Forum Replies Created
-
AuthorPosts
-
Glenn van AsSpectatorHi Doug……..its been too long for me since I have posted here. I saw Rons sig and felt guilty…..darn it all.
Its 2 am and I am in Vegas starting a lecture tomorrow and I cant sleep.
Here is that case I did the other day.
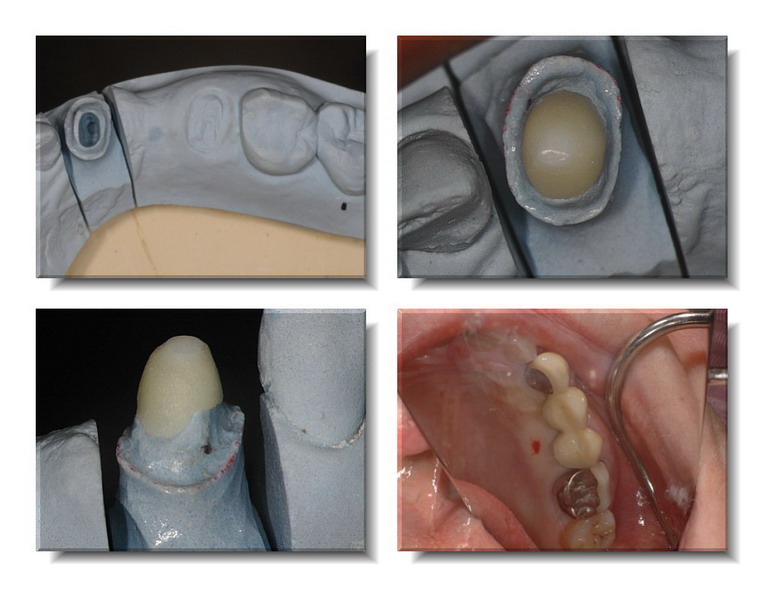
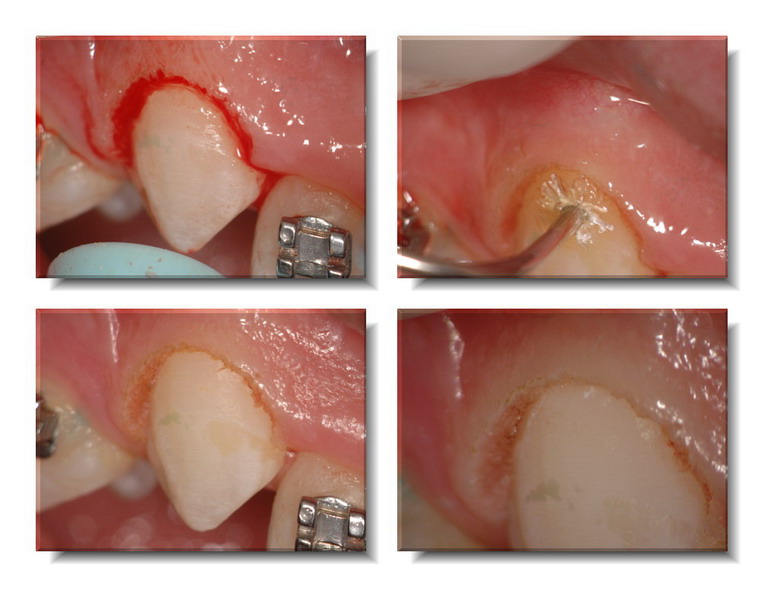
The original bridge from the premolar (2nd ) to the canine fractured and the patient doesnt want implants. I tried to salvage the canine, doing an endo on a completed calcified tooth, some crown lengthening and then it came in like this. I took and impression for a Procera Zirconium post that I cemented with Resin (after using the ErYAG laser to remove the smear layer).
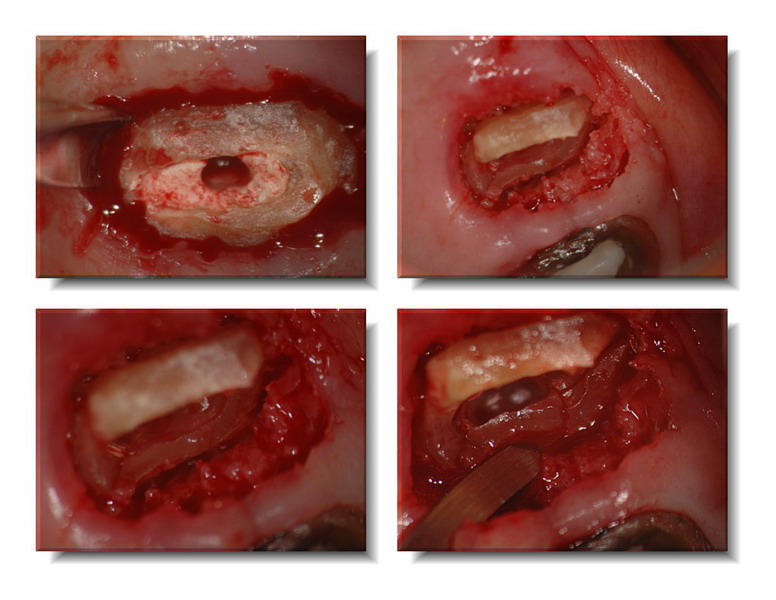
The crown on the first molar was removed (yikes) and then the 2nd premolar was extracted ala Dougs case. I used a 4oo micron tip at 25 Hz and 200 mj with H20 to create a small trough……..crack , crack , crack. A little more troughing and presto mundo, out comes the root.
Placed in some Osseograf and put a piece of gauze over the osseograf til I took the temp and relined it. Didnt want all the extraction preservation material going all over the place. Will leave the temp in for 3 months and then will do an ovate pontic on both teeth that are missing.
The temp bridge is in place……..hope its interesting.
Glenn and PS its too late and to tiring for text , so just follow along….
Boy some of the socket photos through the scope showed RIGHT down to the bottom of the socket….talk about no bleeding!!…what a cool shot. Put that in at the end for you.
glenn


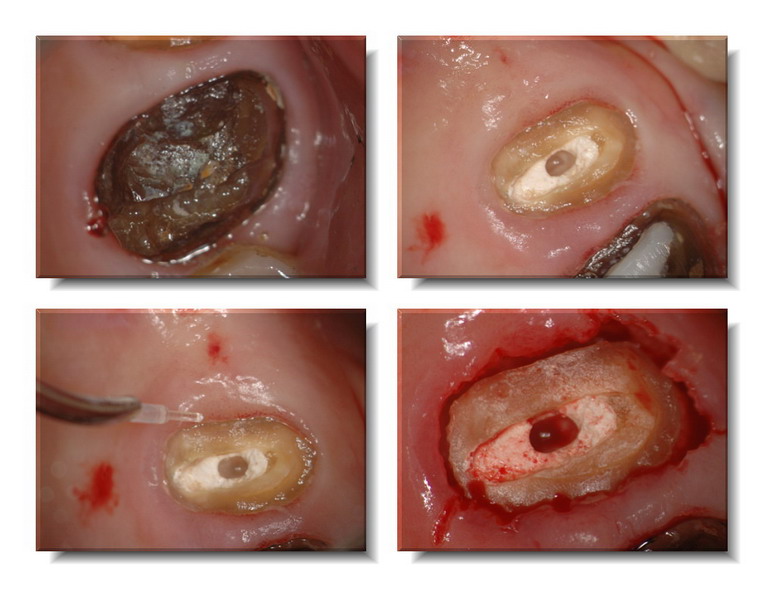
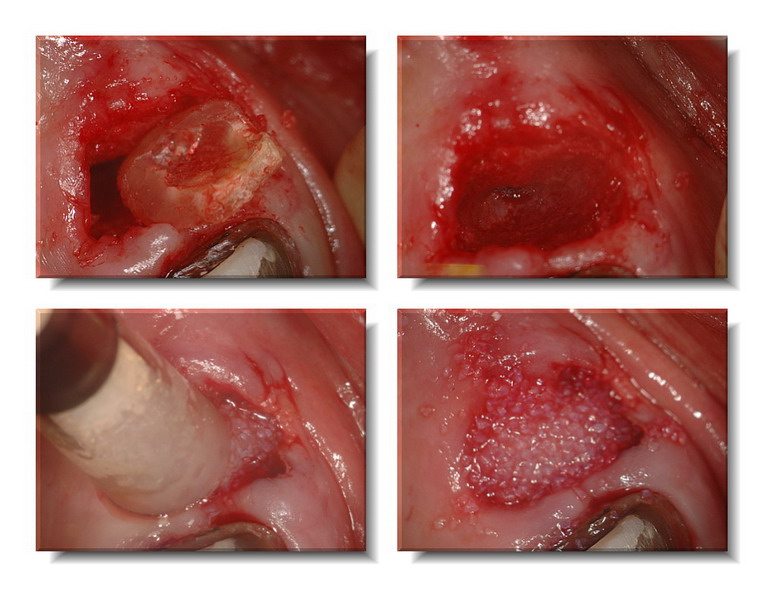

Glenn van AsSpectatorPs and here is a photo of the exo socket, sooooo coool to see to the bottom of the socket without any blood….
Glenn
[img]https://www.laserdentistryforum.com/attachments/upload/DSC_0007_resize.JPG[/img]
Glenn van AsSpectatorDid this one today before I left without anesthetic. Used TAC 20 topical with methylene Blue in it (just helps show it up a little bit better) and used the Er:YAG at 10 Hz and 40 mj with a 400 micron tip , no water but the assistant spraying a little air and water spray to keep patient comfortable. Quite a hunk of attached tissue we took off for the bracket (no photo of that as running behind).
I do this alot now when the patient is all lined up but the canines are taking their time. Watch for the attached tissue though as you must be careful to not cut all of it away……….it is a problem then that will require a graft.
Hope its interesting.
glenn
PS I used Astringident in an Ultradent syringe to get hemostasis quickly, could have used the diode too.
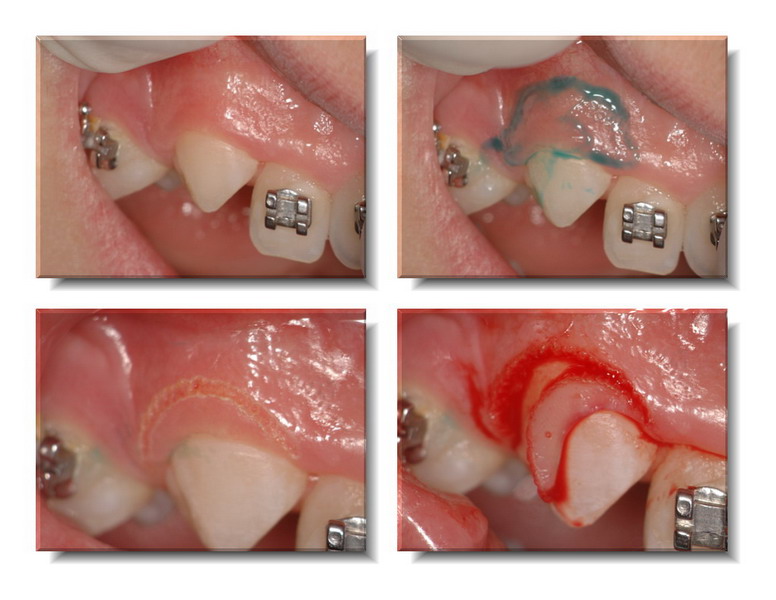
Glenn van AsSpectatorPS – check out how even at 10 Hz and 40 mj you can still get some iatrogenic notching on the enamel surface in the last photo at super high mag!!
Cya
Glenn
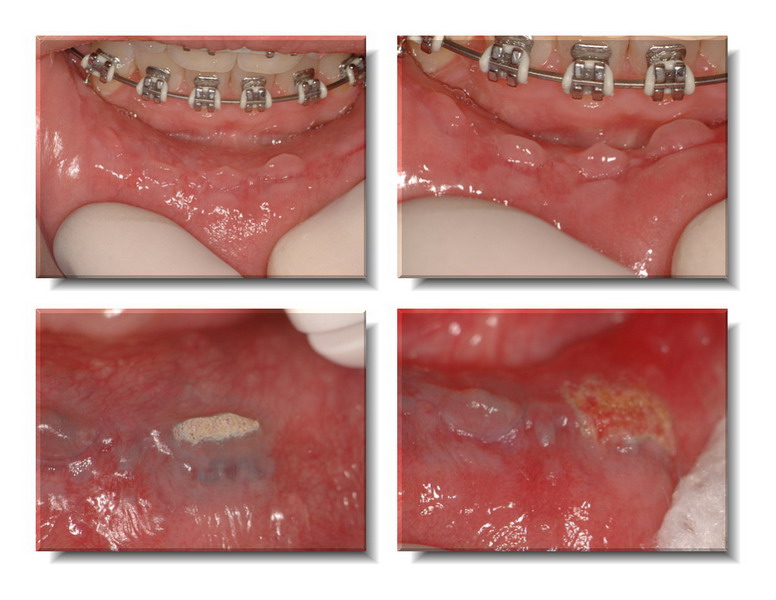
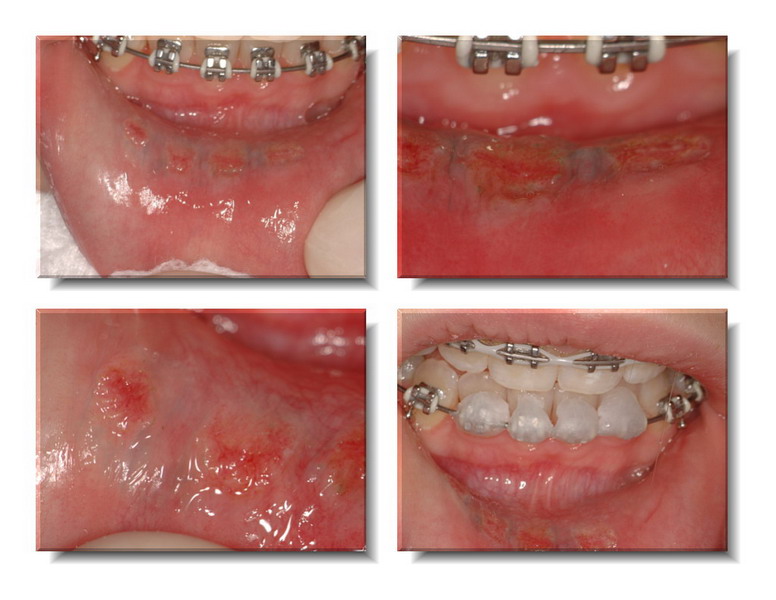
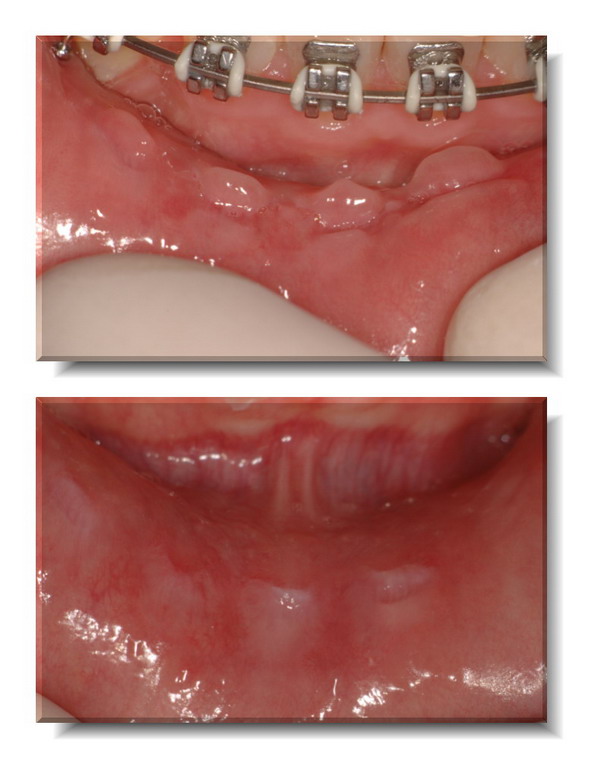
Glenn van AsSpectatorHi folks: Here is an interesting one. These are the ones that if you dont have a laser you often will be leaning towards “watching” these irritation fibromas.
They were induced by the brackets, and irritating the patient. I am scheduled in a couple of months to remove the brackets so I scheduled her to remove the tissue tags with the erbium , done without anesthetic with the chisel tip derm abrading them away. I used 10 Hz and 60-90 Hz without water on the tissue using topical only. At high mag I was able to follow the tags down til they were even.
I will post the healing photos (gotta find them first) in my next post.
Neat use of the Er:YAG laser that I hadnt seen anyone post so I thought it might be interesting.
Glenn
AnonymousSpectatorGlenn, if the guilt gets you posting this kind of stuff…I hope you stay feeling guilty. 😉
It seems like I’ve heard some debate lately about amount of bleeding and grafting. Did you stimulate a little more bleeding before placing the graft? If you hadn’t grafted would you have tried to get a little more bleeding so there would be a ‘full’ clot and good matrix for healing?
Thanks for posting.
Glenn van AsSpectatorHere is the healing photos on Day 6. There is still one area I have to go back on (whiter) but the rest is much better and softer without the tag feeling.
Glenn
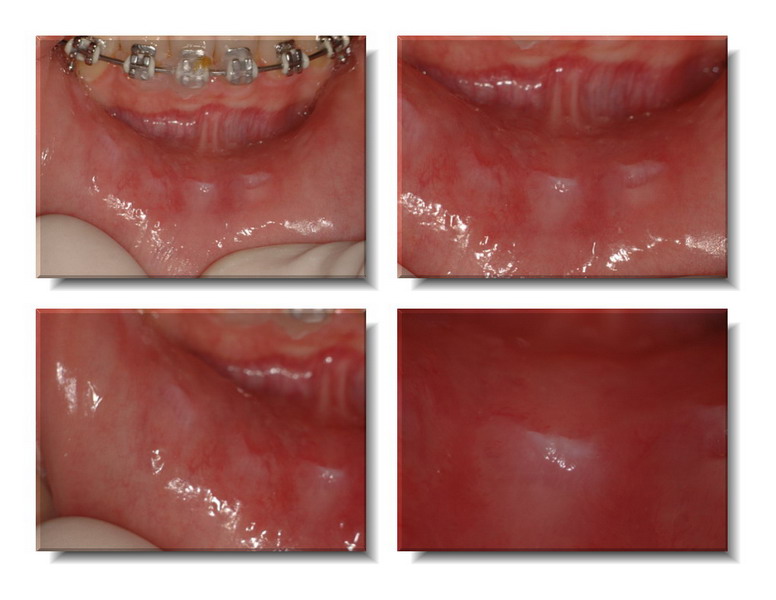
Glenn van AsSpectatorOh ya one more, before and afters at medium mag and high mag…….gotta run.
Glenn

Glenn van AsSpectatorHi there, great question Ron, there still was enough bleeding I think for the graft but that is a very good point. Look at the graft material it was pretty soaked . I didnt stimulate bleeding but I am pretty quick with the trigger finger as well on the camera (I know how to ge these types of photos ……..suction ……suction …….ok quick……….CLICK!!)
As for the other aspect, yes I thinkk that the Nd YAG induced clot is probably the way to go, I just find that the relining of the bridge causes all sorts of bleeding etc. I dont know how firm the clot is from the NdYAG and whether it will resists the pressure from the relined bridge pontic resting on it as the material sets.
This will.
Hope that answers it……..gotta run.
Tom Haney is here in 30 mins.
Glenn
PS I have more stuff I have been saving and will try to post as I get time.
Glenn
zendentistSpectatorHappy Thursday afternoon to all. Just posted this over on that other website, cracked open a cold Corona, and decided to solicit input here regarding this topic:
Going a little further down the road of the 10 hz rep rate that has been discussed recently , I wanted to share something that seems almost too good to be true. While the 10Hz rate has opened up a new door for posterior tooth prep in my hands, a few patients were still feeling some of the prep. I have noticed that patients seemed more comfortable with a 400 um tip as opposed to the 600 um tip, so I I’ve been using a 400 um tip, 10hz, 200 mj on all posterior preps with a further improvement in patient comfort, not to mention speed of ablation. The fluency here is almost exactly twice that of the 600 um tip at this pulse energy, on the order of 500J/cm2; to accomplishe the same fluency with a 600 um tip would require a 450 mj pulse energy, if my math is correct. It seems that the lower average power with the smaller tip is better able to operate below the patient’s stimulation threshold.
Hopefully this will work well for everybody else here; I use a Hoya laser, and I’m not familiar with tip selection for the WaterLase and Opus. I’d be interested in hearing other’s experiences or thoughts along this line.
Zen
February 23, 2006 at 10:04 pm in reply to: Premolar and molar protocol: Fluency vs. Average Power #6084
drnewittSpectatorHey Zen
I have found that starting with the 400 at 10hz 200+ is great for getting through the enamel but it can still get a little sensitive on some, as you know. I found switching down to 10Hz 170mj seems to eliminate the sensitivity, once I’m through the enamel.
Defiantly need to remove ablation product with etch or mechanical though as the 10hz 170-200 leaves a loose rough surface.
Thanks for the info on Fluency vs. Average Power. How did you do your math?
February 23, 2006 at 11:54 pm in reply to: Premolar and molar protocol: Fluency vs. Average Power #6085
zendentistSpectatorDr. Newitt:
My guess is that the lower average power of the 400um tip to achieve the same fluency might be a key to further lowering sensitivity rates.
As far as the math goes, apparently I don’t have a clue. Like Lynyrd Skynyrd sang (paraphrased) “I know a little ’bout (math), and baby I can guess the rest.” Halfway through my second Corona, I realized that in my intensity of converting millijoules to joules, micrometers to centimeters, and beer in liquid matter, I forgot about that pesky Pi constant. While the relative fluencies still double between when decreasing tip size form 600 to 400 um, the actual fluency values are (I think) 71.4 J/cm2 for the 600 um tip, and 153 J/cm2 for the 400 tip. That answer will probably change tomorrow. ( I thought 500 J/cm2 was rather high).
I think you were politely telling me to check my math; if not, please check mine:
200mj pulse energy = 0.2 Joules
600um = .06 cm; radius = .03cm; Pi x radius2=.0028cm2
0.2J/.0028cm2 = 71.4 Joules/cm2
similarly for the 400um tip, radius = .02cm
Pi x radius2= .0013 cm2
.02J/.0013 cm2= 153 J/cm2
Gotta run over to DT and correct my post there before one of those sharp eyed cutthroats makes further mincemeat of me.
Wes
dkimmelSpectatorDoug nice case and gald to see you posting…
Glenn — sweet.
Ron are you using the Nd:Yag in cases like this to form the clot over the graft? Seems like it would be a great way to go instead of the barrier.. I ‘ve thought about doing this a couple of times but the op is getting smaller everyday and I get lazy sometimes in bringing the Periolase into the op. That and I like to put the pontic 2-3 mm into the extration site. Without out the barrier , I’ve be afraid of disruption of the clot and graft particals going everywhere during the cementation process. Then having to go back and laser again. Not a real big deal but a time management issue..
dkimmelSpectatorGlenn that is a nice cut at 10Hz and 40mj. A lot smoother then I would have thought and no enamel ablation.
Cool blue color!!
Robert Gregg DDSSpectatorVery nice application and photo serries, Glenn!
CLAP, CLAP, CLAP!
Bob
-
AuthorPosts
