Forum Replies Created
-
AuthorPosts
-
ASISpectatorVery nice work, Glenn.
You might consider to bias the bracket on the premolar more to the mesial to encourgare greater derotation distally.
How long for treatment from exposure to now?
Andrew
Andrew SatlinSpectatorGlenn,
Very impressive!!! Really nice case.
I wanted to mention that in these exposure cases you need to be aware of keratinized gingiva and design your flap accordingly.
When you are that far palatal it is not a problem, but when you are dealing with canines impacted toward the buccal it really becomes an issue. Instead of the “punch” technique you might consider reflecting a full thickness flap or sliding a pedicle.
Just thought I would point that out to people that may not have alot of experience with these.
See ya!
Andy
2thlaserSpectatorHey Ron,
Thanks for the nice feedback. I love em too. I really can’t work without them…as I don’t use the slow speed anymore to remove decay. I just hope I have increased our quality of dentistry we provide by manufacturing and making these available to all. Thanks again…
Mark
SwpmnSpectatorGlenn:
Cool case.
To make the incision, was the chisel tip placed in contact or out of contact with the palatal tissue?
You mention the incision with the Er:YAG was made “without water” – is the significance because you find that ablation is improved without irrigation?
Al
Glenn van AsSpectatorHi Del ……thanks for the kind words. When I first got my erbium it was drilled in my head that there would be alot of bleeding on soft tissue with the erbium. I had the Argon for soft tissue so why would I want to use the erbium for soft tissue??
Well when I was coerced by Tom Haney to start using the erbium for soft tissue I still remember my dental assistants look that she gave me for using the laser for a Class V….we both looked at eachother as it planed or shaved the tissue away without bleeding. Now the tissue was healthy and a small amount.
It was that moment that made me TRY to use various wavelengths for a variety of procedures to see what would or wouldnt work.
in this case I fully expected to find some bone (hence the flap window design first I wanted to try the chisel tip , which I really like…….
The bleeding was there and I needed to control it with the Argon. If I had used the Nd Yag and no bone was present (there wasnt) it would have been a cleaner cut.
I am glad that you have such an open mind and appreciate your kind words.
Andrew….yes I agree I will rebracket and overdo the rotation the other way to prevent relapse. Good point.
Andy you know what I love……your open mindedness to procedures I and others show here as we try to figure out how best to use the laser for perio procedures. You are to be admired for you positive attitude to much of what I show.
Your point about keratinized tissue on the buccal is very very valid and appreciated. I was aware of the fact that the tooth was in the palate from the occlusal film.
I am in the process of buying one set of surgical instruments to elevate the flaps……I may still use the chisel tip and the laser to cut the flap, but I intend to follow established periodontal guidelines in my flap design.
Allen……the chisel tip is used in contact with the tissue without water at 30 Hz and 80-100 mj.
Water isnt needed because the tissue has water in it.
Air to cool the tissue and in addition if you want to spray sparingly on the tissue it will remove tissue tags building up on the tip…….
Thanks for the kind words.
Glenn
BenchwmerSpectatorPatient is a seventy something, male. Inflamed and redundant tissue isolated to Mandibular anterior. Tissue condition blamed on poor hygiene, overcrowding and heart meds.

Treatment will consist of laser gingival recontouring, gingivectomy and decontamination of inflamed areas and pockets. FR, pulsed Nd:YAG w/ 340 micron contact fiber. Parameters 3.0W 20 Hz 150 usec to excise, ablate and treat inflamed gingiva.

Immediate post-op photo. Patient now has ability to clean area. Placed on three-month recall.

Redundant tissue is back on #23 at three months.

Retreated area w/ same parameters. Reviewed oral hygiene, maintain on 3-month recall.
After 3-months the tissue is back. The patient doesn’t want to change heart meds (Beta blockers) or improve his hygiene.
I guess you can’t win them all. Will keep on recall schedule.
Jeff
Glenn van AsSpectatorHi Jeff: I find that sometimes I learn more from the failures (regardless of the reason) than the successes.
Thanks for posting……be interesting to see what others suggest.
glenn
smileagainSpectatorKelly and Jetsfan
I have had my Waterlase for @ 6 months and the “hype” was that all operative could be done without anesthesia which I naturally tried… and was not satisfied with the level of discomfort the patient was feeling. Patients come to me because they want to be comfortable are not more impressed that they feel pain with a modern laser rather than a drill.
I too use LA when necessary and find that topical followed by Septocaine interlig infiltration is all that is usually necessary…Septocaine has made a huge difference.
Pain free dentistry is my goal and lasers are the way to go.
Best, Jerry
ASISpectatorHi Jeff,
Suggest to patient to consider more frequent(monthly) visits to reduce inflammation and need to retreat gingival hypertrophy. Otherwise, keep up same recare frequency and retreat as necesssary.
If he doesn’t take suggestion, his position is obvious: he doesn’t want to improve situation.
Andrew
Robert GreggParticipantHi Glenn and Jeff,
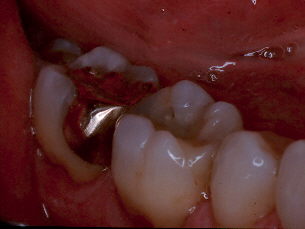
Since we are on the subject of ceramics in posterior teeth, I thought you might want to look at one on an upper left first molar “DO”. Place in 1992, this is an 11 year old “DICOR” that I photographed today on exam.
[img]https://www.laserdentistryforum.com/attachments/upload/VickiDICOR1.JPG[/img]
I can polish or abrade that margin down and/or remove the stain/decay and reseal if I want to. I didn’t.
[img]https://www.laserdentistryforum.com/attachments/upload/VickiDICOR3.JPG[/img]
Was this, is this a good service? Not very opaque, as I barely noticed the inlay under 20:20 view

Did this restoration hold up? Did it “restore” the tooth? Did it “protect” the tooth from secondary fractures? Is it easier to see stain or decay here than with a gold margin? Did it not fracture itself? I answered YES to all those questions.
Bob
PatricioSpectatorHi Gang,
Some of the table talk is getting so technical I am thinking about taking a year off to go to laser tech school. But as to the time for preping I generally am driven somewhat by time. I think 6 to 8 surfaces of composite per hour and then move the time up or down depending upon the complexity and mix of restorations and the patient. I may vary the fee as well for more complex cases adding in a surface I might over look in a quick and easy case so time and effort are factors in my fee or I just tell the assistant to use a two surface fee for a difficult one surface restoration.
I too go for the simplest and most pain free experience for the patient(considering there are different kinds of pain). Since I am driven by planned time constraints I begin in the simplest and quickest manner and escalate rapidly if needed to get the job done right with the patient comfortable in the time planned. I am trying more and more intercrestal and ligajet injections using the laser as my topical (1.5w 7/11 defocused for a few seconds)and then a small amount of anesthetic in the papilla area before I go deeper. I find in many cases very little anesthesia is necessary to continue with the laser in a sensitive area. I am about to try Cavisol for gross decay removal to see what this adds to the mix. Anyone used this product?
Pat
jetsfanSpectatorPat,
I have been using carisolv for over 6 months now, with their special spoons. By and large I have a very favorable opinion of the product, especially when used with the laser and no anesthesia. One problem with the laser is that it is sometimes difficult to differentiate normal dentin from carious. Caries detector gives false positives. The cariosolv will remove carious dentin fairly easily and leave healthy dentin alone. Often , when I think I am done I go in with this product and remove a good deal more. I look forward to trying it with Mark’s spoons.
BenchwmerSpectatorGlenn,
Panavia F Light is not the old Panavia used for Maryland bridges, it’s a new formulation, dual cured, tooth colored, about a (A3), comes w/ ED self prime and bond system.
Bob,
Still looks good. I only used Dicor for full crowns, always composite for onlays, like the way it adjusts, polishes, doesn’t wear opossing teeth.
Here is a case from 1994:

Both done at same time one gold, one Herculite Lab XRV
Now:
I’m happy with both 10 year old onlays.
Jeff
BNelsonSpectatorHi All
In response to what I think was the original question, I also plan approx 6 surfaces per hour with the Waterlase if there don’t appear to be other problems that may pop up. Today, I spent 1 1/4 hrs on a DO on 30. Same woman I did w/o LA one week prior for a 3 surface, no LA, today she wouldn’t let me get into the dentin with just the laser. Still sensitive with an interligamentous injection, and it took 2 IA with Septocaine before I could use the Waterlase to do a small! DO lesion. Don’t have a clue as to what happened. Fortunately she was the last patient of the day and wanted it done. Any ideas?
2thlaserSpectatorBruce,
How old was the patient? I find that women are more prone to sensitivity in lower molars for some reason, and that seems to be the consensus from most of the practioners I talk to. Not exactly sure why. Where was the 3 surface one you did before? Just curious.
Mark -
AuthorPosts
