Forum Replies Created
-
AuthorPosts
-
Glenn van AsSpectatorRon : one thing I am almost embarrassed by is that I have forgotten now what it is like to do dentistry without the scope. I hear now so many dentists who are concerned about doing quality work without jeopardizing their backs and necks to lean forward going to higher and higher mags.
THe magnification continuum ( magnification junkie is another word I hear) is something that leads to more and more magnification as we learn the value in seeing better.
I am a big proponent in scopes obviously but using a minimum of 2.5X power for lasers is a must in my opinion as the tips are so small its tough to see without the loupes.
I think that as you move up in magnification the light becomes increasingly crucial and one thing with the scope is the lighting is co-axial and that allows for no shadows.
I dont really use smooth diamonds very often (sometimes) but working at 10-16X power allows you to focus on the margins and get it where you JUST want it.
I often believe that we try our best to do good work but sometimes our eyes (not our hands) let us down. When we send better impressions to the lab which are prepared with magnification we get better results and I think the lab has to do less “fudging” of the margins.
I laughed yesterday because I have one awesome dental assistant who is very keen and knowledgeable now. We have the scopes in the operatories and there is a video going to a monitor for them to see what I am doing and this allows them to keep the suction out of the way for instance.
My assistant is looking at the monitor smiling as I am trying to get a canine crown to seat and I ask he what is so funny. She mentions that she knew the crown will seat as soon as I get the interproximal contact trimmed down because the gap at the margin is not smooth and the little individual indentations are about 2-3 degrees off on the crown compared to where the indentations should fit on the tooth. She could see the discrepancy visually and knew exactly why the crown wouldnt seat the whole way. I adjust a little more and bang…….down it went.
These crowns were the ones I did for that osseous recontouring case and I am going to summarize the case for everyone and post it in a minute…………..sooo to make a long story longer…………yes magnification and illumination (Xenon light on the scope is unreal) make it easier to do margins which are smooth to your eye but clinically there still are alot of little indentations and bumps so I have a LONG way to go before I get to perfection.
Thanks as usual and congrats on the 4.5X loupes, your laser dentistry patients are the winners in this whole equation!!
Glenn
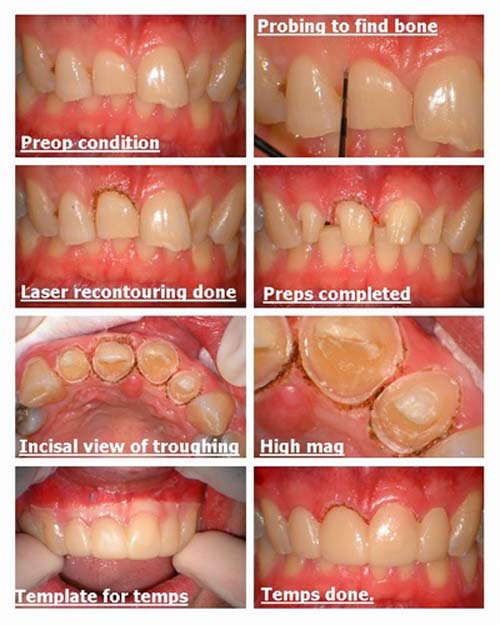
Glenn van AsSpectatorHi folks: Here is a case we did yesterday in the office. 4 anterior crowns which we prepared.
I noted that the gingival architecture on the crowns was not even on the centrals so I used the Argon at 0.9watts continuous to adjust the lengths at the gingiva and make them more even.
THen prepped the teeth and used the laser at 0.9 watts with water and air to trough for an impression.
Temps were then placed.
Just something to look at for a Friday morning.
Glenn
PatricioSpectatorGlenn,
What are the do’s and don’t for troughing on the facial? I have been a little reluctent to trough this area and risk recession and possible margin exposure where I did not want it.
Pat
Glenn van AsSpectatorHi Pat………couple of points
1. Use minimal energy possible- I use under 1 w where possible
2. Blow air or water on the site to cool it.
3. Avoid going over the same area to many times and magnifcation helps here.
4. Keep your temps slightly short to prevent pushing the tissue back
5. DOnt do on patients who are extremely picky and who have fragile , friable tissue with multiple areas of recession.Hope that helps some………I dont have all the answers but will say that a diode is better than my argon and I guess the Nd Yag will be better than both due to its fast pulse rate and allowing the tissue to relax.
Glenn
RodSpectatorAny chance we could see a VERTICAL BWX?
Here’s what I’d try:
First of all, I’d do NO pre-surgical root planing, etc. Pre-surgical (phase 1) root planing could cause the tissue to firm up and shrink. It would also cause the immunilogical factors that are present in high amounts to diminish (by becoming temporarily more healthy). This means that the tissue would be more difficult to manage if it had shrunk and become more fibrous. And you WANT all those immunilocial factors present in mega amounts when you do regeneration. (learned this from Bill Becker himself)
Some sort of temporary splint — even if you had to put a glass fiber ribbon splint on both the buccal and lingual, with the idea that with success, you can remove. Keep it away from the gingival area.
I currently don’t use the laser when I do these. But it certainly couldn’t hurt (possible biostimulation?).
I’d do a great endo. I personally think this is a must. With this much bone loss, there has got to be some endo problem via lateral canals — lotsa literature to back this us — esp. by Selzer (sp?). They’ve shown that even when you get a normal pulp response to EPT and thermal tests, when there is this much bone loss, there are virtually ALWAYS areas of ischemia in the areas of the lateral canals.
I’d flap the area, root plane WITH ZEZA ULTRASONIC CURETTES (this is important in my opinion), absolutely impeccable debridement of the boney defect with the same ultrasonic curettes, taking away a little layer of bone. Just be sure to ONLY use the ‘root planing’ inserts, and NOT the surgical inserts. The ‘surgical’ ultrasonic curette inserts are WAY too aggressive, even for the debridement of the osseous defect (which is what they’re meant for). Just use the ‘root planing’ ultrasonic curette inserts for both root planing and osseous defect debridement.
And yes, do de-epithelialize the internal of the flap, but don’t get all that aggressive — you don’t wanna impair circulation in the flap.
OH, by the way, very important — when you give anesthetic, be sure you use 1:50,000 epi at least 25 minutes prior to your incision. And be sure you give it both buccally and palatally adjacent to the root. This will give you good hemostasis, and that is important in this procedure.
So after your GREAT root planing, GREAT debridement of the defect, and de-epithelialization of the internal of the flap, treat the roots with PrefGel (by Biora — the Emdogain people) for 2 minutes. Literature says you could use citric or even phosphoric acid, but in much shorter times. I disagree. Citric acid will denature proteins, and I don’t like that idea. And phosphoric stimulates bleeding — not good with this technique.
Rinse well. At this time you should have virtually no bleeding.
Inject the Emdogain gel into the defect, onto the prepared root surfaces and to the internal of the flap. Then place your graft material (I’ll discuss below)to fill the defect and close with matress sutures (you don’t want the suture material going through the graft material. I suture with GoreTex sutures. You need to get primary closure.
If I get EXCELLENT primary closure, I usually don’t put on packing. But if the closure is not as ‘sealed’ as I’d really like, then I place packing.
The graft material. I specifically like the Pepgen P-15. Consider this — we know that DFDBA (Demineralized Freeze-dried Bone Allograft) will hasten bone regeneration to a degree. It’s been found that only one out of 3,000 proteins in DFDBA is responsible for this enhancement of bone regeneration. And that protein? Yep, it’s ‘P-15’. Obviously a product that is saturated with pure P-15 is a big plus — studies of this are totally awesome.
But P-15 is dense as all get-out — and this would prevent in-growth of blood vessels and bone percurser cells. So I mix DFDBA and Pepgen P-15 in about a 50-50 mix. The DFDBA will resorb very quickly and is very spongey — thus allowing rapid ingrowth. And the Pepgen P-15 will accelerate attraction of these cells.
I first mix them together when dry (much easier to get a homogenious mix when dry). Then I hydrate with sterile water — I personally mix just a ‘pinch’ of tetracycline in with the water first.
Place the tetracycline in some sterile water (or saline) — just a VERY LITTLE (we don’t want the HCl in the tetracycline to give us much acidity). It should give the water only a very slight hint of ‘yellow’ if you only put the slightest bit in. Let the solids settle to the bottom and suck up the top of the water in a syringe and squirt that into the graft mixture to start the hydration. I do this right before I make my flap. The material should hydrate for a minimum of 15 minutes.
And don’t ‘float’ the graft mix with this water. Once the DFDBA absorbs the water, you want it rather dry (barely moist).
I don’t use a membrane. The Emdogain enhances acellular cementum formation, which in turn forces fiber generation, and that in turn forces bone generation. And the graft material then enhances the ‘fill in’ of the bone between the teeth. If you use ONLY Emdogain, you sometimes get only a thin coating of bone forming on the root surface, with no bone inbetween — this is still good, but I’d prefer bone right straight across.
Emdogain has been found to prevent epithelial down-growth, so I don’t use a membrane. Pepgen P-15 has also been shown to prevent epithelial downgrowth, but this may not apply when mixed with DFDBA (don’t really know)
I then place the patient on Peridex rinse as well as Doxycycline 100mg bid for 2 weeks.
When I say that these patients have no post-op pain, I mean they have NO post-op pain. It’s weird!! You haven’t ‘recontoured’ bone. You haven’t place irritating membranes. And I truly think there’s something about the Emdogain that virtually tells the tissues that nothing has been done.
So far, every single patient, without exception, has said they didn’t even need to take Advil or Tylenol! I kid you not!
GTR membranes always seemed to work very well in my hands, yet this technique has results that are even better.
So yes, if the patient wants to ‘try’ to save the tooth, I’d say OK, and THIS is the technique and approach I’d use.
How ’bout that vertical BWX?
Rod
(Edited by Rod at 12:39 am on Jan. 25, 2003)
2thlaserSpectatorNow, Rod has GREAT perio background with excellent results, so I would go with his advice here, depending on your skill level Ron. Not all of us, especially myself, has done alot of what Rod has done, but am learning. I would DEFINITELY perform a laser root canal, using the Waterlase, and it’s incredible effect on the tubules in the canal. If you haven’t seen the SEM’s of that, I can send them to you, they are incredible. Since my staff has seen them, I am NOT allowed to perform endo without the use of the Waterlase! We have had GREAT results. I think that you DO have a combined endo/perio/occlusal issue here. I agree with Rod, a vertical BW is very helpful. If you have any questions on the RCT with the Waterlase, just ask. It’s so very easy. Great case, I would DEFINITELY try it. I have had a similar one, and we had excellent success with it so far.
Hope this all helps you decide what to do, from us in the peanut gallery!
Good Luck!
Mark
2thlaserSpectatorPS…if you haven’t done so already, I have replaced using a scalpal for incisions. I use the T-4 tip with about 1W 13%air, 11%water, and have had success with very little bleeding whatsoever, and a great “playing field” in which to work in during flap surgeries. The tissue approximates back excellently, BUT DON’T use too much wattage. Low powers are so effective, especially with the T-4 tip, which seems to exude much more energy per pulse than the G series tips. Just a PS.
Mark
PatricioSpectatorGlenn,
Your comments make good sense. Thanks.
Pat
AnonymousSpectatorWow ! Thanks for the input guys. I have lots to present to my patient.
Rod, I knew you would have a very well thought out approach to this. What’s even better is , once again you’re willing to share it with the rest of us. I checked out the pepgin on line and got an idea of cost but what about the emdogain, as expensive? Got all the literature ordered from Biora.
Mark, I haven’t picked up a scalpel since August. Fortunately on my training day, I did a crown lenghtening where a flap was layed using the laser.Since then I use it for all my surgical extractions or other things I need to flap. I also found the 1.0w was very effective but I think I have the water and air a little lower than you 7/11. How ’bout posting the endo procedure you’re doing? I saw the SEM’s in Ft Lauderdale at the Biolase meeting last spring and they are impressive. I just didn’t get a clear understanding of how, once the laser had cleaned the canal , how the endo was filled. Tapered canal or what do you fill with?Soon as we get the vertical BW I’ll post and let you know if my patient wants to give it a go.
Thanks again,
PatricioSpectatorHi from the frozen north,
I have been successfully numbing anteriors and bicuspids at 1.5w(not 100% Jetsfan). What additional benefits are amassed by using 5.5W as Mark and others do? I am just thinking out loud and wanting your thoughts.
I do know I must enter another watt level to cut so maybe 1.5w is less efficient time management. I also begin without my space helmet and light. When I have fogged the tooth for 30 to forty five seconds, sometimes two or three teeth in the same 30 to 45 seconds. I stop and reset the machine at 3.5 to 5.5w and put my eyes on and away we go. Are there different predictible results for numbing which we can devine at various wattages? How much is enough?
Pat
Robert GreggParticipantNice results Glenn–
Some people are just naturals!
Notice that Glenn left some room for the tissue to receed a little, should it need to do so. If no recession, then he can always touch it up later. That’s a good idea with CW or gated pulsed lasers.
Notice Glenn doesn’t have any epithelial peeling or coagulated tissue beyond his laser margin. That a “cool” wound.
Also, Glenn didn’t burn or char-up the tissue (black), indicating he didn’t overheat the soft tissue thus he’s not likely to get recession.
Some remarks to answer Pat:
1. Direct fiber away from soft tissue you wish to leave behind. Don’t point up into the sulcus.
2. Don’t count on water to cool–it can be deceiving like getting a sunburn on a cloudy day. 810-1064nm wavelength transmits right through water. Use air to cool. Water spray is OK, then air dry.
3. Don’t let water “pool”.
4. Watch for “tan” tissue changes indicating that the tissue is getting HOT.
5. Stop if you are seeing epithelial peeling. The tissue is too hot and will go away.Bob
Glenn van AsSpectatorAwesome points Bob………really good stuff.
I dont have all the answers but will say that for anyone looking at only a soft tissue laser. Consider the Nd Yag and also a diode.
THe Nd Yag is time tested and BObs is obviously the cats meow.
Its great to have such a knowledgeable laser user here on the forum.
Glenn
2thlaserSpectatorPat,
These are valid questions. I usually always use the 5.5-6W defocused (at 10mm away), 90%air, 73%water. I know that this weekend in Dana Point, Stu Rosenberg will be discussing 2 other methods he uses with the Waterlase in our afternoon hands on seminar. I think he will discuss the way you do it, a la Dr. Chen, and then I know Bill Grieder has another way he will discuss. I, like you, am interested in learning other methods. I DO have GREAT success so far the way I am doing this, so who knows. Glenn, what do you do with your Er?
Mark
AnonymousSpectatorHi all,
After a morning of discouragement with the Er,Cr:YSGG (2nd molars on females 14-25 are something else aren’t they?), I decided to get a little laser assistance with a surgical extraction of a fractured endo tooth (Pt didn’t have $ for crown lengthening)
Preop images


.
Used Er,Cr:YSGG 4.0 W 50 h20/40 air with 6mm tip. Place tip interproximally to remove bone mesial and distal.
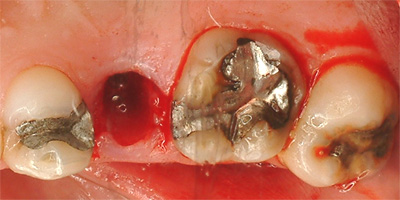
Post ‘troughing’ image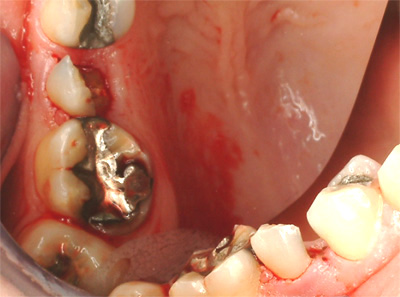
Elevated 2 pushes on distal and 1 push on mesial and out it popped.
Extraction site Image
Extracted Tooth Image

Patient was thrilled. I had told her ahead of time that conventionally we’d flap, remove bone with burr, suture, and that the tooth would break up and she’d be very sore afterward.
I think she’ll do a little better than that
AnonymousSpectatorDiode Trough 1.0W CW Used the air to cool -thanks for the tip ,Bob!
My real question has to do with the fracture on the distal (that is a base on the occlusal , not amalgam -still learning to control the flash on the camera). I was able to put the finish line for the FGC cervical to where I could see the fracture end. What is the consensus for the crack- leave alone , laser etch & seal , or chase the crack?
-
AuthorPosts
