Forum Replies Created
-
AuthorPosts
-
BenchwmerSpectatorI’ve use the same laser.
You didn’t mention settings, duration, pulse width.
The lowest power that does the job, there should be not charring, or tooth changes.
Do you check your power at the tip with a power meter?
Machines can vary by 20% over or under machine settings at tip.
When is training? Be careful.March 10, 2003 at 12:40 am in reply to: low level laser therapy for pulpitis and healing of oral sur #10667
AnonymousSpectatorQUOTEQuote: from Benchwmer
I use one of my lasers for decontamination and coagulation after every extraction. No calls at home for post-ext bleeding, No dry sockets in 3 years.
.Hi Jeff,
It was great meeting you and the others at ALD. How’d the presentation go? Wished I could have stayed to see it.
Would you be willing to share which laser,settings and /or protocol you use post extraction?
I’m sure you piqued everyone’s interest.
Thanks
AnonymousSpectatorIn light of the hydrokinetics discussion, I thought this might fit in well in this thread.
Lasers in Surgery and Medicine
Volume 31, Issue 3, 2002. Pages: 186-193Published Online: 10 Sep 2002
Copyright © 2002 Wiley-Liss, Inc.
Article
Mechanism of water augmentation during IR laser ablation of dental enamel
Daniel Fried, PhD 1 *, Nahal Ashouri, DDS 2, Thomas Breunig, PhD 1, Ramesh Shori, PhD 3
1Department of Preventive and Restorative Dental Sciences, University of California, San Francisco, San Francisco, California 94143
2Department of Growth and Development, University of California, San Francisco, San Francisco, California 94143
3Department of Electrical Engineering, University of California, Los Angeles, Los Angeles, California 90095email: Daniel Fried (dfried@itsa.ucsf.edu)
*Correspondence to Daniel Fried, Department of Preventive and Restorative Dental Sciences, University of California, San Francisco, 707 Parnassus Ave., San Francisco, CA 94143.
Funded by:
NIH/NIDCR; Grant Number: ROI-DE14554, R29-DE12091, T35-DE07103
DOE; Grant Number: DE-AC03-76SF00098Keywords
erbium laser • CO2 laser • dental enamel • laser ablation • infrared spectromicroscopyAbstract
Background and Objectives
The mechanism of water augmentation during IR laser ablation of dental hard tissues is controversial and poorly understood. The influence of an optically thick applied water layer on the laser ablation of enamel was investigated at wavelengths in which water is a primary absorber and the magnitude of absorption varies markedly.Study Design/Materials and Methods
Q-switched and free running Er: YSGG (2.79 m) and Er:YAG (2.94 m), free running Ho:YAG and 9.6 m TEA CO2 laser systems were used to produce linear incisions in dental enamel with and without water. Synchrotron-radiation IR spectromicroscopy with the Advanced Light Source at Lawrence Berkeley National Laboratory was used to determine the chemical changes across the laser ablation profiles with a spatial resolution of 10-m.Results
The addition of water increased the rate of ablation and produced a more desirable surface morphology during enamel ablation with all the erbium systems. Moreover, ablation was markedly more efficient for Q-switched (0.15 microsecond) versus free-running (150 microsecond) erbium laser pulses with the added water layer. Although the addition of a thick water layer reduced the rate of ablation during CO2 laser ablation, the addition of the water removed undesirable deposits of non-apatite mineral phases from the crater surface. IR spectromicroscopy indicates that the chemical composition of the crater walls deviates markedly from that of hydroxyapatite after Er:YAG and CO2 laser irradiation without added water. New mineral phases were resolved that have not been previously observed using conventional IR spectroscopy. There was extensive peripheral damage after irradiation with the Ho:YAG laser with and without added water without effective ablation of enamel.Conclusions
We postulate that condensed mineral phases from the plume are deposited along the crater walls after repetitive laser pulses and such non-apatitic phases interfere with subsequent laser pulses during IR laser irradiation reducing the rate and efficiency of ablation. The ablative recoil associated with the displacement and vaporization of the applied water layer removes such loosely adherent phases maintaining efficient ablation during multiple pulse irradiation. Lasers Surg. Med. 31:186-193, 2002. © 2002 Wiley-Liss, Inc.
Accepted: 7 May 2002March 10, 2003 at 6:16 am in reply to: low level laser therapy for pulpitis and healing of oral sur #10680
Robert Gregg DDSSpectatorHi Janet,
Before I answer your question, I want to say it was great to meet Ron Shalter and Todd Ryan spend some time getting to know both better at the ALD meeting.
Ron’s too modest to tell ya’ll, but he would have stayed longer, except he went to watch his daughter win the MVP award in the State Volleyball Championships.
One more thing….Jeff Cranska’s lecture on laser perio was fantastic! He hit the high notes and made a terrific impression on the audience. I was sitting in the back and gauging the applause. It was both spontaneous and simultaneous, which told me he impressed the audience at an individual level. He showed everyone there–even the old-timers–a new perspective about periodontal regeneration. Great job again Jeff.
OK, Janet. See if I can make this understandable.
Jeff is right about the FDA. So is Ray Tang. Although a company (I forget–Missouri I think) last January 2002 received FDA clearance for LLLT for carpal tunnel pain relief and improved range of motion. And my friend John Karna is just scratching the surface of LLLT applications. It works extremely well.
Low level laser therapy (“LLLT”–pronounced lilt) is typically used when referencing the use of “soft” lasers (non surgical lasers–aka dedicated biostimulation lasers). These are usually 635 (red) to 810-980nm (near IR) hand held lasers for treatment of pain, inflammation, swelling–of ANYTHING. Output energies on these devices are in the range of 100-250millijoules on Continuous Wave (CW).
High level laser therapy (“HLLT”–pronounced hilt) is the use of a surgical “hard” laser in a defocused (non surgical) mode for biostimulation. Defocused, the hard laser will penetrate and biomodulate, but more intensely than soft lasers. I prefer HILT since the power densities we can use are 6000 millijoules versus 250, so it takes less time, I think, to get biostimulation effects.
Tina Karu, the Russian Biostim expert, and Dr. Paul Bradley from the UK are using all sorts of wavelengths for biostim and biomodulation (e.g. pain relief).
They are using everything from red laser pointers to CO2 for biostim. So you can conceivably use your erbium 2.9 as well as your 810 diode.
So the answer for your patient is yes, you can help her.
Ron, the setting for extraction sites with diodes is .4 to 1.0 watt Gated pulse–non activated. Go to the base of the socket for reference w/o emission. Back off a few mm. Lase against the socket walls and stir as you come up. Do not let the socket dry out. If no bleeding, initiate it in the bone or crestal tissue. Repeat the sequence when socket fills with blood. Then after the socket fills with blood, put the fiber in the middle of the socket filled now with blood. Hold fiber steady and lase until a “tear drop” of blood forms on the fiber (by lifting and visualizing), or no more than 60 seconds. The blood will turn to a “rust” color, or have “rust” or darker colored bandings form streaks in the surface of the clot. Observe for cessation of blood flow, except at the soft tissue margins, which is ok. Just dab at margins with tip of a 2×2. Blood flow must stop before dismissing. Clot must be present before dismissing.
We’re just makin’ gravy!
Bob
lagunabbSpectatorRon –
Fried’s postulation outlined in bold in your message was derived from CO2 ablation at 9.6 um. Below are his Figures 7a and 7b showing the difference in composition (by FTIR reflectance) with and without water for CO2.
As shown in Figure 7a, crater surface composition is very different after dry CO2 ablation and Fig 7b shows that composition is maintained when water film was present. The heavy black line is unaltered enamel.
Figure 8 is the corresponding FTIR measurements for Er:YAG and there are relatively minor differences in between dry and wet ablation such that absorbance does not get reduced a lot after a first pulse. In the CO2 9.6um case, absorbance is drastically reduced after the first pulse and I can buy the argument that you would need to expose fresh enamel to keep ablation going. Not the case for Er. Besides 9.6 um is not well absorb in water so mechanism of water cleaning would be rinsing which would be interesting if that works.
There are two problems with his postulation, (1) how does pulverized/vaporized material deposit itself on the crater surface when there is such a big pressure gradient from the crater to the outside of the crater (2) the CO2 composition results are so different than Er (also the much lower absorbance of the CO2 wavelength in water) results that it would be hard to extrapolate CO2 postulations to Er even if they are valid.
Thanks Ron. see if this works.
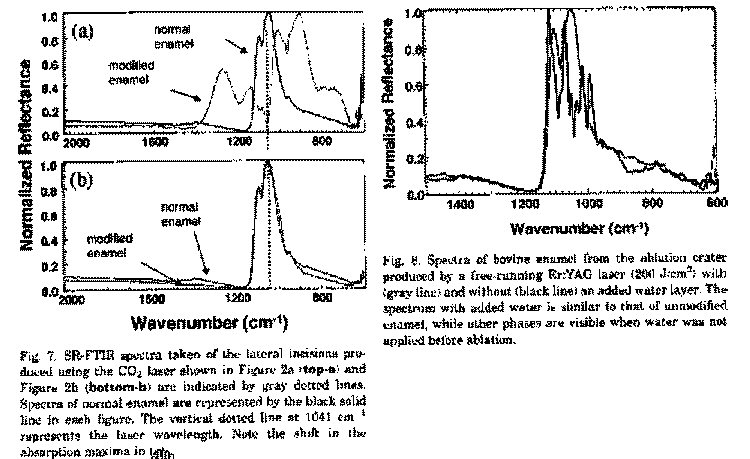
The figure on the left is 7a and 7b. The vertical dotted line is inverse of CO2 wavelength at 9.6 um. Er wavelength is off the chart to the left at about 3500 cm-1.
Figure 8 is on the right comparing dry and wet ErYAG craters. It would be interesting to see the changes if any near 3500 cm-1.
(Edited by lagunabb at 12:22 pm on Mar. 10, 2003)
(Edited by lagunabb at 12:24 pm on Mar. 10, 2003)
March 10, 2003 at 1:19 pm in reply to: low level laser therapy for pulpitis and healing of oral sur #10668
AnonymousSpectatorThanks for the info and kind words ,Bob.
I do have to make a slight correction ,my daughter was her team MVP and they were eliminated in the State regional contest Saturday.She had a very good high school career and even though I’d have liked to see more of the ALD meeting, including Jeff’s presentation,I was glad I could get home for the awards and game.How about settings using nd:YAG for the extraction sites ( since I’ll have that option available soon)?
March 11, 2003 at 12:56 am in reply to: low level laser therapy for pulpitis and healing of oral sur #10677
Robert GreggParticipantHi Ron,
QUOTEHow about settings using nd:YAG for the extraction sites ( since I’ll have that option available soon)?That’s an easy one:
3.0-3.5 watts at the fiber tip, 20 hz, 150-250 usec.
Same technique as described above. Don’t linger or drag…..
Welcome to another Periolase user, Rick Williams from West Texas.:biggrin:
Bob
March 11, 2003 at 1:22 am in reply to: low level laser therapy for pulpitis and healing of oral sur #10673
BenchwmerSpectatorBob,
Why would’t you use a wider pulse width when coagulating an extraction site?
Ron,
I always use 3.oW 20 Hz 635 usec, make sure there is blood in the socket, use bone currette if needed, then work from base up, into all sockets, and work to surface, watch clot thicken, with moist 2×2 to squeeze socket, bite on damp guaze, check in 2 minutes, let them go, have never had to retreat. Have used this technique to remove broken cusps on split teeth and extracted single rooted teeth on Coumadin patients without changing meds without any bleeding comlications.
Great healing, no dry sockets.March 11, 2003 at 1:36 am in reply to: low level laser therapy for pulpitis and healing of oral sur #10669
AnonymousSpectatorOk, review time for me (I lent Todd my books)
Pulse Width is…
time of the pulse?
636usec vs. 250 usec
_ _ _
l l_l l_l l_ length(time) peaks? ?
?and the purpose of the increased pulse width-deeper penetration?

Thanks for yopur patience,
BenchwmerSpectatorRon,
It was a great chance to pick up techniques, see new products, meet old friends and make some new ones.
A tough day back at the office today (I did get in a LPT procedure this morning)
My presentation Saturday at ALD followed 2 past presidents, the certification coordinator, and was followed by the current president. Alot of heavy hitters.
There were only 3 or 4 mentions before my presentation of don’t make claims you can’t prove without the University studies, no one has ever proved laser bone generation, etc.etc.
I presented a single case showing a PAP on #20 (non-vital) #19 8mm pockets on Distal (vital).
My contention was after Endo #20 belief is that new attachment and bone will fill in the defect at the apex. If I can achieve a similar closed system on #19 why can’t I get the same results? I can remove the diseased pocket lining, kill the bacteria, prevent bacterial re-migration, and using the PerioLase and LPT set a clot to close my pocket, then let the body heal itself.
Showed the case after LPT, 3 weeks, 3 months, 2 years. PAs before and at 2 years show no more PAP on #20, increased bone on D #18.
Then I WOWED them with the Millennium animation, finished reviewing the LPT on the diagrams. I faced the Questions. The cordinator(Rechman-U of Cal-SF) wanted to see the studies, told them they are on the way, come to the booth to see the histology. Later, when I saw him walk by the Booth,I confronted him and him and made him look at the post LPT bone histology.
All went pretty well.
I think the weather is nicer here in Maryland (at least there is Sun).
What did you think of the ALD?March 11, 2003 at 2:09 am in reply to: low level laser therapy for pulpitis and healing of oral sur #10674
BenchwmerSpectatorWider pulse, same power, but less penetration, less thermal tissue relaxation,
Allows coagulation without any charring. Want tissue 60-100 degrees C for coagulation.
Do not want vaporization or ablation.
AnonymousSpectatorSounds like an interesting day. I would have been stressed to the max getting up there like that. I’m not surprised things went well, I could tell talking to you ahead of time that you were prepared.
It would be great to see that case. I know the histology Bob showed me was amazing (I actually could see what he was talking about and didn’t feel like I was looking at an ink blot test).
I just encoded the Millenium video for Real Player and added to my website.I think it’ll be a great addition. Millenium sure has done the work in supporting and training their dentists.
I’m glad the weather is better there-I came home to 16 degrees and windchill of zero.
BenchwmerSpectatorRon,
The case is on DentalTown Cases, Another LPT Case Benchwmer 12/5/02
Todd is buying the CdROM of the whole conference, he said he would burn me a copy of my presentation.
wiemsSpectatorThanks for your reply, Jeff
I have been using the laser on 2 watts 20 Hz for troughing, and 1.5 watts 15 Hz for debridement.
I didn’t note any tooth changes, although the tip does tend to spark (light show) when it comes in contact with tooth structure.
My assistant is still alive i should note, and her mouth feels good.I haven’t really motivated to take photos of the teeth I have been working on, but I must say that I am getting the hang of it. My in office training will be in a few weeks.
I do notice that the trough around the tooth is a bit rough looking – not as clean as I would have hoped for. Could be a technique thing, but i have read of other people mentioning the same thing. The sulcus just doesn’t seem as clean as when i use cord. Hmm…I don’t have a power meter.
whitertthSpectatorOk im back!…nice stuff glenn as always….I will post a bunch this week so we can discuss….all the best to everyone!!
-
AuthorPosts
