Forum Replies Created
-
AuthorPosts
-
Don ColuzziSpectatorHi Ken: Karl Stock’s paper at SPIE was in presented in January 1997, before Er,Cr:YSGG made an appearance in the marketplace.
His conclusions of the superiority of Er:YAG on wet tissue of course make sense, because of the difference in water absorption.
As I said previously, you should concentrate more on “current” papers. The present thinking on dental hard tissue absorption is that the water component of course has a peak near 2.94, then there’s a smaller OH- “shoulder” at around 2.79, and a higher (than water) peak for phosphate (Calcium phosphate is the basic apatite) around 10 microns plus or minus. (9.6 TEA CO2 is the best for ablating apatite.)
So, for our current technology, “wet” hard tissue has the greatest cutting potential with Er:YAG, but Er,Cr:YSGG is quite good. Most studies with THOSE two wavelengths have shown a higher ablation temperature with Er, Cr:YSGG than with Er:YAG, but those same studies indicate no apparent adverse pulpal effects.
Again, don’t get hung up on the missing “Cr” in the papers; clinically we use Er, Cr:YSGG and Er:YAG; the investigators use other things…….DON
Anyway,
spider24SpectatorHere is the paper from Keller et al. i noticed before. Ken was so kind to email it to me.
http://www.elexxion.com/images/Comparison.pdf
One thing is very important: The comparison was done at one fixed setting for both lasers (300 mJ/400 µs/4Hz). With other settings it might be completly different.
Olaf
whitertthSpectatorbump
AnonymousSpectatorRon, I think a great deal of the success or failure is due to the patients anticipation and perception. The success rate definitely can definitely be driven higher when the patient is preconditioned with the words -‘ we can always give you a shot, if we need to’ or ‘this is going to feel cold like eating ice cream’. I cringe when I hear the ‘shot’ technique being used, who wants a shot?
Now that being said, I do think that a patient often feels a difference in the procedure, especiallly when moving from a high energy analgesia technique to a prepping energy that is much lower. Again, this may be a way of preconditioning a patient by having them experience a certain level of percussion and energy, followed by a lesser level of percussion and energy, which in comparrison to the high levels, doesn’t seem too bad. Can’t say I ever had any success using the low energy/ slow analgesia technique.I also agree with your statement about visualization. Since the scope I have pretty much abandoned either the high energy or the slow analgesia techniques and see no difference in my success rate. If you can visualize where the tissue and energy interact, you can control the amount of thermal change and keep many people comfortable during the procedure.
As far as why some people react differently than others I wonder if the NTI guys aren’t on to something regarding the clenchers/ change of local pH ideas. Maybe the same thing is happening with the areas that respond somewhat hyperactively to the laser. Change in local pH affecting the speed of chemical Rx in the pain response.
Just my totally subjective , unscientific, anecdotal, two cents 😉
p.s. Bruce, if we’re going to standardize patients I’ve got a list of other attributes we should have them work on

whitertthSpectatorgood points…lets keep this going….
DrDanSpectatorI can’t explain “why” it works when it does…but I do know that more than half the time it does work. I also know that just because it fails on one tooth…it does not mean it won’t work on a different tooth in the same mouth. I’ve seen it happen many times. Why would it work with #19, but fail on #20? They’re side by side. A LOT of it has to do with how we remove the amalgams. The pulpal floor is the most sensitive…so I leave it till the very end. I especially want to remove all the amalgam around the edges early on. After I’ve got nothing but a VERY thin layer of amalgam left across the pulpal floor I’ll penetrate it (barely) to gauge their response. If they don’t flinch I’ll continue on. If they do flinch…I’ll try to flake it out with an explorer. You’d be surprised how many cases you thought were gonna fail that you can succeed with by doing this. You can usually flake out very thin amalgam with not much trouble.
All in all I’d say we get it done in a fairly comfortable fashion 75% of the time.
Dan
DrDanSpectatorDo you see the golden “cats eye” like we used to see on the Waterlase?
I assume you look for a black spot in the middle of the mirror…..correct?
Dan
dkimmelSpectator
So pull the Hp off about an inch.

Pretty easy to see if the mirror is clean, dirty or burnt
Tough pcture to tak.
Hope that helps Dan. It is easier to see this way then even with the Waterlase.
Glenn van AsSpectatorNot so tough to take with a scope!!
I got your PM the other day, will respond this weekend David….keep smiling and your chin up!!
Cya
Glenn
AnonymousSpectatorHi all,
Thought I’d post a followup on a perio case using the Periolase.Total Energy =5626 J Ablation done in ‘diode setting’
Tx date 01/05
Pre TX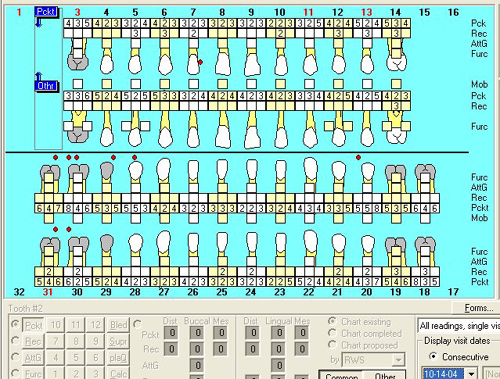
[img]https://www.laserdentistryforum.com/attachments/upload/ww101404.JPG[/img]
Charting 7 mth
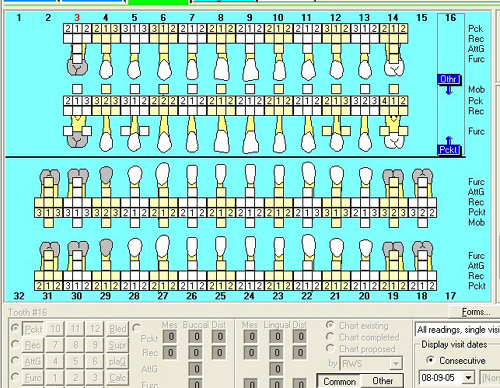
Xray image today
[img]https://www.laserdentistryforum.com/attachments/upload/ww111605.JPG[/img]
Pt is using Oral B 3D. Refuses to wear HBG due to PAP machine for sleep apnea.
Crowns are not mine
Charting same today as in August.
Just thought I’d put this up as there are alot of new Periolase users out there that can’t wait to see their results.
Glenn van AsSpectatorI love it RON……this is exactly what I am looking for to see what results people are getting. Post this on
DT as it is exciting in my mind.Some will say it is the removal of the calculus that did it but how did you get bone in the furca.
Pockets down from 7-2……..
Tell me what peridodontal charting program this is. It really is nice what you have done.
Glenn
CLAP CLAP CLAP…….please keep them coming.
AnonymousSpectatorAnother patient. Had a no show so I’ll just get part posted. Charting is PracticeWorks.
PreTx
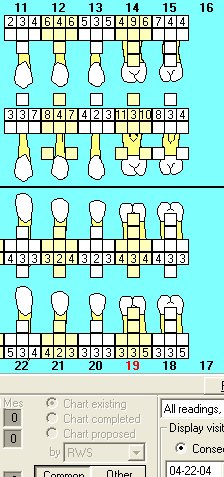
[img]https://www.laserdentistryforum.com/attachments/upload/rc2.JPG[/img]
10 months later. BTW, patient never showed for any recalls between lanap and this appointment where he came in because of breaking a splint.
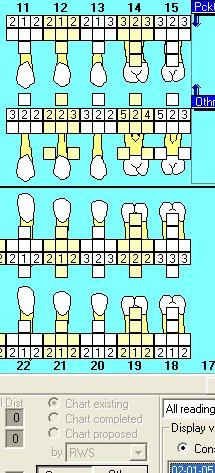
[img]https://www.laserdentistryforum.com/attachments/upload/rc1.JPG[/img]
Gotta go. Thanks for the kind words, Glenn.
Robert Gregg DDSSpectatorWow Ron,
That’s awesome! The staff here was giving you “hoots and hollers”.
Thanks for posting!
Bob
JonaarSpectatorOur Waterlase is several years old but has been used very little. We are now trying to use it on a more regular basis but find that its cutting efficiency is very poor. Does the machine need to be serviced or do we need more operating experience? How often do users have the equipment serviced? Do users have it calibrated each year, as Biolase recommends? Do users buy the costly service contract? Is it a good idea to have a service contract? What is your experience with maintenance?
JonaarSpectatorOur Waterlase is several years old but has been used very little. We are now trying to use it on a more regular basis but find that its cutting efficiency is very poor. Does the machine need to be serviced or do we need more operating experience? How often do users have the equipment serviced? Do users have it calibrated each year, as Biolase recommends? Do users buy the costly service contract? Is it a good idea to have a service contract? What is your experience with maintenance?
-
AuthorPosts
