Forum Replies Created
-
AuthorPosts
-
whitertthSpectatorno I didnt place it but tissue grew over cover screw as we elected no healing abutment due to the lack of space under patients ortho retainer….
cerecdocSpectatorWhat’s “mj” I have a watt setting, and a water and an air setting, with four memory presets. On my waterlase.
cerecdocSpectatorYou said 5.5 watts defocus. At what distance from the tooth is defocus. And what is the air and water setting.
I zapped my palm pretty good at 6 watts and no water about three inches away with my waterlase the other day. I can hear you laughing!
Please spell it out so a dummy like me can get the details.
My training on anesthesia was about .5 watts about 10mm from the tooth with no air or water to speak of.
There is a big difference between 5 watts and .5 as I was trained to do. What am I missing?
Glenn van AsSpectatorRon: CLAP CLAP CLAP……..nice stuff and well handled.
I like what you did.
If I can make one suggestion about the pics, when you take mirror pictures it reverses the pics so if you look at the first two pics they look like the are the right lateral but in fact it was the left lateral.
If you get a cheapo editing program……..ADobe LE or I use ACDSee 5 you can quickly flip them and then not worry about printing them or having them look backwards.
I dont want to sound like I am nitpicking because with such nice pics I want you to be able to show EVERYONE!!
Way to go………
Glenn
Glenn van AsSpectatorHi there………you get wattage by multiplying
Mj (millijoules) with Hz (pulses per second)
The continuum has 5 Hz settings but Biolase has 1 setting of 20 pulses per second or 20 Hz.
Continuum has 3,10,20,25,30.
I like this ability to change the number of pulses per second both higher and lower but I digress.
If I hit a tooth 30 Hz (30 times per second) at 60 mj (millijoules) the wattage is 1.8 watts (1800 milliwatts)
With the Biolase I have only 20 Pulses per second so to get 1.8 watts the actual millijoules is 90 (20X90)
Since Biolase doesnt let you control the pulses per second (its fixed at 20) the wattage is the only figure they give.
Now heres some food for thought……..
1.8 Watts can be.
3 Hz 600 mj which would be a hammer hitting you 3 times per second.
10 Hz at 180 mj ( which is still pretty strong but not often enough pulses to cut fast) (most lasers in japan are only 10 pulses per second so they are slower)
20 Hz at 90 mj ( Biolase setting)
30 Hz at 60 mj ( my setting for cementum abfractive lesions which are moderately sensitive).
I like using the 3 pulses per second on my hand to show kids how it goes pop pop pop and doesnt cut through my hand.
The Biolase can only pulse at 20 times per second.
The theory behind this is that there are two factors affecting pain……
1. Tissue relaxation time ( time between pulses ) so with pain with the continuum I can lower the number of pulses per second.
2. Duration of each pulse. Its my understanding that Biolase has a shorter pulse duration (its quicker I think) than Continuums.Bob the resident guru will correct me but I wanted to help clarify why the Biolase has only wattage posted (you can only control the energy not the number of pulses per second) whereas with the Continuum you can alter both energy (mj) and the repetition rate (Hz) and if you multiply the two you get the wattage.
I hope that I have not totally confused you , because I have managed not to confuse myself!! and thats something!!
Grin
Glenn
gwmilicichSpectatorGlen
That is as clear as mud :-)))))Very succinct and easy to grasp.
Cheers
Robert Gregg DDSSpectatorGlenn–
You give me all sorts of warm fuzzy feelin’s when you talk math like that!:cheesy:
There are laser parameter relationships that manufacturers have to select and program into a laser’s software power “matrix” as part of the laser’s original design. These parameters include Watts, Hz, and millijoules for a given pulse duration.
The fundamental relationship used in microsecond (free-running) lasers is what Glenn so excellently described:
Watts (is the “average power” on the console) = pulse energy ( usually expressed as 1/1000 of a Joule or milli-joule) x the pulse rate (Hz or aka pulses per second/pps)
Now EVERY laser that operates in the “free-running”emision mode MUST have these parameters defined inside the software matrix of the lasers’ computer. This includes the Waterlase, the DELight, the OpusDent, the PerioLase, the Pulsemaster, etc.
However, NOT every laser puts these parameters on the console display for the clinician to view. For example, neither the Waterlase nor the DELight displays the pulse duration. However, the PD has a very important role to play in tissue interactions (though engineers often don’t think so).
According to Manni’s reference, the Waterlase has a pulse duration of 140 usec and the DELight is 300 usec, so the Waterlase has roughly 2’x the pulse energy at 20 Hz at a given Watt as does the DELight.
FWIW, I have VERY strong feelings about this as I feel that lack of complete laser parameters and power emission display discourages understanding of one’s laser and delivery of energy to tissue and prevents ease of discourse of the subject of similar lasers and their effects in tissue. Hence, we end up relying on, “Well it seems to work for me, I don’t know why you are having problems at that power?” How does that advance the science and understanding of laser use once we get past the initial excitement over their early use?
Just as Larry got confused initially, others can become discouraged permanently.
All the device information about your lasers are supposed to be described in the operator’s manual delivered with your laser. If not, insist on them from the manufacturer.
Bob
PatricioSpectatorMark,
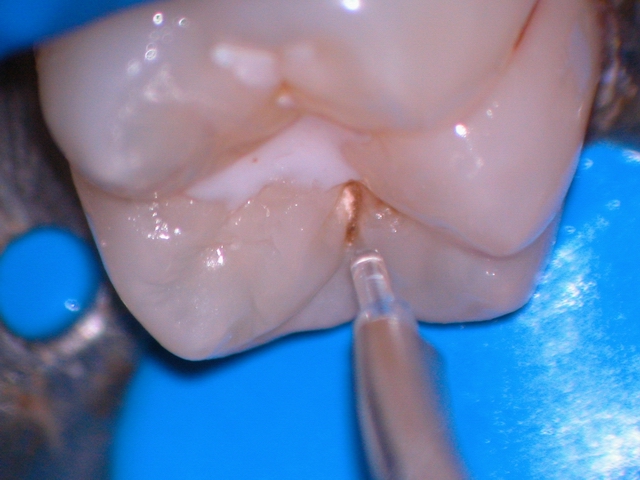
This patient is a young man of about 30 who seemed a little bit on edge and readily sensitive to limited contact with the laser and the small round bur. The area in question was a fracture site on the facial occlusal aspect of the distal facial cusp. From the coloration of the dentin I would say there had been a crack which finally gave way to a fracture. No obvious wear facets. Normal tissues and no other restorations. This area had been repaired twice before. The previous preparation was very minimal which makes me wonder if this was due in part to his sensitivity. He wanted an gold inlay but decided he could not afford one at this time so I, hopefully, improved the potential for the composite restoration with the laser and some retention.
whitertthSpectatorthanks for the info..I am still a digital photo idiot and learning everyday….I still even have trouble posting on this site sometimes but learnnig…which program do u think is best…I se image expert but dont know if that is sophisticated enough….
Glenn van AsSpectatorHi Ron , with the level of pictures you are taking often the only things you need are resize , crop, perhaps some minor editing things and rotation (flip and rotations) .
If you are really a guru , photoshop is a great program but very intense and expensive.
If you want a basic program for editing , sharing , printing and organizing your photos ACDsee 5.0 is good.
You can find them at http://www.acdsystems.com and they used to have a 30 day trial download that was kinda cool to try and see if you like it. Its around 70-100 bucks if you want the program and I like it and thats what I post all my pics on is their server (Sendpix).
Try it and see if they have a download.
Glenn
2thlaserSpectatorHi Pat,
One of the things I have noted over time is that teeth with fractures, crazes, and especially worn areas due to bruxism, have much more sensitivity than most with the laser. In addition, it seems that lower molars especially are more prone to extra sensitivity. I usually make sure I anesthetize with at least 5.5W for almost 2 minutes, BUT if the patient is already “jumpy”, or as you say, a little on edge, they expect pain, so, I just numb them anyway, as I have learned the hard way. They may not be feeling anything, but their PERCEPTION is that of discomfort, and there is no winning in that situation as you found out! I wish I could tell you I have had no problems in that regard, but I can’t. I think if you would have just tapped gently with an explorer on his tooth, he would have reacted, and sometimes I do just that to “test” the patients expectations before I even start. As far as the improved potential, you are right, the composite will have good retention from the laser prep alone as well as the bonding agents too. You did good, as usual, caring for your patient. Sorry I couldn’t help you along any further. Bob, what are your thoughts as you read this thread? Glenn? Ron?
Mark
PatricioSpectatorMark,
Thanks for the help. I will beef up my watts next time but it sounds like I proceeded with a similar thought pattern. I have done a few kids of late. What a piece of cake.A fellow asked me today if I could do his crown prep with the laser. Imagine that.
My fiber optic cable began leaking water backwards, dripping at the base. I tried the Tech’s remedies but the leaking continued. I began to panic like if you found your arm was missing. Then I remembered I have two spare cables in the basement. I ended up with them after some early problems with my new laser. I don’t know what one costs but I can recommend having an extra one on hand. We were back in business in about 15 minutes.
Thanks again.
Pat
Glenn van AsSpectatorHi folks………here is one from today that I did with anesthetic. It was a biggie for me. THe patient was biting it all the time……..
It was a fibroma removal where the fibroma was 6mm in diameter and close to the commissure of the lip. It took around 30 secs to cut through it. I did use anesthetic for two reasons…..
1. It helps with hemostasis if you use the erbium.
2. The patient was very very nervous about feeling something. I think you can try these without anesthetic using EMLA but its tough to grab the fibroma with a hemostat and separate it from the underlying tissue.Well here is the link and I hope you enjoy it……
http://www.sendpix.com/albums/021217/2007520000029d37e47ce33e23661e/
If you care ( its not something I am big on) the fee for this service was around 250 dollars and the actual work took me very little time its the comforting of the patient , preop and postop that adds to it……(I gotta do something for the money I guess !)
Remember that is Canadian though so its probably worth a dime US!!
Grin
Glenn
I am gonna post a frenectomy case I did a month ago and show the healing as I took the braces off today.
Man I have been doing alot of soft tissue stuff this week.
Glenn van AsSpectatorHi guys……..reading dental town tonight the laser guys are posting.
One of the interesting things is that many users when they first start using a laser complain that it isnt cutting or that they are breaking tips.
One of the most important things in my mind is magnification. Mark uses 6X loupes, and soon a scope. I use a microscope which is often at 10-16X power, and it allows me to see beyond the water, to focus on keeping the tip at the optimum point away from the tooth to cut fast but not damage the tip prematurely. I do believe that 2.5X loupes as a minimum will really help you and that the higher the mag the easier it is to use the laser effectively.
I was looking through old photos tonight and I have literally thousands and stumbled upon this one and thought to myself this.
Without the tactile sense we all develop with handpieces in both low and high speed, lasers require much more visual clues to evaluate how we are cutting. The importance of vision for effective cutting is not related to whether you wear glasses or not.
The resolution of the human eye is 200 microns and the Continuum tips are either 400 or 600 microns, clear quartz , and have alot of water spray cooling them and they are required to be a set distance away in thin air from the tooth to cut ( with Continuum it is 0.5-1mm)…….
Hmmm………wonder why some people have trouble seeing it cut.
For those of you using loupes, tomorrow take an extracted tooth, put on the patients safety glasses and try to cut a prep. You will find yourself to be ……..slower, cutting a much bigger prep than necessary and frustrated.
i know because I had a fellow from Iran in the office trying to use the laser last week and he saw me use it on a patient under the scope ( he watched on the monitor) and then we used it without the scope……….he told me……..hmm……….it isnt cutting as fast as when you used it!!
Nothing had changed!
Heres the pic and let me know what you are using for magnification and what it has done for you.
Oh heck I am biased towards the scope and the benefits of magnification for ALL dentistry , and hopefully when Mark starts using the scope he will see the value that I see.
Take care and as I have mentioned many many times, I value your tips here and your friendship, and in this season of joy I wanted to wish you all a most happy, safe and enjoyable holiday season.
Glenn
Glenn van AsSpectatorAw darn it all the first image was too big……….here is the resized one at 640 by 480……….
Take care………
Glenn
-
AuthorPosts
