Forum Replies Created
-
AuthorPosts
-
Glenn van AsSpectatorHey Allen……I learn as much from posting these cases because so many people show me stuff that I would never be able to figure out.
I actually did two crown lengthenings yesterday but only 1 with the laser, the other was a lower left third molar buccal…….YA WHAT FUN THAT WAS……..NOT
I dont mind closed flap and am starting to figure out when to use it , and really am gathering some nice case results now.
As for learning, alot of it came before the course actually because Danny, Hack2, and Andy were patient (well sometimes) with my mistakes and I am starting to get a little bit better. I have now done over 60 osseous procedures and I am feeling alot better about it.
Allen , maybe in Canada it is a little different , not so litigious. In addition the confidence the scope gives you is another factor.
I made a mistake with the Gradia as it was supposed to be posterior and not the radiolucent anterior. The flowable was either Matrix from Discus (Dont think so) or more likely the one from Caulk Dentsply that they also make in a hybrid.
Cant remember the name of hand.
Finally Al, thanks, your friendship over the years and good nature fun to keep me grounded has helped me begin to see why I do these collages.
Hope all is well in Florida and that we get a chance to share a beer, and a laugh again soon.
All the best
Glenn
SwpmnSpectatorDr. Fried:
Is it appropriate in this forum to ask about codes and fees?
Absolutely. I don’t use the erbium laser for treatment of periodontitis so have no knowledge of appropriate coding.When you use the waterlase for 15 seconds in a 6 mm pocket, is it really flap surgery and does it really reduce the pocket?
No, it is NOT flap surgery. Initial trials I ran using manufacturer recommended protocols to treat periodontitis showed no improvement in periodontal indices(these were old recommendations from 2001).Sometimes I think that my electrosurge would do the same thing.
You are probably right. In fact, with heat applied along the length of an electrosurge tip rather than just the end, could be you would see disinfection of the pocket and some initial improvement in periodontal indices.I think the erbium laser is best used for hard and soft tissue surgery like composite preparation/removal, reduction of bone in open flap procedures, troughing around broken down teeth to facilitate extractions, frenectomies and biopsies of fibromas. Also works pretty good to obtund the discomfort of apthous ulcers.
Al
Glenn van AsSpectatorGreat minds think alike Allen, I agree with EVERYTHING you said in your post…….
Heck you must have absorbed a ton of osmosis from me in that fleeting moment where you hugged me in your avatar photo!!
GRIN……
Wait , maybe I absorbed it from you………..no it couldnt be, I still never have a date when I go to dinner. You usually bring TWO!!
Glenn
PS I changed my DT avatar…..you happy now??
Grin
Robert Gregg DDSSpectatorI was just noticing that there is no “Mission Statment” on the banner or title pages of the LDF.
Anyone think this is a good idea?
Bob
Glenn van AsSpectatorI posted this on DT, but thought that it was applicable for the thread here, its my way of chasing the cracks, and I do hear what Graeme is saying but prefer at this point to go with full coverage restorations for these after minimal chasing of the crack to retain as much tooth structure as possible.
Please bear in mind that Graeme has forgotten more on minimally invasive dentistry than I will ever learn but that I havent had the problems yet with these, treating them conservatively with the laser and then putting crowns on after to hold the cusps together.
This one was asymptomatic.
Glenn
HI folks: I think that there is alot to be learned and discussed from this case I did last week so here goes…….
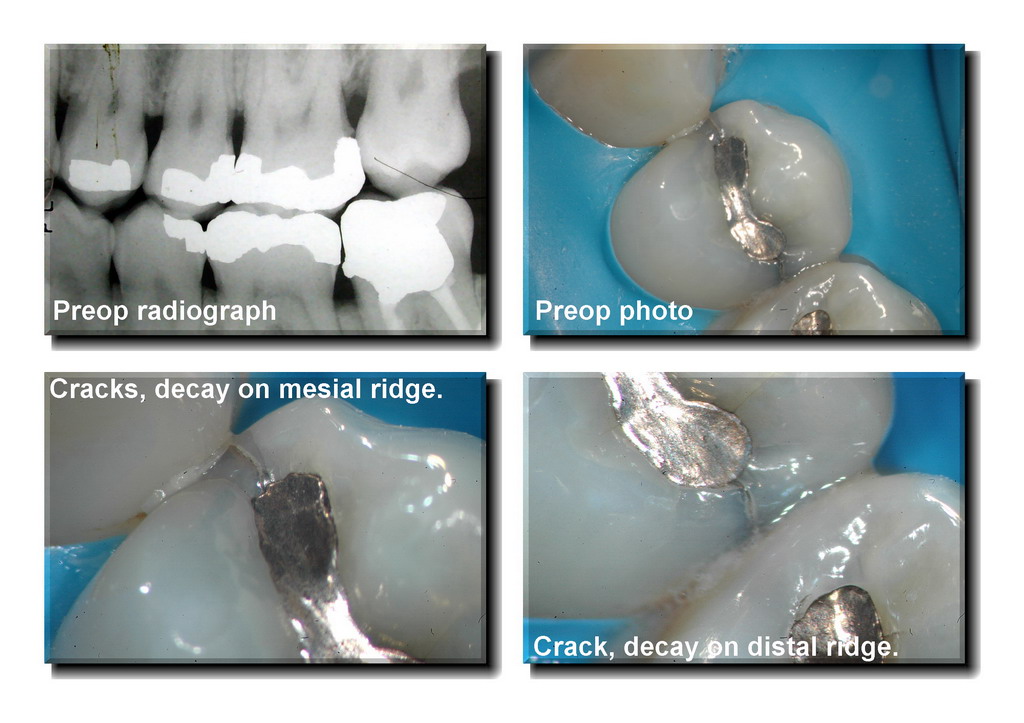
This patient came in a little while ago and although I couldnt see anything on the BW radiograph, I didnt like the look of the occlusal amalgam on the first premolar (maxilla- left side, number 24 in Canada , #12 in US).
What didnt I like, well the shadows on the marginal ridges but more importantly the cracks on the mesial (2 of them) and the one crack on the distal. Now I can tell you that almost always when I see this there is trouble under the amalgam and the restoration better be removed because these are the precursors to vertically fractured teeth (Mesial to Distal cracks).
I hate shadows on marginal ridges and when there are cracks visible at high mag they are a deadly combination.
THe patient said to me……” I dont want to do anything, it doesnt bother me to cold or chewing”
I told him that if there was nothing underneath the old amalgam that I would do it for free (hes a good friend) and bet him that there would be ( bet was a cold one next time we get together).
He agreed to see what was under there.
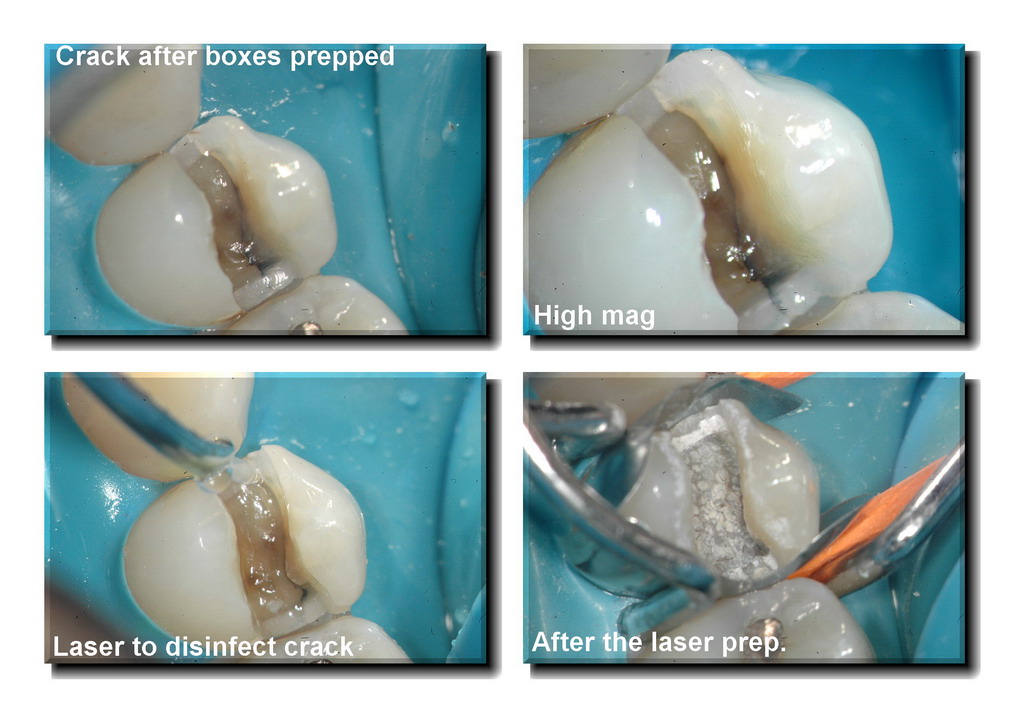
WOW …….what a crack huh, and it was asymptomatic. Now Rockin Rod Kurthy has a great picture of a vertically fractured tooth that he shows to his patients who have cracked teeth showing what end stage vertical fractures (requiring exo) look like. Its amazing how with high mag and illumination I see these all the time and now we are starting to treat them pre-emptively before they cause symptoms.
I hate chasing the cracks despite very knowledgeable people like Graeme Milicich who say that you must remove the whole crack, I prefer to remove a little with the erbium laser (400 micron tip cutting 1-2mm into the stained groove to remove the stain) and then fill the area with flowable and do a core buildup, afterwards removing the occlusal forces.
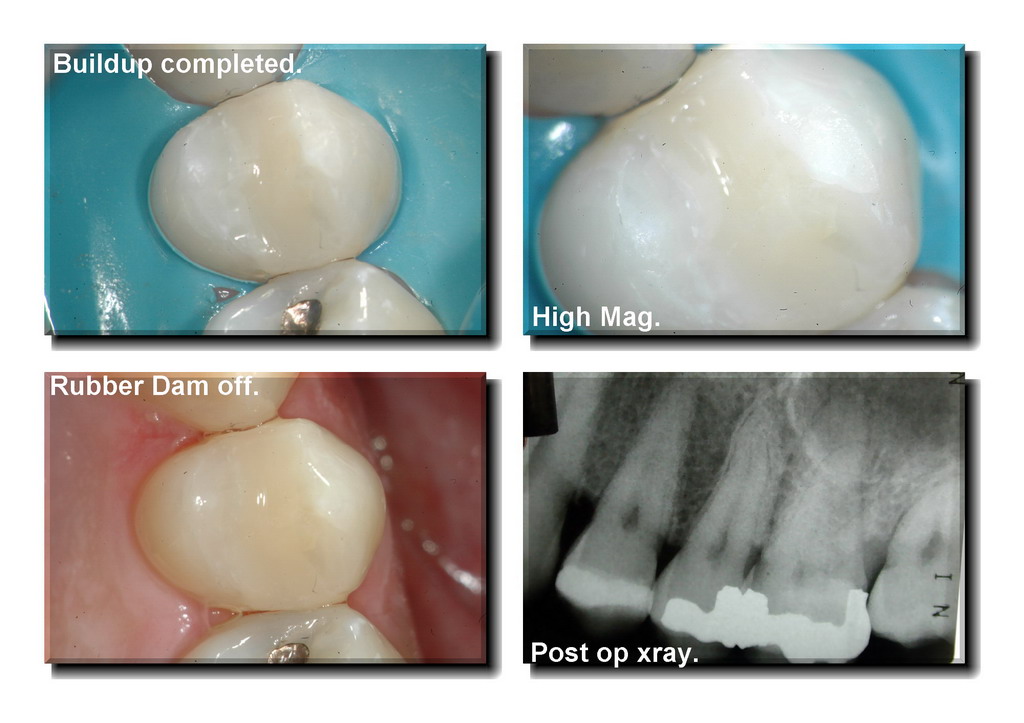
Now remember, this tooth was asymptomatic to begin with so there are no pulpal symptoms, the tooth test vital and as you can see from the post op rad, the restoration is a LONG ways away from the pulp.
He is scheduled for the crown to try and hold it together.
I hope it stimulates some conversation but my main points were.
1. Cracks on marginal ridges Mesial and Distal with gray shadows are not a good thing.
2. With high mag and illumination you can attack these cracks prior to them becoming symptomatic and in my opinion save the patient from endo or catastrophic vertical fractures.
3. The laser if you have one can help reduce bacterial count (one of the reasons for sensitivity) without removing alot of tooth structure.
4. Crowns on these are ideal and the scopes documentation helps get this approved.Finally I know he needs other work in his mouth……..we are getting there slowly but surely.
Cya
Glenn


kellyjblodgettdmdSpectatorRobert – this is a great question. I’ll give you a little “head’s up” from what I’ve just experienced. I decided a couple months ago to advertise our office as the exclusive “Laser Periodontal Therapy” office in town. It took less than 6 weeks for some unknown dentist to complain to the Board. The only changes the Board required of me was to state that I am not a Periodontist. (?)
My point is be overly cautious if you want to minimize issues with the Board. Granted, the Board doesn’t really have an issue with my advertising, they just have to deal with the complaints that are filed to them.
I’m sure there are a lot of guys on this forum that have tried one avenue of advertising or another. Hopefully, we’ll get some good responses going on this.
Kelly
spider24SpectatorComparative Study on CW-Mode versus Pulsed Mode in
GaAlAs-Diode-LasersDr. med. Dr. med. dent. Claus Neckel*, D-Bad Neustadt / Germany
ABSTRACT
In the last six years, GaAlAS-diode-lasers have become more and more popular. Due to their small size, their good electro-optical coupling and delicate glass fibers, this type of laser fits into most dental offices perfectly. The first diode-lasers and still most of the devices on the market, work in a continuous wave mode or in a gated mode up to 50 Hz. When using this setting, high temperatures in the tissue are inevitable.
In this randomized study we tried to evaluate the difference in clinical cutting efficiency, post operative outcome and the histological findings of the excisional biopsies using a new diode-laser called ora-laser jet 20.
We preformed 40 biopsies:
Group I: in cw-mode
Group II: in pulsed mode 10.000 Hz gated (1:1)
Group III: in pulsed mode 10.000 Hz gated (1:3)
Group IV: in pulsed mode 10.000 Hz gated (1:10)
The macroscopic results and postoperative outcome of the patients in group IV were best.
Scarring and postoperative pain was more intense in the cw-group and high-pulsed group with an on/off-relation of 1:1. the histological evaluation showed more thermal damage the longer the laser pulse lasted.Keywords: laser, diode, cw-mode, pulsed mode, gated on/off-relation
1. INTRODUCTION:
A surgical diode-laser in dentistry was first introduced in 1994 by ORALIA, Germany1. Since that time, many companies have seen its potential and brought many new products on the market due to the main advantages of this lasertype as: small size, good electro-optical coupling and the use of delicate glass tips or fibers. On the other hand, there are still some technical pitfalls that have to be overcome.
Diode-lasers deliver their energy in a continuous wave mode or a gated pulsed mode. Thermal interaction with the lasered tissue is largely dependent on the wave length, the target tissue, the output power at the fiber tip and the application time.
Heat dissipation or diffusion from the site is a function of the thermal conductivity of the tissue and laser time. Collateral damage in the surrounding structures can ultimately be observed after laser application. Minimal thermal side effects are the aim of laser application to differentiate from sheer thermal cutting using electro-surgery.Due to the technical problems, diode-lasers run either on a continuous wave mode or gated2, mostly in an 1:1 on/off-fashion. Using this kind of application parameters, we experience a high thermal interaction and a continuous temperature rise in the target tissue. Low output powers are necessary to keep charring and thermal damage minimal. Cutting efficiency is reduced and intraoperative anesthesia is mandatory.
In 1999, a high-pulsed diode-laser (ora-laser voxx 08) was introduced which could achieve a gated pulse frequency of up to 10.000 Hz. With a laser diode rendering 8 Watt output power at the fiber tip, the cutting efficiency3 could be accelerated, nevertheless not without giving users problems in finding the right parameters for a sufficient application of the laser.
Aim of this study was to use fixed parameters of a new diode-laser for excisional biopsies of the oral mucose and to evaluate the clinical, individual and histological outcome of the patients and the specimens.
2. MATERIAL AND METHOD
In the study, we included 28 female and 12 male patients in an age range between 34 an 71 years. All 40 patients were randomly selected. The excisional biopsies were preformed under local anesthesia, using 3 % Aricain with 1:200.000 Adrenaline (Ultracain&Mac226; DS). Aim of the therapy was to obtain a histological diagnosis and to remove the entire tumor.
2.1. Clinical diagnosis of the biopsies:
26 fibromas
14 epulides fissurataThe dimensions of the tumors were in a range of 5 cm to 8 mm and were primarily situated in the cheek or the vestibule.
After excision, no sutures were used and no wound dressing was applied. If necessary, the denture of the patients with epulides fissurata was relined.2.2. Our laser:
The laser we used in the study was the ora-laser jet 20 of the company ORALIA GmbH, Konstanz/Germany. It is a GaAlAs-diode-laser emitting 810 nm. Maximum output power was 25 Watt. Continuous wave mode and pulsation of up to 10.000 Hz gating with an on/off-ratio between 1:1 and 1:10.
2.3. Clinical parameters in the study:
Group I:
400 µm glass fiber, continuous wave mode, 1.5 Watt output power at the fiber tip.Group II:
400 µm glass fiber, pulsed mode 10.000 Hz, gated 1:1 on/off-relation; a peak output power of 5 Watt at the fiber tip.Group III:
400 µm glass fiber, pulsed mode 10.000 Hz, gated 1:3 on/off-relation; a peak output power of 20 Watt at the fiber tip.Group IV:
400 µm glass fiber, pulsed mode 10.000 Hz, gated 1:10 on/off-relation; a peak output power of 25 Watt at the fiber tip.Cutting efficiency and intraoperative appearance was monitored. All patients were followed-up after 3 days, 1 week and 4 weeks. We evaluated all patients for their individual postoperative pain, clinical aspects of wound healing and the histology of the specimens with respect to thermal damage to the tissue.
3. RESULTS
3.1. Operative findings:
Cutting efficiency:
The comparison of cutting speed showed that the continuous wave mode with 1.5 Watt output power at the tip had the lowest praparation rate.
It was followed by the biopsies of group IV with the on/off-ratio of 1:10. The difference between both groups was significant, whereas the speeding up between group IV and III (1:3 on/off-ralation) was only subjective. The significantly fastest group were the biopsies of group II.Clinical aspect of the donor site:
The parameters we looked at doing the excisional biopsies were charring and blanching of the tissue. Group I (cw-mode) showede some charring of the epithelial lining. The tissue had a very dry aspect and about 0.5 mm blanching around the excision. Group II looked very similar to group I. Charring was also significantly present. Both group III and IV presented different features. Charring was significantly less visible and the surface of the wound had a raw less dry aspect.Coagulation:
All groups showed sufficient coagulation in excision region. No bleeding occurred during the procedure or the wound healing phase even in patients with bleeding disorders (N: 6; 5 Acetylsalicylic Acid, 1 Coumarintherapy). The wound surface was totally dry in group I and II and showed a raw aspect with bleeding spots in group III and IV. These bleeding spots did not require any treatment and showed no bleeding tendency even after vigorous rinsing.3.2. Postoperative findings:
Individual patient outcome:
All patients reported of no or minimal postoperative discomfort. In those cases where the excisions were in direct contact to the margin of the dentures, the patients observed discomfort during masticatory function. No significant difference between the groups could be evaluated.Clinical postoperative follow-up:
At the three day postoperative inspection in group I, we found a slight redness of the direct surroundings of the excision. The wound had a grayish-white layer of fibrin on the surface. Wound sensitivity was minimal. One week postoperative, we found closing of the wound from the margins. Even small wounds of 8 mm in diameter had not yet filled in. Redness was not present. After four weeks, all wounds had closed in. In most cases, it was very difficult to distinguish the excision site. Scarring was minimal.Group II showed significant redness of the surrounding tissue after three days. Wound sensitivity was minimal even with the showing redness. The fibrin layer on the surface of the wound showed typical structure. At one week, in three cases redness of the surrounding tissue still without sensitivity was present. No wounds had yet closed in. The wound healing seemed to be delayed in comparison to group I. After four weeks, all wounds had healed. The identification of the excision site was easier as little scarring was detectable. The scarring was a visible mark without functional changes as induration or tissue augmentation.
Group III displayed minimal redness around the excision after three days. Fibrin layer and wound sensitivity were normal. After one week, the wounds were closing in. No wound, even small ones, had totally reepithelialized. After four weeks, all wounds had healed. Almost no scarring was distinguishable.
Group IV presented only in two cases redness in the periphery of the wound after three days. Sensitivity was minimal. All wounds had a fibrin layer. At the one-week follow-up, we found good wound healing with a significantly faster epithelisation rate. A small wound had almost closed in. After four weeks, the excision sites could not be distinguished. Scarring was not visible.
3.3. Histological findings:
The histological evaluation of the biopsies confirmed in most cases our clinical diagnosis. Only in one case, the diagnosis fibroma hat to be specified as ossifying fibroma. In the specimen you could find osteoclastes and osteoblasts with mineralized and non-mineralized osseoid. The tumor had no hint for malignancy and was removed totally.
In group I with continuous wave mode, the histology showed a thermal damage zone of up to 125 µm. The range found lay between 80 and 125 µm. The target tissue for thermal damage is connective fibrous tissue. Very little muscle cells are effected.
Dehydration of all damaged cells is prominent. Signs of coagulation and protein denaturation are predominant. Some superficial charring adjacent to deeper thermally deteriorated zone could be found.Group II exhibited similar results only that the thermal effects were significantly more drastical. The thermal alteration showed a depth of 250 to 800 µm. Muscle cells and fibrous tissue showed dehydration and cellular disintegration, Charring was an often found site with very deep thermal damage.
In group III the histological changes exhibited a thermally damaged zone of 45 to 65 µm. Connective tissue again was the main target. Dehydration of the damaged cells was prominent. Charring was found very seldom and the thermal destruction zone was more constant in depth.
Group IV displayed a maximum of thermal damage of 25 µm. The depth ranged between 15 and 25 µm. Charring was not visible. The thermal damage zone was very consistent in depth.
All specimen could be evaluated by the pathologist. Total marginal evaluation was only possible in the specimen of groups III and IV and of group I in 50 % of all cases.
4. DISCUSSION
Photothermal interaction with tissue is the basis of surgical lasers. In this process, radiant light is absorbed by the tissue and becomes transformed to heat energy changing tissue structures4. The amount of laser light that is absorbed is dependent on a number of factors such as: wave length of the laser radiation, power output at the laser tip or focus, pulse or non-pulse , if applicable: pulse character and the optical properties and composition of the target tissue5. Every single parameter of the laser beam can significantly alter the thermal interaction of the laser radiation in the tissue. The wave length by large determines the heat generation in tissue as the absorption of the radiation in a specific tissue is dependent on the emitted photon character. The CO2-laser-beam is highly absorbed by intracellular water with soft tissue. Because of this, 90 % of its energy is absorbed within the first 100 µm of penetration of the tissue surface3. The high absorption of the laser energy leads to rapid vaporization of water and pyrolysis of organic material in the target tissue. High superficial carbonization and charring can be observed even when using low energy densities. Diode-lasers emitting 810 nm are well absorbed in dark pigment as hemoglobin, melanin pigment and other dark tissue components. The absorption rate in water is by far lower than in a CO2-laser6,7.
Laser light is primarily absorbed by the tissue inducing a molecular excitation8. Important is that the target molecules have a similar energy level structure as the laser wave length. Later the thermal energy is dissipated to the surrounding tissue structures by thermal diffusion and conduction. Heat dissipation is dependent on the thermal conductivity of the target tissue and will determine the extent of collateral damage in the adjacent tissue. This process which is highly influenced by the vascularity of the tissue, is characterized by the thermal relaxation time of a specific tissue. The degree of collateral damage is dependent on the target tissue properties such as tissue composition, water content, vascularity, volume of radiated tissue and tissue surface9. Furthermore, radiated energy and length of radiation are important factors in this process. Thermal relaxation time is the time that is required for a specific tissue to cool down from an accumulated temperature to 37 % of the maximum value10.
Using a continuous wave mode for surgery thermal dissipation is minimal other than by blood flow. Constant motion of the fiber tip is therefore mandatory to avoid overheating of the tissue11. Although lower power output is recommended, tissue dehydration and charring is observed. Using a pulsed approach, in a gated 1:1 on/off-mode, tissue has time to dissipate heat and to keep the temperature from rising continuously. In our clinical setting using a 10.000 Hz pulsation, we encountered more clinical, individual and histological damage than the cw-mode group showed. This is due to the fact that the time of the off-phase was too short for a sufficient heat conduction, leading to a continuous increase of temperature. This also explains the clinical signs of mild inflammation in the postoperative phase and the scarring of the healed tissue. By lengthening the off-phase, heat dissipation is much more sufficient and thermal damage can be controlled much better. This can only be achieved at the expense of cutting speed. Therefore the pulsed mode with an on/off-relation of 1:1 had the best cutting momentum, an on/off-ratio of 1:3 was similar and the on/off-ratio of 1:10 showed a slightly slower speed. High output power at the fiber tip helps cutting efficiency and with clinical parameters of 20 or 25 Watt the cutting is comparable to a CO2-laser.
Important when comparing diode lasers is the fact that we defined the output power as power at the fiber tip and not as output power of the laser diode. Due to the ovoid outlet, the optical coupling is very difficult and often we find a significant loss of energy between laser diode and fiber tip12.
In the histological specimen, we found equivalent results to the clinical findings. Using a very high pulsation rate and short relaxation time, a thermal effect in the tissue is prominent. Charring can be found readily. This carbonized tissue is an example of laser induced modification of taget tissue. By burning the superficial tissue, a new extremely high absorbing agent is created that can create excessive high temperatures of up to 3200° C. This temperature is thereafter dissipated and conducted into the surrounding tissue damaging its structures irreversibly. All specimen showing charring simultaneously exhibited a deeper concentric thermal damage zone. By using a very high power output and longer off-period in the gated pulsed mode, thermal interactions in the tissue could be controlled. Charring was minimal and therefore unintended side effects of excessive heating as could be found in the gated one-to-one on/off-relation.
By controlling the thermal side effects of laser application, we found that this treatment stand out again electro-surgery. In this therapy, thermal destruction is by far more prominent. A further advantage of both treatments is their coagulating ability. Even in group IV with minimal thermal destruction of the target tissue, the coagulation was absolutely sufficient to achieve a stable wound over the period of healing. This therapy can also be used for patients with bleeding disorders3.
5. CONCLUSION
After introduction of high-pulsed diode-lasers, it has become very difficult to distinguish the right clinical parameters for the surgical use of these machines. For excisional biopsies with the ora-laser jet 20, we recommend using a continuous wave mode with low output power and low cutting efficiency or to excise with high output power, high pulsation rate and at least an on/off-ratio of 1:3, better 1:10. Clinically and histologically, 25 Watt peak output power at the tip, 10.000 Hz and an on/off-ratio of 1:10 gave the best results. The difference in cutting momentum was not significant. 10.000 Hz combined with an on/off-ratio of 1:1 brought the largest thermal destruction zone and should not be used. All clinical parameters apply to the ora-laser jet 20 and do differ from other diode-lasers on the market. They should be adapted adequately.
SwpmnSpectatorQUOTEAnyone think this is a good idea?Generally good idea. We have to defer to the founder for his opinion.
Have many complex thoughts regarding the subject based on what I’ve observed over the last four years.
This forum is unparallelled. Only “pure” forum where dentists can discuss/debate their findings and inherent biases. No $$$ input here from the manufacturers.
lookin4tSpectatorI like what you’re doing..and I’m not sure I want to see my cases mag’d that high.
One comment-DB of the molar-I’m sure you smoothed it in a later photo, but notice what the end cut of the chisel tip creates in that area that you smoothed out later. A little divot-may be easier to smooth is out with something that is not solely end cutting…..you’re doing very nice work however. As I said, I’m not sure I want to mag my work that high

kellyjblodgettdmdSpectatorBob – how succinct :biggrin:
(You know I’m dying to hear more)
Kelly
kellyjblodgettdmdSpectatorTreated a patient last week with moderate to severe tenderness in her buccal vestibule fro #22-28. She couldn’t brush or floss, her tissue was so tender.
Pre-lasing condition:

The area was treated w/ 2000J of Nd:YAG energy in a defocused fashion (20Hz; 100usec pulses; 200mJ/pulse).
43 hours later the patient presented back for evaluation. She said she hadn’t felt any pain since the lasing. She was truly amazed and thankful.Post-Op condition:

Cool stuff!
Kelly
kellyjblodgettdmdSpectatorBy the way – I posted the much smaller lesion I treated for this woman on this forum 2 years ago. Fortunately, she knew who to see when this tissue stuff reared it’s ugly head again:
http://www.rwebstudio.com/cgi-bin/ikonboard//topic.cgi?forum=24&topic=49
Kelly
AnonymousSpectatorGo to it guys 😉
My purpose for this forum was one- the sharing of information to overcome the woeful lack of training , generally available, at the time the forum was started.
Glenn van AsSpectatorThanks Lookin4t, I think your cases would look far better especially in the suturing department. I agree that you have to think alot with end cutting only devices.
Its alot of work not having side cutting and some divots do get created.
Hope all is well in sunshine land……off to Charlotte to Nash tomorrow.
Cya
Glenn
Glenn van AsSpectatorThat is way cool and only 43 hours later……unreal.
I have an assistant with lichen planus erosive form and she is suffering.
Wonder if it would help for her.
Great case Kelly, wonderful photos too……
CLAP CLAP CLAP
Glenn
-
AuthorPosts
