Forum Replies Created
-
AuthorPosts
-
2thlaserSpectatorJeff,
I’d like to see those. The Spoons I developed are a bit smaller, and very sharp. Glenn can tell you more about them too. I always like to compare products. I too, LOVE spoon excavators, and hardly EVER use a bur to remove decay. After seeing what a bur does to tooth structure, I try not to use one. I have really become fairly efficient at drilless dentistry. Sometimes I am amazed. Anyhow, great post, good stuff!
Mark
Robert GreggParticipantHi Everyone,
Here’s a “Laser Periodontal Therapy” case I started last week.
This photo series demostrates the key element in treating ALL types of periodontal disease case types in only ONE treatment visit. That is, as opposed to treating a pocket or quadrant in a series of sequential visits, one week apart.
They KEY is getting a stable fibrin clot to form immediately post-op, and before the patient is dismissed.
Profound anesthesia is ALWAYS used for intial treatment.
[img]https://www.laserdentistryforum.com/attachments/upload/MarkXray.JPG[/img]
Pre-Op X-ray. Can a pocket be a VERY thick PDL space?
[img]https://www.laserdentistryforum.com/attachments/upload/Markpoach1.JPG[/img]
4.00 watts, 20 Hz, 200 mj/p, 360 micron fiber, 650 usec PD @ 110 Joules per tooth
[img]https://www.laserdentistryforum.com/attachments/upload/Markpoach2B.JPG[/img]
Obtaining a predictable, controllable, reproducible and STABLE fibrin clot has been difficult for all laser devices (especially CW diodes with or w/o “activated” hot-glass effect), until we found the value of varying the pulse duration on a pulsed Nd:YAG. Extending the thermal “injury” time for just a few hundreds of microseconds made all the difference—not too cold, too short thermal exposure time, or too photo-disruptive, AND not too hot as to vaporize, cauterize, burn the blood proteins away (they are VERY thermally sensitive;-), OR sear or DRY out the tissue edges that would prevent “clotting closure” of the wound.
[img]https://www.laserdentistryforum.com/attachments/upload/Mark7day3.JPG[/img]
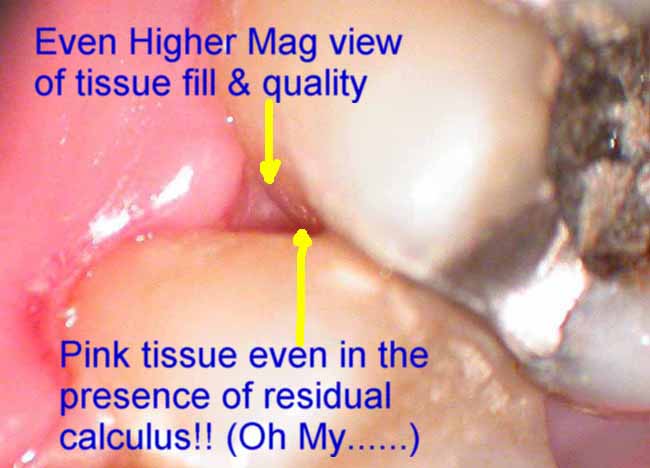
7 Day post-Op reveals fibrin clot persisting in the area still struggling to heal in the bicuspid region. The area that is healing the best, is the area which had the deepest pockets, most root surface areas involved and most negative tissue architecture. But it is important to note that the area still needing the fibrin coverage, is still showing the fibrin along with residual tissue redness and inflammation. So is that SLOW healing? Or something else???

Microscope shows higher magnification of the desirable fibrin and its appearance. No, it is NOT necrotic tissue. It also shows a better idea of how well the inner interproximal tissues are healed……sealed down below.
[img]https://www.laserdentistryforum.com/attachments/upload/Mark7dayHiResV4.JPG[/img]
Self explanatory
Self explanatory
[img]https://www.laserdentistryforum.com/attachments/upload/Mark7day5.JPG[/img]
OK…..really high magnification of the interproximal tissue appearance
Bob
Andrew SatlinSpectatorshow off!!
andy
AnonymousSpectatorQUOTEQuote: from Robert Gregg on 7:34 pm on June 5, 2003[img]https://www.laserdentistryforum.com/attachments/upload/MarkXray.JPG[/img]
Widened PDL= Occlusal Trauma?
 ?
? ?
?
Glenn van AsSpectatorHi Mark…….great talking to you today and I used your spoons today. I still like my slowspeed for decay removal verification but that is personal preference.
I still feel that with lasers it is not easy to remove the soft mushy decay but it does work well to remove the last bit of decay once the bulk has been removed with spoons, slowspeeds etc………
I will post a pedo case in a minute………
Great thread and nice talking again to you.
By the way, those of you using the lasers should really look at marks spoons…….nice stuff………
glenn
Andrew SatlinSpectatorRon,
Widened pdl, particularly at the osseous crest, changes in furcation involvement and altered lamina dura are common radiographic findings associated with excessive occlusal loading.
Andy
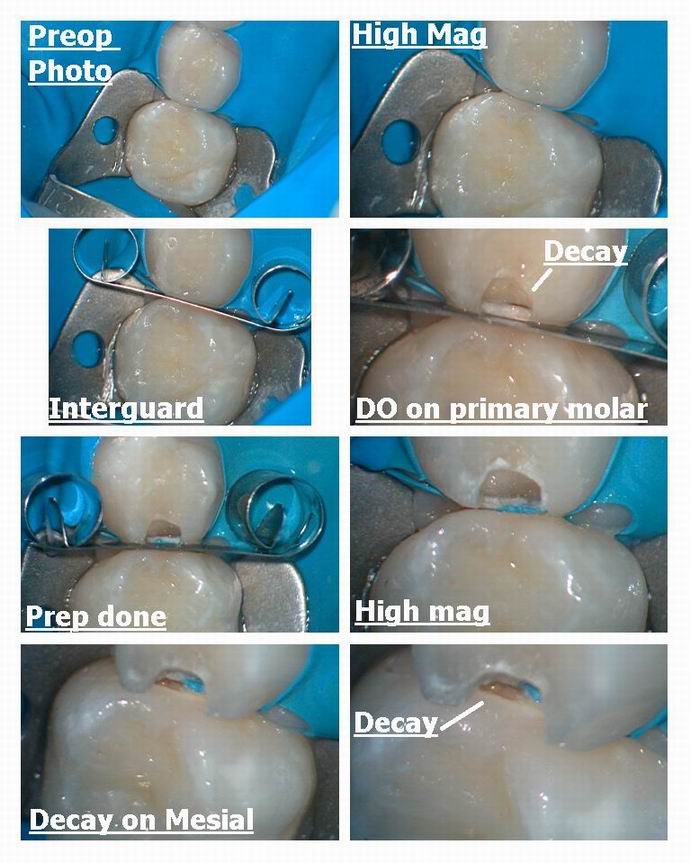
Glenn van AsSpectatorHI folks: I just wanted to show you what the combination of the laser and the microscope can do for treating children.
I did this whole case on a 5 year old today without anesthetic except for topical….took around 30 mins including photos.
Primary interproximal caries were moderate in size on the primary molars, and the Erbium Yag laser was used at 30 Hz and 160 mj with 600 micron 80 degree tip on Hoya Delight laser. That would be around 4.8 watts for the Biolase folks with a tip that has a 6 after it.(600 micron)
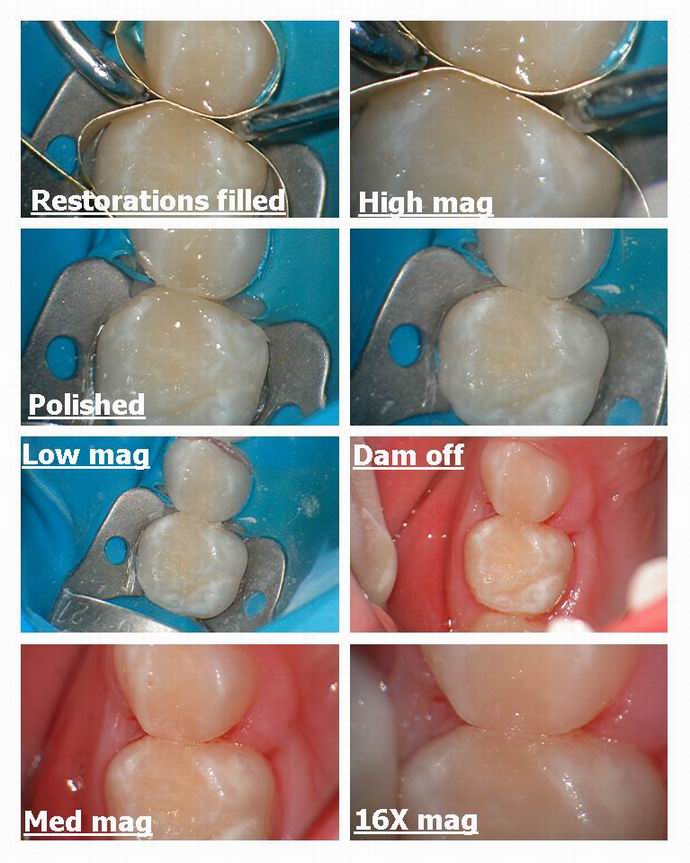
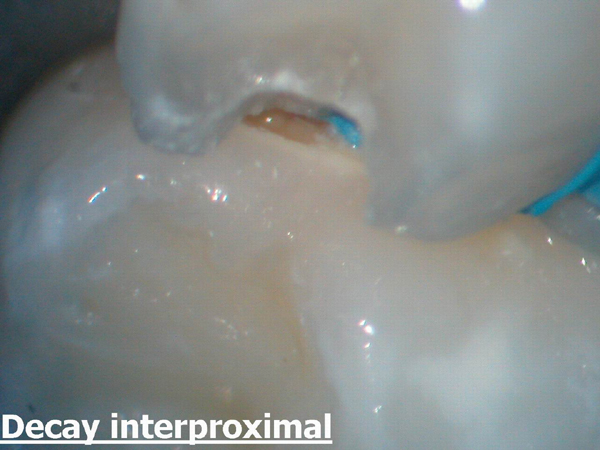
I prepped the first primary molar with an interguard in between to show you how to protect the adjacent tooth and the final photo (enlarged) shows how the decay is visible at 16X mag with the scope. You could see the hole and in addition see which side of the contact the prep needed to go.
The concern is how to check for the fact that all decay is removed as the laser is non tactile, and I either will use high magnification ( can see if the dentin is still leathery), sharp spoons (mark colonna makes a great set of these) or a slowspeed round bur near the end because there is a little bit of desensitization that occurs after using the laser for a couple of minutes that allows for etch and slowspeeds to be used judiciously.
I filled the base with a flowable (Dyract) and Tetric Ceram overtop.
The dad was watching and they are always stunned to see what is possible now ( they watch the magnified view from the microscope, on the monitor………can hardly wait for flatscreens to come down in price) and he was very appreciative of his daughter not needing anesthetic for these teeth.
I will go out and say that you can sometimes do these in kids with a bur, but it has been my experience that although the laser may be slightly slower the sensitivity with the non contact mode of operation, the water spray to cool the tooth and the gentle popping make this a nice alternative for children.
If you want to say …….I never have a problem numbing up children……..I can do that in 7 minutes…….kids are no problem for me, then that is fine, and I wont argue with you. I will say though that many of the children I have in
my practice are great when I use the laser on them……its nice having another tool in the toolbox.I am just here to show you a few pics ( like a coffee table book, just think of me as the Kramer of scopes and lasers then) so that those of you not using a laser might see what these preps look like.
Hope that you enjoy it……..all the best….
Glenn

ASISpectatorHi Jeff,
Thanks for the background.
The use of a probe is indeed a good reference for all, not just to quiet the peanut gallery.
Andrew
ASISpectatorThanks, Glenn, for sharing again.
Your images are just so darn captivating to look at. I can hardly wait to do some photo posting once my scope and camaera are set up.
Best regards,
Andrew
ASISpectatorHey, people in laser dentistry land, isn’t anyone doing desensization at all?
I am really interested in your input.
Andrew
Lee AllenSpectatorGlenn,
The followup on my patient with the bite sensitivity: I took Mark’s advice and removed all of the class I composite and found that indeed there was a crack under the distobuccal cusp adjacent to the area treated last. This was a tooth that had been restored with all bur, was 4 mm deep and off center to the distobuccal making that side thin. Prior to anesthetic, it did test postitive to the Tooth Sleuth in the same area.
This will be interesting to follow since the patient did not want to have a recommended crown (I use an intraoral camera to show patients their tooth–poor mans version of the scope), so a composite replacing the cusp was placed over a GI base. I find less contraction forces at work when I place a big base. I expect the patient to be back for the crown.
Thanks to all for the help in sorting out this one.
Lee
AnonymousSpectatorHer’s a good start-
http://www.rwebstudio.com/cgi-bin/ikonboard//topic.cgi?forum=29&topic=21
ASISpectatorThanks, Ron.
Andrew
2thlaserSpectatorLee,
You are welcome from my end. You are such a good dentist…for those who haven’t met him, trust me, he is! One other thing I do when I find those cracks, I lase into them, making sure that there is NO bacteria in them as much as possible. I also believe that this area is strengthend a bit by the restorative materials upon setting. Just a thought. Anyone else with thoughts on that? Teach me!….
Mark
Robert Gregg DDSSpectatorNice dentistry and service. No better choice for kids IMHO…
Nice pics and post as usual!
Bob
-
AuthorPosts
