Forum Replies Created
-
AuthorPosts
-
AnonymousSpectatorQUOTEQuote: from Swpmn on 1:21 pm on May 4, 2006How about going back and telling us exactly what you did, settings, etc.???
Amount of time in temp?
Why do you think this was successful? Due to the missing crown and ability to get access and angulation?
BTW, awesome!
Robert Gregg DDSSpectatorThanks Glenn for the explaination. Sounds like what Eric Bornstein was discussing at the MDT meeting.
Michael–There has been no “head-to-head” comparison of any diode or diode methodology to LANAP either in vivo or in vitro except for the AADR Harris and Loomer in vitro experiement showing FRP Nd:YAG had a 16 fold lethality over 810 nm diode w/o destruction of the surrounding tissue.
In fact, I’m not aware of any human histology regarding any diode or diode methodology of any kind. A few people have reported to me that HH is being pllanned or is underway, but that’s it so far.
And other then Larry Finkbiener’s Argon study, I have not seen any cummulative data looking at clinical indices of any diode, including PAD.
Now, Dr. Eric Bornstein has some very interesting stuff regarding dyes and diodes, but no comparative info other than his Dentistry Today article that he wrote comparing the light dosemitry of LANAP and the need to use about 3 times less “light dose” using a diode in the perio pocket.
Bob
Robert Gregg DDSSpectatorHi aaroN,
Good to hear from you.
Bob, we’ve talked in the past about not using grafts with LANAP because the graft just gets in the way of healing. But, away from teeth/roots/PDL, do you expect healing to be enhanced in immediately placed implants, or socket grafts when the Periolase is used to stablize the clot? I may not be understanding the entire picture yet . . . . any information is always cherished from you!!
Yes, I expect the healing of any graft to be enhanced using a FRP Nd:YAG and the proper parameters–even away from structures that you mentioned.
Bob
Robert Gregg DDSSpectatorDavid,
We discuss this in detail at Day 4 and Day 5………….;)
I actually look at the article as movement toward eventual acceptance of laser perio.
In 1992, Cobb published 2 articles that said Nd:YAG laser burn roots, inhibit fibroblasts migration and were generally dangerous. The AAP adopted a laser Position Paper that reflected his flawed study designs.
Around 2000, Dederich published a laser review in JADA that said laser perio was no better than S/RP.
Now Cobb is saying there is “minimal evidence” for lasers perio treatments.
In January, AAP President-Elect Preston Miller said that the new lasers (i.e. Periolase) for perio treatment are worthy of looking at. His partner is a Periolase owner.
The AAP and Cobb are preparing their members for a “soft-landing” when the results can no longer be ignored or denied.
The failure to cite the Yukna abstract was a big mistake. It once again hurts Cobb’s credibility. It was a big mistake to say that only peer reviewed papers would be included, then cite a Dentistry Today article, but not all that pertain to laser perio.
Those periodontists who rest to hard on this latest Cobb paper have sand for a foundation not bedrock. If the perio folks you are talking with share the same con clusion, ask them if they also share the direction that Cobb and the AAP are moving……
A perio friend of Cobb’s and lectuer at UMKC is a Periolase owner. Cobb has follwed his results for the past 18 months. This periodontist has been so successful in clinical results (getting what we claim) and ROI as well that he is attending Bootcamps to become a LANAP instructor.
So, I’m starting to feel a bit like the Indians at the Little Big Horn listening to Custer tell his troops, “We don’t need to wait for General Reno’s reinforcements, we have them right where we want them.”
Making critical conclusions while ignoring all all the available data can be dangerous. Relying on incomplete data and accepting that at face value is foolish for professional soldiers and periodontists alike.
Bob
Robert Gregg DDSSpectatorNice David!
Bob
dkimmelSpectatorThis is a pre MD case and was done with the Waterlase. I have to say that I would do the case differently today.
First I used the Waterlase with a G-6 tip with 0.75W 0 water 30a in contact to trough around the root. I then cored and prepped the tooth. I prepped the tooth to give me 2mm of solid tooth. Since I had plenty of attached gingival I removed enough to just expose the margin of the prep. Before starting I had bone sounded the tooth as well as the tooth distal and mesial to the prep. I decided I needed to go 5mm from the new gingival margin. I marked the G-6 at 5mm. I used the Waterlase with the G-6 at 2W 20water and 40air . I worked the tip around the prep until I was at the osseous. Staying out of contact I kept moving the tip around the prep until I got 5mm . At this point I went to .75W 10water and 30air. This time I placed the tip on the bone and moved it quickly feeling the bone as I go till it feels smooth. Next I angled the tip under the tissue blunt dissecting it . Then feeling the bone to make sure I left no ledges. I bumped the watts up to 1-2 W if needed. Lastly I used a scaler to plane the root to make sure no thin layer of bone was left on the root surface. At this point with loops you can see the bone.Placing the temp was a bit tough. The patient was medically compromised and her gums on a good day bleed easily. I used the diode at 5W continues in noncontact to help with hemostatis . I don’t remember but from the look of the tissue I must have used some FeCL as well.
I did leave the patient in the temp for 3 months before the final impression. The tissue did look pretty ugly the day of the CL but the patient reported no discomfort the next few days and it healed nicely.Access was key to this case. I could have done the CL prior to the core and got better access. I wanted to know where my margin would be before I started and I was not sure I could isolate the tooth for bonding after the CL.
With the MD or even the Waterlase I would have used a Z tip. As I trashed the G tip on this case. I also would have had more tip length to work with. I also feel I needed to reduce the interprox a bit more. I am a little concerned about the look of the tissue on the mesial buccal. Then again it did not bleed after an aggressive probing.. Time will tell.Allen thanks for the comment on the crowns. I have a running battle with my lab about crowns. He say ‘s his all ceramic Cerapress looks better then his PFM’s. 20 is a cerapress and 21 is a PFM. It will be fun showing him this post-op photo.
Ron ,Bob thanks as well…
Glenn van AsSpectatorI know that Surgitel just came out with loupes inserts that apparently are fantastic.
Dont know if they fit Orascoptic.
Glenn
etienneSpectatorHi Aaron
Thanks for the compliments. I would definitely say that not only did the Nd:YAG stabilize the graft (remember, there was no membrane here) but it also enhanced healing. If you doubt that, just look at the 2 days post-op picture. As a matter of fact, grafting an infected site like that without the benefit of lasers is something I would be very hesitant to do.Placing the implant at the time of extraction/grafting? I am sure it is just a matter of time. In fact, I know of people that are doing it now. If it fails, what have you lost? Of course the risk of failure will be higher but the benefits will be tremendous to the patient if it succeeds. I suppose it boils down to informed consent.
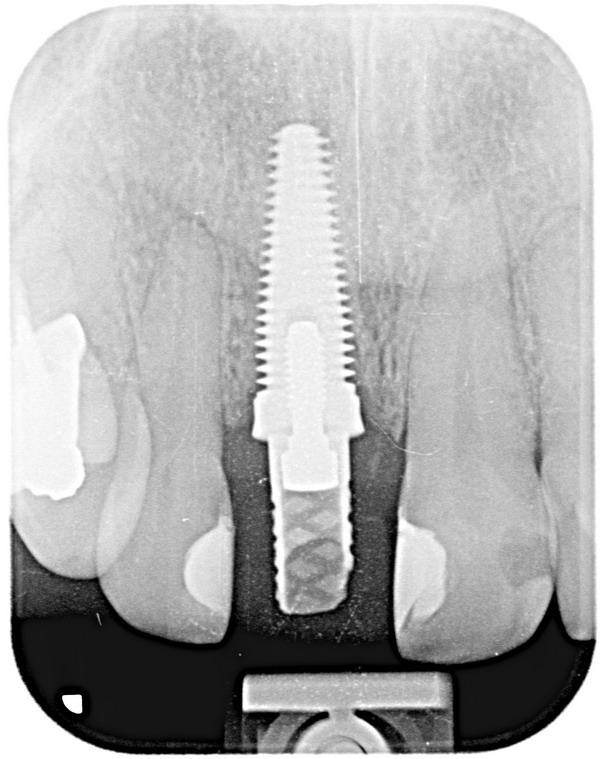
This implant is by a local company called Southern Implants. They export to the UK, Australia etc. It is called a co-axis implant due to the fact that the restorative surface of the implant is offset at an angle to make it easier to make a “screw down” crown with the access hole in the singulum area. It is threaded all the way to the platform (apart from the offset area). I have never done platform swtiching on this particular implant. Good idea.
I’ll post some pics of the graft etc.
Take care
Etienne
(Edited by etienne at 1:20 pm on May 6, 2006)
etienneSpectatorHi Aaron
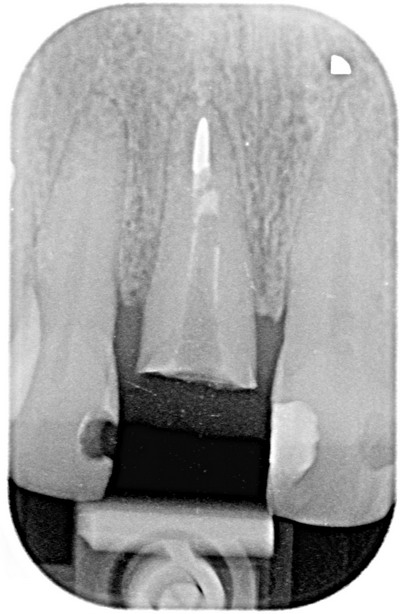
Some pictures of the grafted area and implant.This was the initial situation with cracked root and abscess.
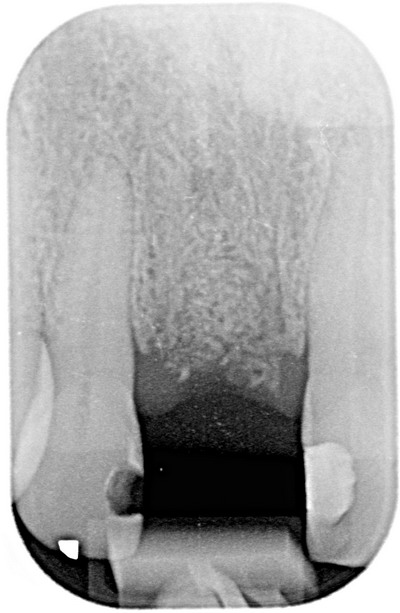
Just before placing the implant, 6 weeks after extraction and grafting.
Implant with healing abutment in place.
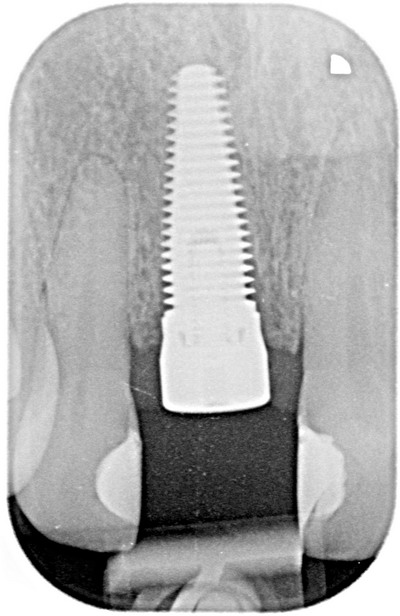
Temporary crown placed, this was taken 5 weeks after placing the implant, approximately 2 1/2 months after grafting the site.
Take care
Etienne
whitertthSpectatorI got a 45 y/o buddy who came down last week withg Bells palsy, and was thinking of trying my Laser smile ( Diode) to try and help him…Anyone know of any literature out there or has anyone seen this help/
Thanks….
BenchwmerSpectatorI had a Commentary article, “Do ALL Dentists Use Lasers” along with 2 case studies (one a three year LANAP) printed in the May issue of Dentistry Today.
Contemporary Esthetics May 2006 issue published a different one of my case studies, “Laser Assisted Extraction,Immediate Bonded Splint and Bridge Procedure”.
Let me know if anyone ever looks at these publications, what you think of the articles.
Thanks.
Jeff
cadavisSpectatorI’ve completed the training on the Sirolaser and I have to say I”m impressed with it. It’s extremely easy to use. I did an extraction yesterday on an older patient that is on meds whiich make him a heavy bleeder. I didn’t take him off the meds this time. I used the diode to create hemostasis and it worked great. I also completed a labial frenectomy on a youg girl with a large diastema. The diode cut fast and smooth. Great result. I have a post op shot of it and will be taking one and two week followup shots which I’ll try to post later. I’m not sure how to transfer our Sony Digidoc shots out of her charting and into this forum though.
Chris Davis
cadavisSpectatorI purchased the Q1000 LLLT device while at the ALD in Tucson. I’ve tried in numerous times on various things that it is supposed to be good for. Numbing pedo teeth, TMD, etc… I’ve have had no discernable success with it. Maybe poor technique, who knows. Has anyone had any success with this device?
Chris Davis
2thlaserSpectatorJeff,
Saw the first article in DT…nice. I know I read them!!I will read the CE one soon…Always nice to see someone publish on lasers, period!
Mark
Lee AllenSpectatorDavid,
Thanks for the great post-op. I need to go back to take stock of my Closed CL cases.
My technique is very similar except that I do not have a Diode (I think I just admitted to being a dinosaur). I use more water especially on the bone. I now do so after having a painful post op with a non ideal situation. It was a crowded interprox with misaligned teeth. I think there was not enough water flow onto the working tip and it got charred. The results were good, but this patient was my first to take pain meds.
I admire your results and understand the “box” you were in. Under other cricumstances, I would lay a flap. I notice patients still do not feel discomfort if incised with an Erbium and the tissues are not stretched; I get good visibility, and incisions heal side to side, not end to end. My 2 cents.
Question: Why use the Z tips? Co$t, or length = visibility and access, or personal preference.
And which tip? -
AuthorPosts
