Forum Replies Created
-
AuthorPosts
-
2thlaserSpectatorYes, it’s weird Glenn, I seriously don’t have any problems with my laser. I am now in a experimental mode, doing things that should blow the fiber, and haven’t yet, and my laser is cutting as fast as ever. I can’t figure it out. Lucky I guess. When I blow the fiber, I will document what I did to do it, but so far so good.
(I have a spare!). Anyhow, hope everyone get’s back to lasering soon.
Mark
Robert GreggParticipantHi Jeff,
Nicely said Glenn and Mark.
I had a nice discussion about this sort of thing (Waterlase is better for perio than an Nd:YAG) with Stu Rosenberg at the ALD Destin meeting. I told him that I had heard these stories second hand that Biolase reps were saying these sorts of things about perio. He appeared genuinely upset. He said to tell him if I ever learn their names and he would set them right. He said there was no room for salesreps to be mis-representing laser capabilities.
I told Rick Shock flat out that what he was saying to me (in front of another doctor) about Waterlase for perio was just the same as Nd:YAG was just plain wrong and he needed to stop saying stuff like that.
There is no excuse for any company to let loose any sales rep into the field without proper sales, product training, and message calibration. The company should have several days of sales training, a notebook, and a list of Do’s and Don’ts. If a company continuously has sales reps that are repeating the same identical mis-information, then it is not an accident, in my opinion.
At Millennium Dental Technologies, we train our sales reps and we scrutinize what our sales reps say. When they first start on with us, they are required to go through Laser BootCamp (3 days) with the rest of the doctors. They wear a suit and tie. They get the same instructions and books (3) that every doctor gets at BootCamp. Then they come back for a sales orientation meeting. They must then attend a “Preview Session” given by either Dr. McCarthy or myself. We must observe them at a trade show booth, and listen to their conversations with prospects. Then, when we feel they are “on message”, we give them a computer with a PowerPoint presentation that we developed, that is scripted for accuracy and FDA compliance. Still, they are not allowed to give presentations without a doctor/LPT dentist present, unless it is a one-on-one with a doctor in their office.
Unfortunately, I have spoken to several Waterlase users who bought it because they were told they could in fact perform periodontal treatments with their Waterlase, and in turn have told me they tried it, and it just didn’t perform. They aren’t just disgruntled about the misrepresentation from one company, they suspect that those companies that are careful with their sales message, might also be “stretching the truth”. That, and the harm to patients, is the real injury when reps say those things.
Now on a personal note (and here’s how you answer Jeff):
How does this sales rep reconcile:
1. That MDT’s laser–called the PERIOLASE (duh!)–an Nd:YAG, was developed SPECIFICALLY for use in the periodontal pocket?
2. That MDT has the first USPTO patent for a laser periodontal procedure–using an Nd:YAG?
3. That MDT has FDA clearance for safety and efficacy for Laser curettage, sulcular debridement, and LPT, respectively (removal of diseased or inflamed soft tissue in the periodontal pocket) to improve clinical indices including Gingival Index (GI) – improving the quality, quantity, and severity of disease; Gingival Bleeding Index (GBI) – reduce bleeding from the gums; Probe Depth (PD) – reduce the depth of the periodontal pocket; Attachment Level (AL) – increase the level of tissue attachment; and Tooth Mobility ™ – lessen loose teeth? Center for Devices and Radiological Health, Food and Drug Administration 510(k) # K010771 November 27, 2001 & #K014272 March 28, 2002:
4. That the “hot-tip” effect is used with diodes, not Nd:YAGs in the periodontal pocket.
QUOTEEvery time I talk to a BioLase rep or someone who sells Diodes, the Nd:YAG has the properties of a diode, and the Diode has all properties of a pulsed Nd:YAG.They are simply as wrong as they can be. That’s like saying a diode has the properties of an Erbium laser–it’s so absurd on the face of it as to be laughable.
Diodes are Continuous Wave (CW) lasers. They ONLY work on soft tissue.
Nd:YAGs are “Free-Running” (FR) or 10-6 (millionths) seconds pulsed lasers and interact on HARD and soft tissues both. The ONLY tissue Fr pulsed Nd:YAGs will not interact with is healthy enamel. Diseased enamel, de-calcified enamel, dentin, decay etc with be vaporized by a pulsed Nd:YAG.
Pulsed Nd:YAGs are more like erbium’s than they are like CW diodes.
But imagine if anyone from MDT was to suggest that erbium’s are like neodymium’s in they both do the same thing. Besides firing the sales rep who should say such a thing, we would loose all credibility.
For lasers to make a long lasting impression and have wide-spread adoption in dentistry, the purveyors of the technology must have integrity and credibility. After Jeff’s experience last night, I think we can understand where some companies are in terms of their longevity factor. That, not millions of dollars in sales, will determine the survivors in this field. Substance or slander, science or hype–the individuals at the top of the companies set the tone, and establish the “Corporate Culture”, and the sales messages.
Bob
whitertthSpectatorBob, I agree with alot of what you are saying but I must respectfuly disagree with one thing…I am not talking scientifiacally now since i am am a clinician and not a scientist, clinically the waterlase is wonderful for sulucular decontamination. I have not had one perio case not improve dramatically using my waterlase. while I am not comparing it to the Periolase, as I know u guys have a great product, personally i dont value another laser investment at this time for a “soft tissue laser” wether it be a diode. Nd yag, etc since I get incredible soft tissue results virtually 100 percent of the time with my waterlase with the obvious benefit of its abilty to cut hard tissue as well….Just my 2 cents
whitertthSpectatorIn my lectures that I give i have routinely said and i firmly belive that while there hasnt been any laser thus far that is great at doing everything, the waterlase comes pretty damn close to being the catch all of lasers at this time. As far as no anaesthesia, i see it as a tremendous benefit in the acceptance of treatment. many patient would opt for a virtually painless procedure without anasthetic than one with local. I am not condoning what any sales rep here is saying. facts must and i mean must be spoken. But, The waterlase really is all its cracked up to be. Anyone not getting great soft tissue results just isnt trained properly..If u r having trouble e mail me or call me at my office 516 239 6204 and I will try and assist you anyway I can .
whitertthSpectatorhit them over the head with a sledge hammer?
BNelsonSpectatorHi All,
Having invested in a Waterlase because it “can do everything” I have to admit that I was not as well informed as I should have been. Now that I have learned alot more about laser physics, it’s obvious that one wavelength isn’t going to be the best for everything. I do a varied number of procedures with the Waterlase and routinely recontour tissue around Cl V lesions very nicely, but now that I have a Periolase I vary my laser usage considerably more. In my practice I personally am having more fun with the Periolase and treating periodontal disease than treating decay with the Waterlase. Bob’s LPT procedure is absolutely amazing to see. The results have been incredible and the patients love it. Attempting to treat inflamed 8-10 mm pockets with an Er is not even close. But the comments about sales persons is very correct. Many will “stretch” the truth to sell you. Get educated and make your own decision on the facts. Then go have a lot of fun impressing patients with the incredible new techniques you can perform.
Robert Gregg DDSSpectatorThanks Ron,
“I must respectfuly disagree with one thing…I am not talking scientifiacally now since i am am a clinician and not a scientist, clinically the waterlase is wonderful for sulucular decontamination.”
I appreciate that, Ron. And I appreciate your perspective. Nice thing about this forum is we can share our different perspectives.:)
“Sulcular decontamination” (SD) is one thing. And I completely agree with you that erbium lasers kill bugs in the perio pocket. I have the references to show that. No arguement there. But sulcular decontamination is just one component of treating the periodontal pocket. Right? I mean, what’s the plan for the root surface acretions? How about a stable fibrin clot?
Anyway, SD is not what was apparently represented by the sales rep according to Jeff:
“He commented that this technique is better than any other laser Perio treatment because you don’t have to use any anesthetic.”:confused:
I’m sorry, but that just isn’t true.
Based on 12+ years of treating all types of perio using all types of techniques and lasers, there is nothing that “is better” or equal to treating periodontal disease–Case Types I-IV–as a stand alone periodontal procedure (with FDA clearance by the way) than a properly configured pulsed Nd:YAG and “LPT”.
We have the basic science, the clincial results, the retrospective, multi-center clinical data, and the human histology to make that statement. Erbiums do not have this sort of perio science at this time.
And that’s part of the problem I have with companies, and their sales reps when they make bold comparison claims that aren’t supported with science or even facts.
While Del McCarthy and I spent 10 years doing the science on lasers (all types, including erbium) for periodontal disease–manufacturers of erbium lasers were developing their devices and doing the science for dedicated HARD tissue removal. Fine! Cool! Great! We’re are happy for that. :cheesy:
Hard tissue clearance for enamel and bone removal has greatly advanced the field of laser dentistry. So has our development and FDA clearances for perio tissue regeneration.
But erbium device manufactuers and their sales reps should not now come along and make unsubstantiated claims that an erbium laser “is better” than those devices that actually have done the clinical and histologic research. That’s not fair, it’s inappropriate, it’s not factual, and it may even be harmful to patients. The manufacturers need to spend the time and money that we have done, get their own data, then make their claims. To do make exaggerated claims, false comparisons, or disparage other devices is just not going to advance the adoption of lasers in dentistry.

And with erbiums, at this time, no one knows what the tissues are that “re-attaches” to the tooth, whether it is new attachment, long junctional epithelium, or ankylosis.:confused:
With pulsed Nd:YAG, using our laser lconfiguration and patented periodontal treatment methodology, we know from controlled university human histology that we are getting new attachment. Just as importantly, we know there is absolutely no, nada, zip, ziltch damage to root surface or pulp from the “hot-tip” or any other such false attribution that is often made about pulsed Nd:YAG.
I’d be happy to send our research to you, Ron, or anyone else who’d like to receive them. Just send me a private email with an address.
As and side, does anyone know why it is called “sulcular decontamination” and not “pocket sterilization” anymore? Yep, cuz we ain’t killin’ 100% of the bugs. Kill rates….and kill depths are determined by a number of factors:
1. Wavelength which defines depth of penetration/absorption into tissues. Nd:YAG penetrates deeper into tissues than erbium. Right?
2. Temporal emisson mode “TEM” (e.g. free-running pulsed versus CW or gated pulse) which defines intensity, and therefore the strength of the wavlength’s effect (at depth or at the surface of tissue).
3. Pulse duration which further defines the depth of penetration/absorption of a “true-pulsed” (i.e. free-running) per pulse.
But killing bugs in the pocket-space (sulcular decontamination) is not the only place that bacteria reside in perodontal disease-infected tissues, nor is that the only requirement for the successful and safe regeneraton of the periodontal attachment apparatus (say versus long junctional epithelium or ankylosis of bone to root.
And I have a substantial disagreement that early to advanced periodontal disease can be properly treated w/o anesthetic. For those that don’t remember what went on 13 years ago, when pulsed NdYAGs first came out, we were the first champions of pocket sterilization, laser curettage without anesthetic. Dr. McCarthy, and the early pioneers like Dean McDaniel, Hector Martinez, Tom Pikar (Canada), Tom Branham, Terry Myers and others (12 all told) were the very first to develop this approach. Many still use it. None have the results or success that they do now using our anesthetic LPT methodolgy–and McDaniel, McCarthy, Branham are doing the LPT protocol now….But if you have never seen what can optimally be accomplished, then I unerstand why good results (better than non-laser) look great.
QUOTEpersonally i dont value another laser investment at this time for a “soft tissue laser” wether it be a diode. Nd yag, etc since I get incredible soft tissue results virtually 100 percent of the time with my waterlase with the obvious benefit of its abilty to cut hard tissue as wellI guess I’m not very good at explaining that the free-running pulsed Nd:YAG is a HARD tissue laser, not merely a “soft tissue laser”, and is not in the same category as a diode, anymore than a free-running pulsed erbium is in the same category as a CW diode……..oh well. Maybe when I can get my digital, scope mounted camera taking decent pictures I can better demonstrate the hard tissue capabilites that FR Nd:YAGs have. But don’t expect our sales reps or any of us saying a pulsed neodymium “is better” than free-running erbiums for undefined “hard tissue” applications–even though there are quite a few.
QUOTEAnyone not getting great soft tissue results just isnt trained properlyAgreed. And what training is required by laser manufactureres before their laser is shipped? None–unless you are an MDT customer. We require 3 days of basic didactic and clinical hand-ons, live patient training before we will ship the PerioLase MVP-7. It’s was named “Laser Bootcamp” by our doctors who first went through it many years ago.
Thanks Bruce, too. I think your perspective is valuable since you own both the Waterlase and the PerioLase MVP-7, and you have been through both company’s training programs.;)
All the best,
Bob
(Edited by Robert Gregg DDS at 11:46 am on May 8, 2003)
whitertthSpectatorBob, Please dont misread me, I know you have a wonderful product. I applaud how much importance you guys place on training. That still is a major problem in this industry( the lack of training). I will pose a question though…If someone is treating perio with an erbium and clinically seeing great results ie, reduction in pocketing, no bleeding, pink tissues etc where is the value for that doctor to purchase an ndyag laser.. not being argumentative here just curious…..all the best
Robert GreggParticipantRon–
Thanks for the kind words.
I know you’re not trying to be argumentative. I hope we are having a good and “enlightening” discussion–just coming from different perspectives.
I understand your question. And it’s a fair question. But I think it assumes a few things, like–the location in the mouth of teeth being treated, the severity of disease, the depth of the pockets treated, the number of times a pocket is treated, and the results are the same with both devices and techniques. So let me ask you:
1. What kind of perio pocket depths are you treating? 5mm? 10mm? 20mm?
We treat shallow to 20+mm pocket depths routinely.
2. Are you treating acutely inflamed as well as chronically inflamed tissues?
We treat all types and severities in one visit with speed and efficiency.
3. Do you get instant hemostasis so a stable fibrin clot can form? (Important for regenerative potential and long term stability)
We do by varying 7 different pulse durations in the PerioLase.

The left photo is a Pre-Op with 11 and 12mm pockets and extensive hemorrhaging during S/RP phase of LPT. The right photo is 4 minutes Post-Op4. How does your fiber-delivery system get to the distal aspects of 2nd and 3rd molars?
We treat every pocket, of every tooth, of every patient.
5. How many times do you have to treat a Case Type IV perio patient?
We treat only one time, regardless of whether the pocket depths are 9 or 19mm in the same patient.
[img]https://www.laserdentistryforum.com/attachments/upload/Saxon composite Pre & Post-op.JPG[/img]
The mesial defect in the left x-ray was 19mm, and the distal defect was 16mm. The x-ray on the right is a 9 month post-op of the same tooth after only one treatment
6. What sort of pocket depth reduction, bone density increase are you getting when treating case type III or IV?
Peer reviewed, retrospective, blinded, multi-centered, private practice clinical study study of 65 patients and over 1900 probing sites showed that laser periodontal therapy using a specific modality called “LPT” for “Laser Periodontal Therapy” was reproducible in reducing 90% of pockets without any recession in ONE treatment by a minimum of 50% regardless of pocket depth as such:
> 4mm – 2.2mm reduction
> 6mm – 3.1mm reduction
> 8mm – 4.5mm reductionhttp://spie.org/scripts/abstract.pl?bibcode=2002SPIE%2e4610%2e%2e%2e49H&page=1&qs=spie
5. What is the mid-term stability of those pockets at say 24 months?
Our LPT treated pocket are stable at 24 months and beyond.
[img]https://www.laserdentistryforum.com/attachments/upload/Saxon Compositea.JPG[/img]
Same tooth as the above x-ray over a 24 month time frame
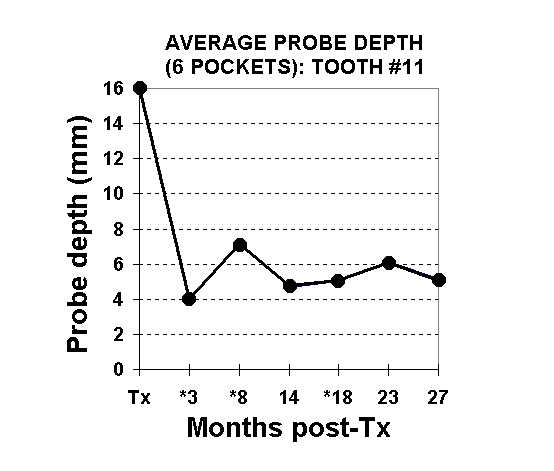
Same tooth with average probe depths charted over 27 monthsI’m responding only to your question about clinical results. Like I said in my earlier post, if all I had was an erbium, and I saw better results than I saw pre-laser use, then I would conclude as you have that I had a pretty neat instrument. And I am sure that it is for some applications, but not for all perio case types, or as a complete protocol and procedure.
There are lots of legal reasons why you might want a dedicated “perio” laser and an FDA cleared perio protocol for treating perio disease.
FDA cleared “Laser Periodontal Therapy”:
1. Defines a specific protocol for scientific research. (“sulcular decontamination” does not)
2. Standardizes training and calibrates academicians, researchers and clinicians. (“sulcular decontamination” is done with great variation in technique—no standardization in parameters or technique)
3. Is a defined protocol for efficacy and patient safety in clinical practice. . (“sulcular decontamination” has no defined, that is standardized protocol)
4. Has the power of Federal Regulatory authority behind the clearance. (Important legal status that “sulcular decontamination” does not have)
5. FDA clearance is recognized by State Boards (Important for State Board inquiries for some clinicians over the years—in Florida no less)
6. Provides legal basis for defense in professional liability claims – i.e. is legally defensible in a malpractice claim.
7. LPT is now a legitimate option for periodontal informed consent when offering traditional surgery. (“sulcular decontamination” is not)
8. LPT is not just the only FDA cleared laser periodontal protocol – it is the only FDA cleared periodontal disease treatment protocol for treatment of the full mouth.
But if we take your position one step further removed, one might also ask, “If I have a 踰 high speed handpiece that cuts everything including gold, amalgam, porcelain, bone and does so faster, cheaper (if not better) than a โ,000 dedicated hard issue laser that cannot cut amalgam, gold, or porcelain, then why would I want to invest in that??
Of course I would get quite a reaction from this group. And rightly so, because there’s a lot of other value-added aspects to a hard tissue laser than just the cutting speed and materials limitation that make it a valuable investment.
Invest in the optimal laser for the clinical requirments and demands, and don’t try to force a square peg into a round hole…….You don’t want someone to try LASIK on you or a loved one with a laser that wasn’t optimized for it–but a salesman said, “It’s just as good as an eximer laser!”
Best regards,
Bob
(Edited by Robert Gregg at 4:08 pm on May 8, 2003)
Robert GreggParticipantAnd a hearty welcome to Kim Stevens, RDH of Dr. Craig Long’s office. Thanks for signing up! Check through the site and see what’s going on.
I guess we’ll be seeing you soon for your Day 4 training session!
See you then.:biggrin:
Bob
Andrew SatlinSpectatorBob,
A technique to close black triangles? Wow is right!!
Can you give some more details? I would love to here about it.
Andy
dkimmelSpectatorBeen trying to use the Lasersmile more often. Been doing the decontamination and the degranulation as shown by the trainers. Have seen some nice results with a couple initial patients.
Had a patient this week that need periodontal sx. I did the degranuation on selected sites. Then flapped using the Lasersmile. I was rather surprised by the amount of granulation tissue still present. The tip was activated and with an open flap it still took a while to degranulate the area. Makes me wonder about my other cases!
Anyone seen this?
DAvid
RodSpectatorI just got Jim Jesse’s DVD on the Waterlase. TWO BIG THUMBS WAY UP FOR THIS!
There are no two ways about it — if you’re reading this post, and even THINKING about getting a Waterlase or other hard tissue laser, or if you already have the Waterlase or hard tissue laser, this DVD is an ABSOLUTE MUST.
Think about it….the Waterlase is a big investment. My newest book tells ya how to make a HUGE profit/ROI from it, but it doesn’t go over the fine points of using it. Jim’s DVD goes through all sorts of techniques using the Waterlase.
There are several things that I do differently from Jim, but hell, that can be said of all of us. The point is that it does a great job of showing you how the soft/hard tissue lasers can be used.
If you’ve already made the investment of a hard/soft tissue laser, you’d DARNED WELL BETTER get this DVD and pick up numerous valuable pearls you can use.
I watched it THREE TIMES on Tuesday, and already used SEVERAL of the pearls I picked up.
The thing sells for the ridiculously low price of only 趚. This cost Jim BIG BUCKS to make. This is a great price, and you can NOT afford not to get it.
Order it by calling (909) 940-1158.
And NO, Jim’s NOT giving me a ‘cut’ of the sales. I just hope he’ll at least make some profit after all his hard work. Great job Jim!! Thanks for the great insights.
Rod
Rodger ‘Rod’ Kurthy, D.M.D.
Author of:
The No-Coupon ‘Marketable’ Dentist
So Rod…Should I REALLY get a laser?
Rod…HELP!!!! Teach me how to make some MONEY with my laser!
(Books offered at [url=”http://www.NewPatientsInc.com)”]www.NewPatientsInc.com)[/url]
kellyjblodgettdmdSpectatorThanks, Ron. I usually save the sledge hammer for collection issues.
Robert Gregg DDSSpectatorFinally! Three years after beginning the human histology at LSU with Ray Yukna, the study has been published! It will be presented this June at the International Association of Dental research (IADR) in Sweden. It’s on-line at:
http://iadr.confex.com/iadr/2003Goteborg/techprogram/abstract_34208.htm
1735 Laser-assisted Periodontal Regeneration in Humans
R.A. YUKNA, G.H. EVANS, S. VASTARDIS, and R.F. CARR, Louisiana State University, New Orlreans, USA
Objective: The Laser Assisted New Attachment Procedure (LANAP) has been advocated for the sulcular debridement of periodontal pockets with the goal of obtaining new attachment. Clinical case reports have reported favorable clinical results, but there is no human histologic proof of regeneration.
Methods: 3 patients with 2 single-rooted teeth with moderate-advanced chronic periodontitis associated with subgingival calculus deposits were enrolled. Occlusal adjustment and direct bond extracoronal splinting was performed. Under local anesthesia, a 1/4 round bur notch was placed at the apical extent of calculus as carefully as possible. One of each pair of teeth received Nd:YAG laser treatment of the inner pocket wall to remove the pocket epithelium (laser settings were 3 watts, 150 pulses/second, 10 hz). Both teeth were then aggressively scaled/root planed with an ultrasonic scaler. The pocket of the test tooth was lased again to coagulate any blood present and to form a pocket seal. Triple antibiotic ointment and a light cured dressing was placed. Control teeth received all of the above except the laser treatment. The patients were seen every 10 days for the first month, then at 2 and 3 months, at which time the treated teeth were removed en bloc for histologic processing. Decalcified step serial sections were stained with H & E.
Results: 2 of the 3 LANAP treated specimens showed new cementum, new bone, and new periodontal ligament in and coronal to the notch. The control teeth had a long junctional epithelium with no evidence of regeneration. There was no evidence of any adverse pulpal or tooth surface changes in either specimen.
Conclusions: This report supports the proof of principle that LANAP can be associated with periodontal regeneration on a diseased root surface in humans.
Supported by Millennium Dental Technologies and the Louisiana Periodontics Support Fund.
Seq #178 – Therapeutic Intervention – Adjunctive Treatment 11:00 AM-12:15 PM, Friday, 27 June 2003 Svenska Massan Exhibition Hall B
Back to the Periodontal Research – Therapy Program
Back to the 81st General Session of the International Association for Dental Research (June 25-28, 2003)
-
AuthorPosts
