Forum Replies Created
-
AuthorPosts
-
Robert Gregg DDSSpectatorRon (K),
Nothing for me to disagree with what you wrote–or even offer an “old salt’s” alternate perspective……
Bob
SwpmnSpectatorQUOTEI need some assurance that the laser is being used to achieve the effect and its not just placebo effect.Above selected quote from Schalter is my motto.
Some people think anyone using a laser in dentistry is a quack. For this reason we need to be very careful in what we report. I once had a dentist literally get in my face and challenge me with questions even though my use of dental lasers is very conservative. In my opinion this is a scientifically-based forum and should remain that way.
How about creating a category on the forum for “LLLT/HLLT” or “Alternative” or “Investigational” or “Biostimulation” uses of lasers in dentistry?
ASISpectatorKelly,
That is amazing healing in less than 2 days. What was the diagnosis of the lesion?
Nice pics.
Thanks for sharing.
Andrew
BNelsonSpectatorRon and Bob,
I am treating a 60+ woman for a very similar dysesthesia. 11yrs duration after a number of implants were placed in mandible. Dr said he damaged the IAN while placing the one in the mand left first molar region. Patient has had no feeling from second bi area to center of chin and gets a severe “electric shock” when touching the gingiva in the bi area. I have treated her 6 times now, 7000-8500j per. The “shocks” stopped after teh first tx and she has an approx 8mm wide area distal to the midline that extends up to the lip and toward the corner of her mouth that still feel numb. She can now put lipstick on and drink normally and is unbelievably happy. I have been treating the entire length of the IAN with additional time on the hot spots near her chin.So all, it does seem to work in some unbelievable situations.
AnonymousSpectatorBruce, that’s awesome!
Are you done treating or will you continue? I stopped when we no longer made any more improvement.
czeqm8SpectatorAre you charging the patient or is it just good will? If you charge, what ins. codes do you use? It is definitely worth a charge. This a tremendous service to a patient that has suffered for a long time. Congratulations on your success!
Matt Brink
KevinMelkerSpectatorFor a guy that is so anti-laser, Bob how many lasers were sold after my anti-laser course?
I read Larry’s comments and I hope when he says standard of care he is relating to proper treatment modalities of perio or perio rest. The Periolase is great but just another instrument in the overall treatment of patients. It is not a cure all but can be extremely beneficial when used properly but not so beneficial when not.
Thanks,
Danny
Robert Gregg DDSSpectatorHi Danny (Kevin?)–
To All: Danny’s is NOT anti-laser. Danny is pro-patient, pro-tooth salvation, pro-bone preservation. I wish every periodontist luminary was as “ant-laser” as Danny is……..;)
It was a good course for us, thank you. We had a dozen attendees contact us in the days after the meeting, and a few of them have signed up since. So thank you for that opportunity.
When I talk about “changing the standard of care”, I am talking about the treatment of infectious/inflammatory periodontal disease by regeneration versus ressection, following sound biologic and physiologic principles.
I was so impressed (as was Ray Yukna) with Danny’s course content and “reverse crown lengthening” (among other key perio concepts) that I included some of Danny’s photos in our Day 4 lecture yesterday.
I agree completely with the statement, “The Periolase is great but just another instrument in the overall treatment of patients. It is not a cure all but can be extremely beneficial when used properly but not so beneficial when not. ”
I would add that it is a remarkable instrument for reasons unique to laser photo-biology and photo-physiology–such as the release of growth factors in tissue following laser irradiation.
That’s why we have 3 days of training before we ship the Periolase, and then have a Day 4 at 6 months and Day 5 at 12 months.
I’d like to hear from some Day 4 graduates to tell their experience and the difference that Day 4 has compared to the first 3 days. Day 4 is a continuation, intensification, sophistication and expansion of laser principles and perio biology/physiology.
Day 5 expands these concepts further. Day 5 attendees can’t believe how much more they learn after 4 intensive days of trainining–so they ask when Day 6 is………..
“You can’t see this stuff enough”
Danny helping tremendously with all his energy and resources (personally and professionally) in the effort to push the current standard of care away from tooth extraction and “Ticture of Titanium” and towards tooth and bone preservation.
“Respect biology and biology will respect you.” — Danny Melker
Thanks again Danny for your “anti-laser” stance!!
Bob
Lee AllenSpectatorGlenn,
Thanks for posting this case. Classy.
I am trying to work out the power densities you used on the bone. What is the area of the chisel tip? I have noticed the groove making with the smaller tips, also. The larger diameter/area tips are the best solution.
Great photos. Makes me feel like I was there.
Glenn van AsSpectatorHi Lee: I am constantly changing my ideas based on what I find closed flap going to open, and open flap plus what Danny and Lookin4t and also Andy advise.
In general for open flap
Chisel tip is first at 40Hz and 110 mj or for higher energy 30Hz and 140mj with lots of water , and little or no air.
Chisel tip is 400 by 1200 microns (I think) or its 400 by 800. I think it is the former not the latter.
For the 600 micron tip 50Hz and 50mj or 40Hz and 60-70mj or 30Hz and 70-90mj
For the 400 micron tip 50Hz and 30 mj, 30Hz and 50 mj.
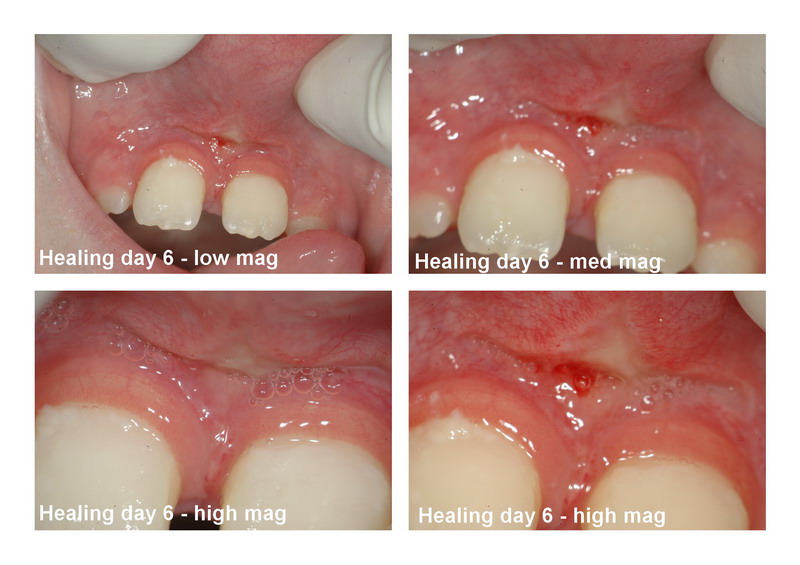
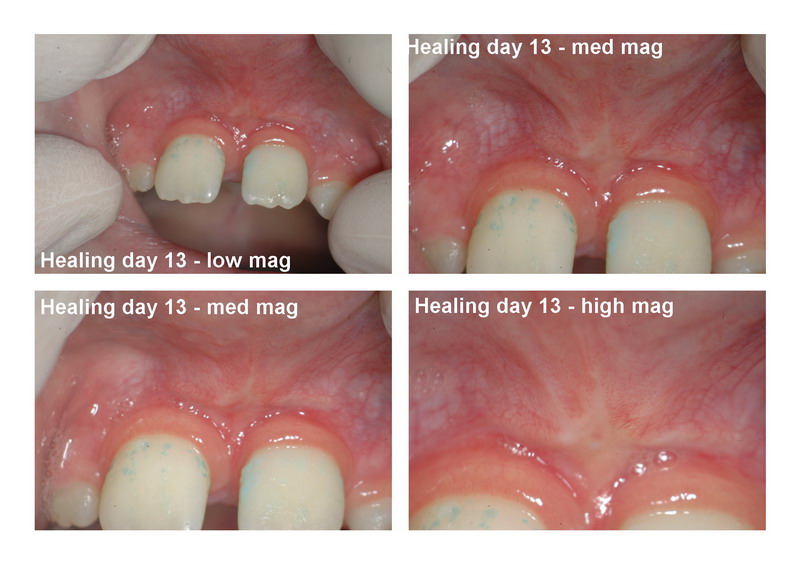
HOpe that helps and check out these 2 week healing photos of the case I did above when I took out the sutures on Monday.
Glenn

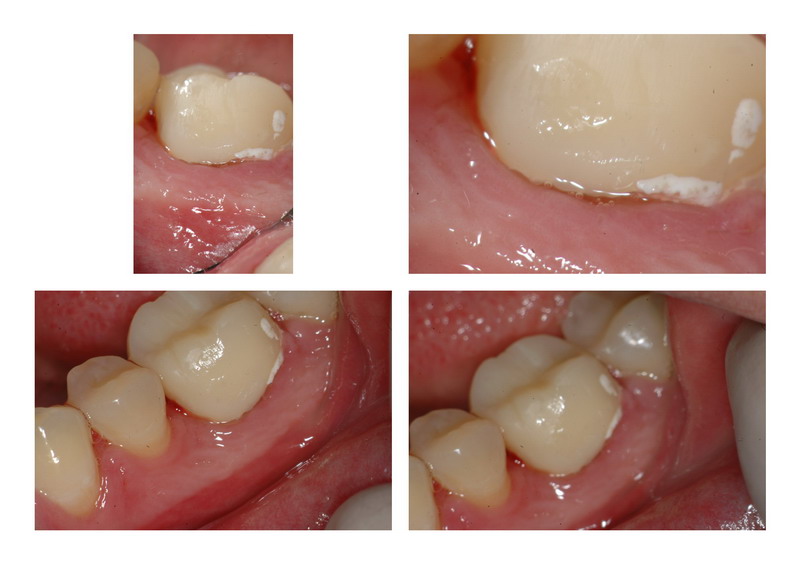
Glenn van AsSpectatorThe Silence is deafening.
Here is a chisel tip erbium yag frenectomy.
Used 40 Hz 100mj with the chisel tip in NON CONTACT.
It is cool to see how this works and I just took the chisel and turned it the opposite way to get the fibers out in between the teeth in non contact.
In my opinion there is less bleeding in NON CONTACT than in contact. Of course anesthetic was used, no water , just air.
I have used the soft tissue tip before but it bleeds more.
This one healed nicely, patient took one advil the first day.
Hope it is interesting.
Glenn


SwpmnSpectatorYeah it is kind of dead in here but here is something that might be worth discussing:
Noticed on Dental Town Dr. van As reported an anectodotal finding that his erbium frenectomies seem to heal faster than diode frenectomies. Not real sure yet due to low numbers but possibly seeing a trend along those lines.
Have a once a week Friday or Saturday stint in a large group practice where have been transporting my 810nm diode for various procedures. Frenectomies with the diode take more time than the erbium particularly when I get down to the attachment fibers. They do seem to heal slower than the erbium frenectomies performed in my office. On the other hand they bleed less. Did one the other day where patient never bled a drop.
We have such outstanding success using the diode laser for crown/bridge retraction that I’m beginning to wonder if the diode laser is better suited for these very fine surgical applications. Since my diode laser is basically always ON, even when “pulsed(gated)”, I’m thinking the longer application time to complete the frenectomy results in a greater overall heat dose to the treatment site. Perhaps this results in more collateral damage and longer healing period. Diode setting has been Continous Wave to 10Hz Gated and 1.5-2.0 Watts with an initiated 400micron fiber.
Maybe the truly pulsed erbium with inherently high peak power and rapid cutting of high water content soft tissue results in lower overall energy dose?
Nd:YAG frenectomists wanna chime in?
BenchwmerSpectatorThis may be East Coast .
A seventy year old woman presents with a longitudinal fracture of #13 (non-restorable), already missing #1,3,14,16. ++ Mobility #2,15.
Treatment plan is for an immediate Virginia Partial denture, with extraction of #13 and Maxillary frenectomy at time of insertion. The partial works as a surgical stint.
Before treatment-

The Virginia Partial is a hard acrylic denture with a metal framework, there are no anterior clasps. A soft acrylic flange provides the retention, fitting above the CEJ. In this case the Maxillary frenum needs to be removed to allow room for this band. Akkers #1 clasps were placed on #2,15.
PerioLase pulsed Nd:YAG was used at 3.6W 50Hz 100usec for tissue ablation.
Immediately post-lase
Insertion of the Virginia Partial

2″ target=”_blank”>https://www.laserdentistryforum.com/attachments/upload/Vonsch41805a.jpg[/img]
2 months post-op

Lab work by Lab One, Richmond, VA
Laser Perio Therapy (LANAP) will now be performed on all 4 quadrants, now that the occlusion can be relieved off #2, 15.
Jeff
SwpmnSpectatorThe WaterlaseMD has now been available for nine months. Must be quite a few clinicians using the MD. From an engineering and clinical standpoint, the unit appears to be a vast improvement over the Waterlase I leased in April 2001.
WaterlaseMD has a user selectable pulse duration – 140microsec for hard tissue and 700microsec for soft tissue. I believe the theory behind the 700microsec soft tissue setting is that a longer on time of the pulse will result in absorption of the wavelength over a larger, deeper area and thus improve hemostasis.
Since I’ve only used erbium lasers with relatively short pulse durations of 140-300usec, would like to ask Waterlase MD users:
1) Does the 700 microsecond pulse duration setting effectively control bleeding?
2) If you have used electrosurge or a diode or Nd:YAG laser, how does it compare?
3) Do you find that the MD tips become contaminated and difficult to cleanse once used on soft tissue? Particularly if used without water spray? With cleavable fibers on diode and Nd:YAG you just extend and cut so tip contamination not much of a problem.
czeqm8SpectatorThis guy is a train wreck. He has decay and pocketing. I am just trying to keep him together until he makes a commitment to his mouth.
I forgot to take a picture before I removed some of the decay, but you can see there is still plenty left.

I try to retract the gingiva to see the rest of the decay, but it is too low on the root.
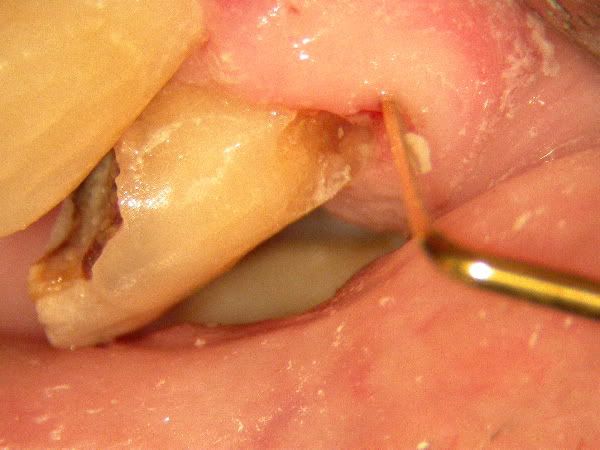
Gingivectomy and decay removed. Very close to pulp as noted by the secondary dentin around pulp.

Filled with composite.

There is no need to worry about biological width here. This guy has major pocketing all over. He knows about it too. Hopefully he will come around soon.
Matt
(Edited by czeqm8 at 11:11 pm on June 27, 2005)
-
AuthorPosts
