Forum Replies Created
-
AuthorPosts
-
zendentistSpectatorQUOTEQuote: from etienne on 12:58 pm on April 17, 2006
Hi Guys
I have been using the Deka Smart 2940D+ Er:YAG laser for a few months now. Most patients complain about sensitivity and have to be numbed. Even when I turn the pulse energy down as far as 50-100mJ with 5-10Hz the patients still experience pain. I am using the shortest pulse duration available, starting out in defocussed mode with maximum waterflow and they still complain. I have been in dentistry long enough to be able to tell when patients are just being difficult but am convinced that these people are more than uncomfortable during treatment.Even for something as small as these lesions I need to use local anesthetic.

Any suggestions?
Thanks!
EtienneEtienne: I’ll chime in here with another thought. I don’t know the laser you’re using very well, but you did mention that you’re using “the shortest pulse duration available”, so I’m guessing your laser allows you to vary the pulse duration. Dan you tell us what the range of pulse durations are? Generally, shorter pulse durations are associated with increase sensitivity due to the higher peak pulse powers.
I treat these occlusal cupolas frequently, but my delivery system is significantly different on my Hoya unit, so quoting my settings won’t help much, but generally more water, lower pulse energy (mj), and lower hz translates to less sensitivity.
etienneSpectatorHi Guys
I first posted this case in Sept 2005 when this aptient visited me from out of town.This was the initial situation on tooth# 31:
size.jpg)
I took a digital pa at the time:

I treated the patient by placing a splint, using the Nd:YAG in the sulcus and adjusting the occlusion as per the advice given at the time. I saw the patient again today.

The soft tissue surrounding #31 looks good. The furcation lesion is clinically evident. The tooth went from class 3 mobility to class 1. My gut feel is that the tooth is cracked bucco-lingually. There is a visible crack, how deep it is I don’t know.
What do you see on the x-rays and where do I go from here?
Thanks very much
Etienne
etienneSpectatorSame case, tooth nuber 8. Initial situation:


I completed endo on both #8 and #9 and splinted them.

This is the current situation:
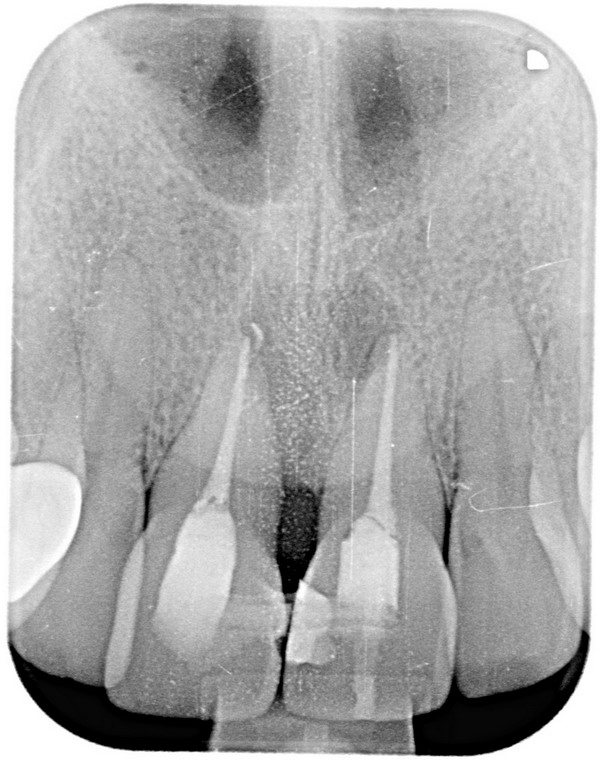
The tooth is stable because of the splint but there is still puss draining from the mesial side of #8. Vertical root fracture? There is no pain or discomfort at all.
Any advice?
Take care
Etienne
kmarshallSpectatorthis could be perio-endo. You treated the endo (great job; love the fill of the two accessory canals) now treat the perio. Hope it works out.
Keith
kmarshallSpectatorGreat result. Do you use the laser with the canal dry? How long? Past the apex?
Thanks.
etienneSpectatorHi K
Thanks for the compliment.Yes, use the Nd:YAG in a dry canal although the laser will have a drying effect on the canal as well. You will actually hear the laser going “click” if the canal is dry.
Protocol is approx 20sec per canal while withdrawing the fiber, repeated 5 times per canal.
Take care
Etienne
etienneSpectatorHi K
Thanks. My initial thought was endo-perio, which is why I did the endo. I am concerned about the fact that there is still drainage from beside the root although there seems to be more bone than at the beginning!
Take care
Etienne
Robert Gregg DDSSpectatorEtienne,
My preference is to use the laser as a heat source as well and use NaOCL and/or RC Prep to help dissolve the smear layer, pump the bleach into laeral canals and tubules. The wavelength and parameters will be effective alone in disinfecting the pathogens, but the bleach will give it an extra effect, I think.
Bob
etienneSpectatorHi Bob
Thanks, interesting thoughts. I would love to see the results if somebody did a study on it.I damaged the fiber on my laser and am waiting for a new one. I almost feel ashamed everytime I seal a canal while not having the laser in action!
Take care
Etienne
Robert Gregg DDSSpectatorActually, Leo Messerindino did a study back in 1990 using an FRP Nd:YAG (150 usec) and bleach using the old dLase 300.
Results were 99.9% elimination of CFU’s with laser and bleach while either alone was only 90% reduction.
Bob
etienneSpectatorHi Guys
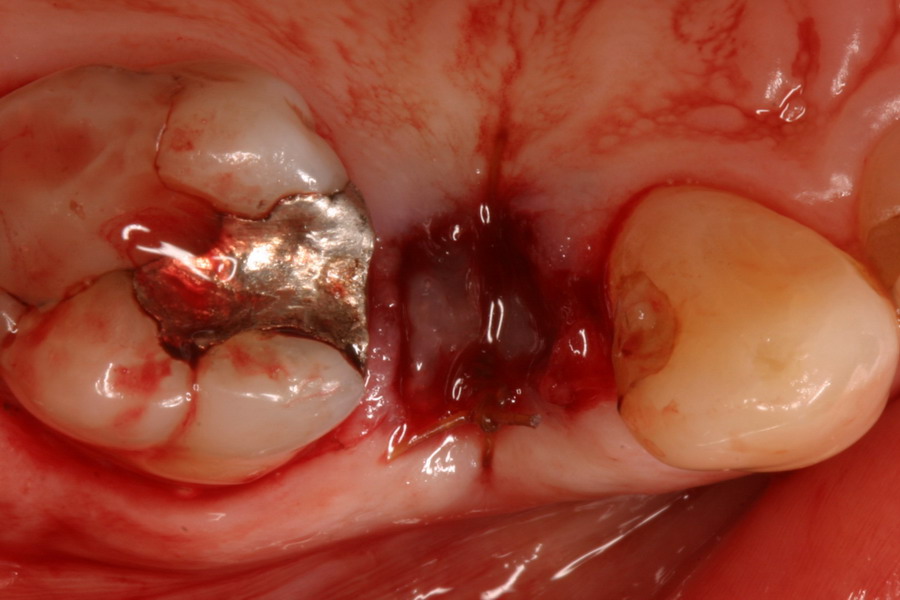
I did not think that this warranted another thread. Here is a case that I did today with laser and PRP, just as a matter of interest.This what the product look like.
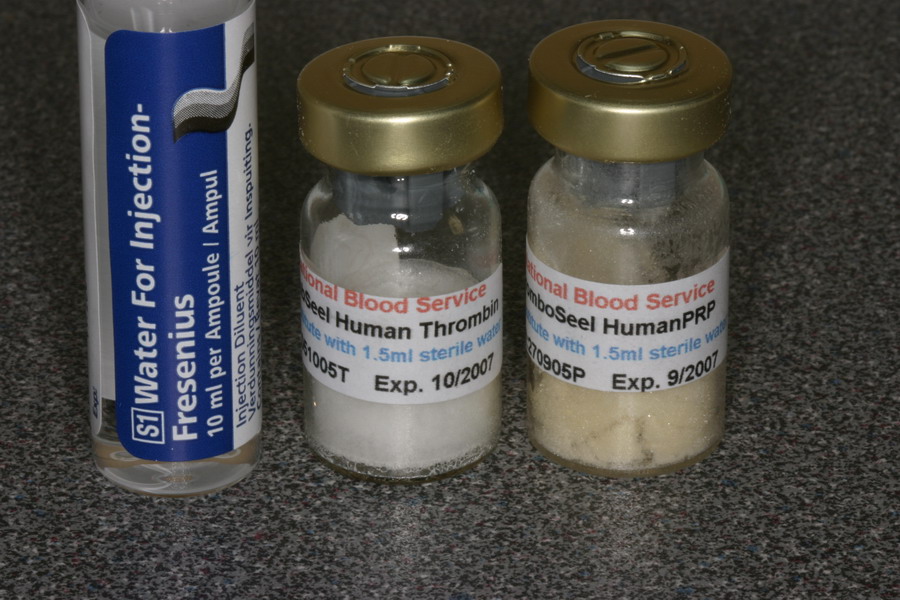
This was the case before I started.

After the root was removed I used the Nd:YAG inside the socket.
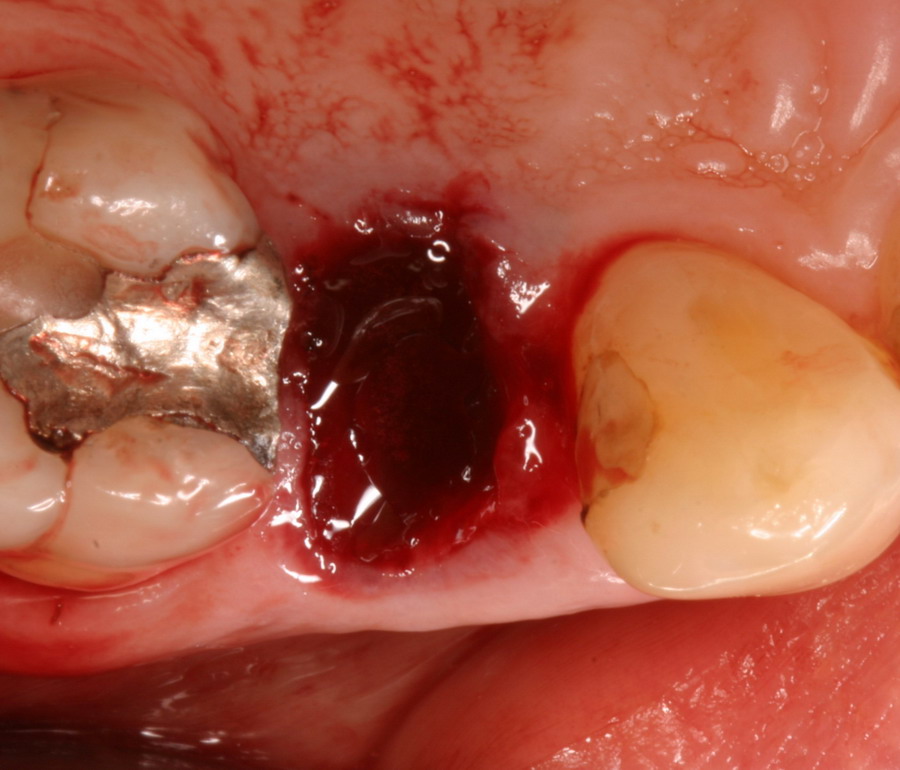
This what the clotted PRP and Thrombin looked like.

Here is the socket augmented with the clotted PRP and stabilized with a suture.
Any thoughts appreciated.
Take care
Etienne
etienneSpectatorHi Bob
Thanks very much, I wasn’t aware of it. Do you know where I can get a copy of the article? I looked on Pubmed without success.
Take care
Etienne
dkimmelSpectator
Anyone else read this review??
DAvid
whitertthSpectatorOf course i did…interesting stuff..I have been speaking with Bob about it…I will let him comment on this…but interesting enough no Yukna mention…….;….
arrowsmithSpectatoretienne,
The previous case with #8 being lost, adding a graft, and then placing the implant . . . . how long did you wait until placing the implant after the extraction and grafting? Maybe I’m wrong, but it looks like around a month . . . . do you think the buccal bone is stable enough? Did you reflect a flap during the placement of the implant? What size implant did you use?
Bob, there is a lot of discussion about atraumatic extractions preserving the bone height/levels. Is there any connection with using the Periolase to disinfect/clean the extraction site, and maintaining even more bone, long term?
aaroN
-
AuthorPosts
