Forum Replies Created
-
AuthorPosts
-
Robert GreggParticipantAh Yes!:biggrin:
The POWER of the VISUAL (magnified) illuminated image……..Seeing is believing, and understanding, and learning, and……..Glenn, are you sorry now you helped me with my photography??

Real world clinical photos (from a “real world” wet gloved clinician) are better than any sales campaign or advertisement a company not founded by and for clinicians can ever use to get their point across…without the hype. This is TRUE!
Do NOT leave it up to an photonic engineer to figure out the solution to a CLINICAL problem or challenge. You will be waiting for a LONG time. Some do it better than others, but if they had done it well enough, you guys might have never heard of me or Del. :shocked:
Wow! Some just might like that!! I can think of a few on Dental Town, the AAP, the…….
Bye for now……..;)
Glenn van AsSpectatorJeff: thanks for sharing a nice conservative technique for us to see……..
I dont like doing these kinds of preps because in my hands inevitably an unsupported cusp fractures off (MB for instance) but you have done it well. I dont believe the bonding strengthens the tooth so much.
ANother question, why Panavia F which is so opaque for such a case. I think an alterantive would be a resin cement such as Variolink or Calibra or something translucent which would have made your margins less noticeable because they do stand out.
Again in closing , thanks for sharing the case, and dont think I am being too picky ( I didnt talk about biologic width yet did I
 )
)Grin
and thanks
Glenn
Glenn van AsSpectatorBob : funny you should mention this but Gary Carr once told me that the key to acceptance was visual confirmation of the procedures at magnifications beyond what normal photography could shoot.
The pics get people to stop and think……hmmm..if he can photograph this and can see this……..hmmm….
Thats were the uncertainty starts for some that they will look at it further.
The guys who look for ROI, speed, proficiency, reducing learning curves and are resistant to change will then make up reasons why its not needed…..
This isnt rocket science
I dont want to see my work that close.
I have 20/20 vision
My lab doesnt even do work that close up
My back and neck are fine.
It wont work in my area
My staff wont like it.
I am ready to retire.
I am just starting my practice.In the end , only so many people will commit to the change and the effort required to get to the point where they can take the magnified images.
The people here on this site who have bought lasers went through a similar period when committing to that technology………
Oh well, some do , some dont, ………NEXT.
And Bob, I am never sorry that I gave you a hint or two….didnt take long for you to get such nice photos. Every time someone like you or Andrew decides that the photos I post are interesting, and you decide to follow the path I have taken, it makes me feel a tiny bit better inside, like hey maybe I do know a thing or two.
Enough philosophizing……..time for my morning decaf!!
Cya
Glenn
Glenn van AsSpectatorHere is an update on a case I did a while back (9 months or so ago) where I cut a flap to expose a premolar. Really this was my first case of attempting to do some surgery with the erbium and since then we have done extractions, osseous recontouring and other flaps stuff………
I now have put these pics into JPEGs as before they were on sendpix and are long gone in terms of storage (they were kept for 1 month on the site).
I have updated the photos to show you what the case looks like now, and intend to do this more now to show you what some of the cases look like 9-12 months down the road…….and maybe in revisiting these cases we stimulate a little bit of discussion……….
Here is my original statement and photos are attached.
Hi Folks: I am glad I went into work this morning to do this case.
I have never done an exposure before , this was my first.
I feel like Mark Colonna…….well not as good looking or as smart but something close to him then.
(A Mark Colonna wannabe)
This young 14 year girl has the most crowding of any child in my entire dental career. I extracted all the first premolars and still had trouble getting some of the teeth in.
6 months into treatment one tooth is not coming in and I take a new pan , pas and an occlusal and the upper right 2nd premolar has rotated and is not coming in as it is blocked out.
I am feeling pretty sheepish and off she goes to the specialist. Well the parents are a little upset with me for not noticing the possibility before , and ask if I can do it to save them some money………enter the erbium.
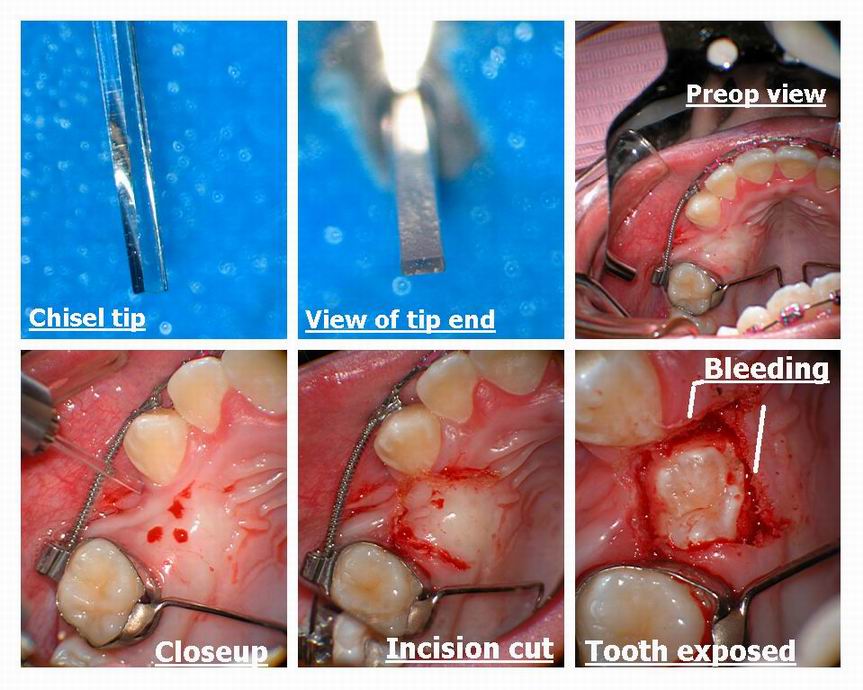
Continuum has some nice new tips which are shaped like a chisel for periodontal work ( from Japan) and in addition the make a nice scalpel. After anesthetizing……( I wasnt gonna try so dont ask me why), I very quickly used the chisel tip to cut my flap. I had sounded through the tissue to feel the tooth and when I saw no bone, I thought lets just cut a window in the palate.
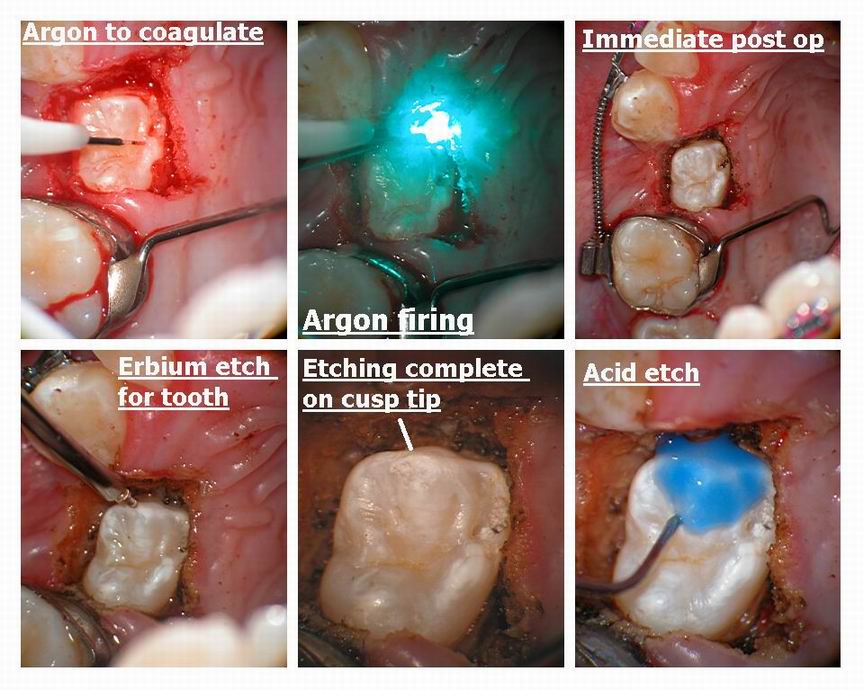
At this point , I notice the tooth was not really 100% formed, and a little decalcified. Not wanting to risk the erbium, I used the argon to quickly trough around the tooth ( I was worried about etching the tooth and bleeding).
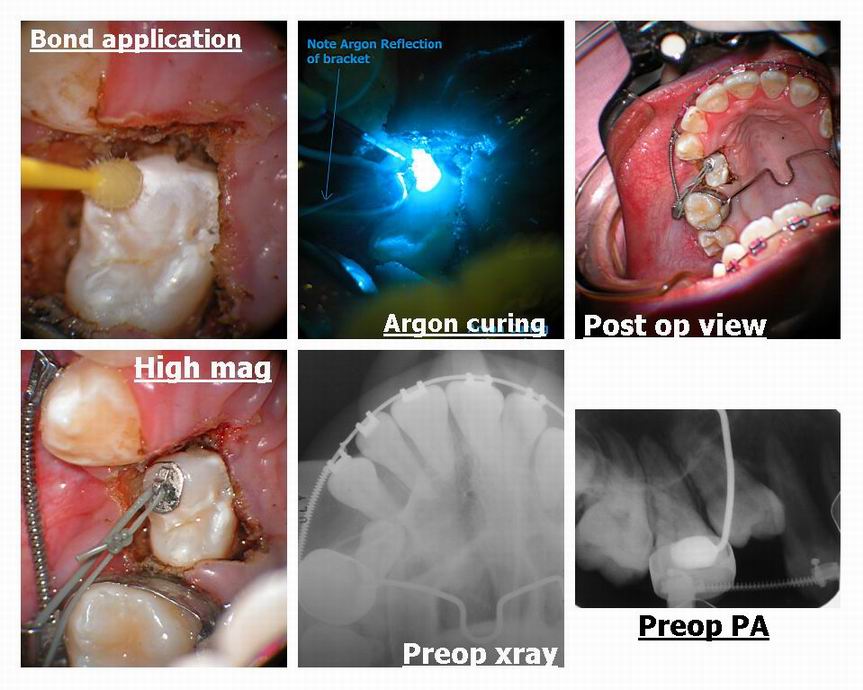
Then I thought to make a better bond of the bracket to the tooth I would very lightly etch with the erbium prior to acid etch the tooth.
Some like Mark may have been content with the erbium etch to hold the bracket on……….bigger kahunas than me.
I then tied the elastic ligature to the archwire as I didnt have a chain that could fit anywhere. I have the eyelet and I usually pigtail a ligature through to bring the tooth in.
I am trying to derotate it first and then bring it down. I have done this a few times with canines before, but never exposed the tooth myself.
I asked my O/S how he stops the bleeding……..electrosurge he says………..
Oh yes the Argon laser tip is so small it assured me that the resin was set.
I know that others who have done alot of surgery will criticize certain aspects of my procedure. I ordinarily would have done the entire procedure with the Argon , but wanted to try out the new chisel tips for flaps (worked very well at 30 Hz and 100 mj without water (3W))
Ok now time for my flame retardant suit ………..
FIRE AWAY.
that way next time I will know what adjustments to make, but remember, at least I had the kahunas to try it and the photos to show it.
Grin
Glenn

BenchwmerSpectatorGlenn,
The new Panavia Light cement is a resin cement dual cured with a dual cured dentin bonding agent. Self-etching, all in one prime and bond. Acceptable color for posterior onlays. Never any post-sensitivity. This was bonded w/o using any local. Great stuff.
Dr. Leigh wanted to do a crown on #30, (Ivy Leaguer).
I’ve been doing indirect composite onlays now for 12 years, never shoeing cusps, you have to believe in bonding. Of the thousand onlays, maybe a dozen fractured cusps over these years. Those you can repair w/ Air abrasion and more bonding. This is the third one Dr. Leigh has done for me in the last 4 years. All wonderful. No post-op discomfort at all after being lased.
Bob,
The photos are using a 20-year old, 35mm Nikon 6000, w/ Lester Dine ring light, Fugi slide film, scanned w/ HP Photo-Smart S20. These were taken using a mirror.
Thanks.
Jeff
Robert Gregg DDSSpectatorHi Jeff,
I end up in your camp about bonding these sorts of restorations.
I started bonding with DICORs in 1985, and after figuring out it was the poor occlusion that caused my problems, I now have complete confidence in my posterior inlays like this.
But I have EVERY crown, inlay whatever patient back for a one week post-op check to look at their bite on the new restoration. AMAZING what shows up ay 1 week that didn’t at the seat appt.
Bob
BenchwmerSpectatorGlenn,
WOW!!!
How can you not believe in the strength of composite bonding after seeing the forces you used in moving and alligning this tooth and the bonded bracket?
Jeff
Robert Gregg DDSSpectatorGlenn,
I’m LOL….and watching the French Open tennis.
I hear those EXACT same objections……
Decaf!? Heck, I need caffeinated Hi Test to get going every morning…….
It’s been funny about the microscope. The first year I used it 10% of the time and then only on .55 (unless I was using it to retrieve separated intruments in endo–then up to 1.5). The 2nd year I used it 20% of the time an occasionally at .66. The 3rd year I used it 40% of the time and mostly at .66. The 4th year I used it 60% of the time at .66 and 1. Now I used it 90% of the time at 1, and feel extremely comfortable to take photos….cuz it’s sooooo easy with digital cameras!
I used to bug Ralph Klink about getting 35mm for the camera, and he said to wait until digital got better. He said I would go crazy trying to get good case documentaion with 35mm. Appears he was right. This is fun!
I REALLY do understand how STRESSFUL “Change” can be in the clinical operatory (and office in general). Everytime we bring in a new technology, there is stress involved–even though it is “positive” stress–it’s STILL stress to learn something new.
I respect those who are measured and cautious in how, what, and when they bring new stuff in so that they can get the best out of the technology for their patients.
Glenn, you can feel very good about yourself and your tireless efforts to reach, challenge, and inspire so many in the profession–inlcuding the likes of me. You will never know how much you are admired and appreciated by so many who will never consider to mention it to you.
Time for my caffeine…….
Hope to see you around the 15th. Disneyland is just down the FWY from me.
Bob
Robert Gregg DDSSpectatorGlenn,
That’s sooooo reeeaaally nice a case and finish. Do you do you own ortho banding and movement? Tooth movement, I mean.;)
Bob
Glenn van AsSpectatorYes Bob….its my ortho case. I do a fair amount. Took some training for 10 years and even tried one year to get into ortho grad school (around 10 years ago) but without success. I think that someone had another plan for me (scopes and lasers) and so it wasnt ortho grad school for me (my marks were pretty average in dental school).
Yes I was a wee bit worried Jeff about whether the bracket would stay on the decalcified tooth so I bonded the bracket on erbium etched enamel.
Thanks for the kind words………maybe I should post it to dental town……..what do you think.
Glenn
BenchwmerSpectatorBob,
Using LA and acid etch I used to need frequent follow-up occlussal adjustments. Now that I can seat most of these onlays without using LA and acid-etching, I see better occlussal results and almost no sensitivity.
Jeff
Glenn van AsSpectatorHi Jeff: thanks for the update……I will maintain that I dont like the opaque color for posterior white onlays or inlays………for gold ok but that is your choice.
As for the bonding , I am glad you are getting those kind of results , I dont. My experiences with bonded indirect resins hasnt been very good. Same kind of results as with Targis Vectris which sucked in my hands.
I applaud your efforts and photography.
Thanks
Glenn
AnonymousInactiveGlenn,
NO flame retardant needed for posts like this. You did a tremendous service for your patient – that is the main concern – results. You used the instruments that you have very well.
I would have used other instruments simply because I have other instruments. But there is no way that anyone should argue that you should not have used a particular instrument – or did the work that you did with the instruments you used.
Great work and visibility.
(Edited by Delwin at 11:05 am on June 7, 2003)
AnonymousInactiveGlenn,
NO flame retardant needed for posts like this. You did a tremendous service for your patient – that is the main concern – results. You used the instruments that you have very well.
I would have used other instruments simply because I have other instruments. But there is no way that anyone should argue that you should not have used a particular instrument – or did the work that you did with the instruments you used.
One thing that I try to do when doing both sides of a contact point with composite is remove one of the “dueling” bands as soon as that side is cured to reduce the thickness of my bands and increase the potential for my ring clamp to give me the interproximal pressure that I desire in my contact point.
Great work and visibility.
ASISpectatorHi Bob & Glenn,
I echo the philosophy and conviction that you guys are speaking of and practising in.
I have indeed been very inspird, and contiunued to be inspired, by the images that Glenn have so kindly posted and shared with us all.
I attended Glenn’s microscope lecture at a Pacific Dental Conference some 3 years ago. The images that I saw stayed with me and made me question the work that I had been doing. How good is my really good work? Worse yet, how bad is my okay work? That bothered me and kept me thinking….
When my interest was intriqued by the capabilities and the enhanced healing of dental lasers, the combination of the “one two punch” just made so much sense.
I am but a neophyte in both the use of lasers and scopes, but am so excited by the end result of the treatment that I see from the generous sharing by all on this forum (Thanks again, Ron), that the learning curve that I face will just be part of the journey to enlightment.
My, if one doesn’t know any better, one would think this is Dental Philosophy 101.
Andrew
-
AuthorPosts
