:confused:
Does that make any sense?
Thanks Glenn.
Good point. Great photos as usual!
I also use ultrasonics with various endo tips. In fact, I used the ultrasonics right after I got blocked in the last photo to trough the canal open wider. Then I went back with the Fr Nd:YAG to clean out the dentinal debris and get a clear view.
But that assumes we always know WHERE to trough. Sometimes the canal can “hide” in places unexpected, and the coloration and even the normal anatomical landmarks are missing.
The pulsed Nd:YAG has the optical capability to differentiate between different densities and chemical components of intra-pulpal materials.
So using the Fr Nd:YAG to identify, then open up the canal using instrumentation of choice (ultrasonics), then going back with the Fr Nd:YAG to clean out the dentin debris is a nice combination. That and how magnification makes it easy to view can really be an awesome enhancement.
You are very correct about the way these MB2 canals go one way, then track back another, too.
Also, ultrasonics–like rotary instruments–are “indiscriminate” hard tissue cutters. They also create a lot of debris that covers the area I am trying to view. With a pulsed Nd:YAG laser, I can remove tissue one to three pulses at a time, keep the viewing field completely free of debris, and watch the progress as it is taking place, giving me much more control, access, and visibility than even when I use ProUltra ENDO ultrasonic tips (from Tulsa Dental).

So, I love using the laser to locate, the ultrasonics tips to cut quicker, and the laser to clean out the debris from ultrasonics in an alternating fashion. Combining the two technologies together with the microscope makes for an awesome combination–and lots of fun too.
Thanks everyone for a great discussion!
Bob
Robert Gregg DDSSpectatorGlenn,
I guess we both not reading very well. 😉
Ron’s post was about a 10 milliwatt LLLT laser of the 809nm wavelength. (an 809-nm diode laser operated at a power output of 10 mW in the continuous wave (cw) mode at energy fluences of 1.96-7.84 Jcm-2).
I transposed the numbers from 809 to 908 confusing you and others….oops. Sorry.
The point for newbies is that all lasers in the near-infrared 800 to 1500 will have a similar effect, whether used in Low Level Laser Therapy (LLLT) with a 10 to 250mw biostimulation laser (with no surgical capability), or High Level Laser Therapy (HLLT) using the lasers you mentioned that are primarily surgical lasers with many Watts of output power (not milliwatts), but defocused have biostimulatory effects.
Thanks,
Bob
(Edited by Robert Gregg DDS at 3:19 pm on May 31, 2003)
Andrew SatlinSpectatorI don’t think a blade is equal in every situation, I think it’s Better!! (lol). Honestly though, from what I have seen on this site, Glenn could do beautiful dentistry with any instrument. If I needed this work done in my mouth I would choose what was just shown. Except for the flying up to Canada part. Too cold–and our hockey teams are doing better anyway. Go Ducks!!!
Have a good weekend all.
Andy
Andrew SatlinSpectatorHi Glenn,
Very nice case. Great tissue healing at two weeks!
Forgive me but I am still a rookie. Erbium recontouring– is that a gingivectomy for esthetics? Then why the troughing? Is that also done with the erbium?
Andy
Glenn van AsSpectatorHi Andy: I used the erbium to recontour the tissue so the heights of contour (the gingival heights) would be similar.
The troughing is done to back the tissue from the margins for impressions to get a sharp margin.
All the best…..
Glenn
AnonymousSpectatorQUOTEQuote: from Robert Gregg DDS oThe formula is ED = Joules divided by surface area. Surface area is Pi (3.14) times the radius squared.
So if you have a 320u fiber the surface area calculaton that was apparently used by ADT is apparently .8123. Divide 200 millijoulesby .8123 = 246.21445.
Bob
The 200 millijoules is the assumption that I missed.
Thanks for the explanation.
whitertthSpectatorGlenn, that case is purely awesome….. Great surgery and an unbeleivable final result……u should be proud…
all the best!
whitertthSpectatorI’m not sure about Hoya, but Biolase doesnt yet make a tip that has a wider diameterwhich would allow u to recontour bone a bit faster…. Luxar once made a wider ceramic tip for soft tissue that might be nice for more rapid bone removal…Glenn what r your thoughts about tip diameter…BTW Did u anaesthetize in this case…. also how long did it take? once again… warmest regards
-
AuthorPosts
